The EGSYS score uses clinical variables to predict which patients may have cardiac (CS) or non-cardiac syncope (NCS). It has been validated in the emergency department context. This study aims to determine whether the score has the same applicability in an outpatient setting.
MethodsIn this retrospective study of all patients observed in the outpatient setting of a hospital with a syncope unit between January 2015 and December 2016, the EGSYS score was calculated for each patient, and its sensitivity and specificity were determined for the prediction of CS in patients with score ≥3.
ResultsA total of 224 patients, mean age 64.3±21.7 years, 116 (51.8%) male, were analyzed. In the 163 (72.7%) patients with confirmed syncope, CS was diagnosed in 27 (16.6%) and NCS in 136 (83.4%). The EGSYS score was ≥3 in 40 (20.0%) patients with NCS and in 13 (48.1%) with CS. A positive score had a sensitivity of 48.2% (95% CI: 28.7-68.1), a specificity of 77.9% (95% CI: 70.0-84.6), and a positive and negative predictive value of 30.2% (95% CI: 20.8-41.8) and 88.3% (95% CI: 83.9-91.7), respectively.
ConclusionThe EGSYS score has limited usefulness in an outpatient setting, where observed patients have already been been medically assessed. Given its high specificity and negative predictive value, it may be useful to reassure low-risk patients and family members.
O score EGSYS para avaliação do doente com síncope em contexto de urgência utiliza variáveis de ordem clínica e foi validado para diferenciar entre síncope de etiologia cardíaca (SC) ou não cardíaca (SNC). Este trabalho pretende determinar se o score tem a mesma aplicabilidade no contexto de consulta.
MétodosEstudo retrospetivo a partir dos registos eletrónicos dos doentes observados em consulta externa de síncope entre janeiro de 2015 e dezembro de 2016. Foi calculado o score EGSYS para cada doente e determinada a sensibilidade e especificidade para a predição de etiologia cardíaca em doentes com score 3.
ResultadosForam avaliados 224 doentes, com média de 64,3 ± 21,7 anos, 116 (51,8%) eram do sexo masculino. Nos 163 (72,7%) com síncope confirmada, o diagnóstico foi de SC em 27 (16,6%) e SNC em 136 (83,4%). O score EGSYS foi 3 em 40 (20,0%) doentes com SNC e em 13 (48,1%) com SC. Um score 3 teve uma sensibilidade de 48,2% (IC 95%: 28,7-68,1), uma especificidade de 77,9% (CI 95%: 70,0-84,6), um valor preditivo positivo e negativo de 30,2% (CI 95%: 20,8 – 41,8) e 88,3% (CI 95: 83,9 – 91,7) respetivamente.
ConclusãoO score EGSYS tem utilidade limitada no contexto de consulta de síncope, que recebe doentes filtrados por avaliação médica prévia. Dada a sua elevada especificidade e valor preditivo negativo, poderá ter utilidade como tranquilizador do doente e parentes no contexto clínico apropriado.
Syncope is defined as a transient loss of consciousness and postural tone due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery.1 It is a symptom with a wide range of possible causes, ranging from benign to potentially fatal.2 These can in general be divided into cardiac and non-cardiac causes, the former of which are associated with higher mortality, irrespective of age.3 Syncope accounts for 1-5% of emergency department (ED) admissions,1,4,5 but only 1-6% of patients with syncope go to the ED.4,6,7
Initial assessment of a patient with syncope thus has two main aims: to exclude a possible cardiac cause, and to determine the risk for future adverse events.8 In the diagnostic approach to these patients, a thorough investigation is essential, including clinical history, careful characterization of syncopal episodes, and assessment of the findings of the physical examination and 12-lead electrocardiogram (ECG).9,10 Even so, several studies have shown that the initial assessment only provides a definitive diagnosis in 20-50% of cases.9,11,12 Accordingly, various risk scores have been developed and validated for initial triage in syncope, aiming to identify patients at greatest risk of a cardiac etiology and adverse events.8,13–16
The Evaluation of Guidelines In Syncope Study (EGSYS) score, which is based on clinical and electrocardiographic variables, was developed in order to identify patients presenting to the ED with syncope who are likely to have a cardiac cause. It uses six variables: palpitations preceding syncope (+4 points); heart disease or abnormal ECG, or both (+3 points); syncope during effort (+3 points); syncope while supine (+2 points); autonomic prodromes (-1 point); and precipitating or predisposing factors, or both (-1 point).8 The score was developed and validated for use in the ED in order to identify patients at greater risk of adverse events who would benefit from hospitalization and more comprehensive etiological investigation. A score of ≥3 has sensitivity of 92% and specificity of 69% for diagnosing cardiac syncope, and has a strong association with prognosis, predicting low mortality among patients with EGSYS score <3.8,17,18
However, its validity in an outpatient setting has not been tested, hence its applicability in this situation is unclear. The present study aims to assess the diagnostic accuracy of the EGSYS score in outpatient consultations in a hospital with a syncope unit to which patients with syncope of uncertain etiology are referred.
MethodsWe carried out a retrospective descriptive correlational study including all patients observed at their first consultation in our hospital's syncope unit between January 1, 2015 and December 31, 2016. Patients with syncope were identified and its etiology was determined. The EGSYS score was calculated and its ability to predict a cardiac cause was assessed.
In each consultation an electronic record was made of the patient's baseline characteristics, personal history, characteristics of episodes of loss of consciousness, prodromal and recovery symptoms, predisposing factors, physical examination, and 12-lead ECG. Syncope was defined in accordance with the European Society of Cardiology guidelines.1 Cardiac disease was defined as the presence of one of the following: previous history or clinical diagnosis of any form of structural heart disease, including ischemic heart disease, valve dysfunction, cardiomyopathy or congenital heart disease; previous diagnosis or clinical evidence of congestive heart failure; or physical signs of structural heart disease. The ECG was defined as abnormal with sinus bradycardia <40 bpm, higher than first-degree atrioventricular (AV) block, complete bundle branch block, pathological Q waves, supraventricular or ventricular tachycardia, left or right ventricular hypertrophy, ventricular pre-excitation, long QT interval, or Brugada pattern.
Patients were assessed according to a previously published protocol.19 In addition, patients with symptoms associated with exertion underwent exercise testing, and those with suspected iatrogenic hypotension underwent ambulatory blood pressure monitoring. Patients with suspected neurocardiogenic syncope were referred to the neurology department, where they underwent additional tests at the discretion of the neurologist (electroencephalogram, brain magnetic resonance imaging, or brain computed tomography). Cardiac syncope of mechanical cause was diagnosed in the presence of severe valve stenosis or other forms of flow obstruction. A diagnosis of arrhythmic syncope was made in the following circumstances: documented syncope or prodromal symptoms coinciding with a period of sinus bradycardia <40 bpm or sinus pause of >3 s on the ECG, a period of Mobitz I second-degree AV block or of supraventricular tachycardia, a period of Mobitz II second-degree or third-degree AV block, alternating bundle branch block, or pacemaker dysfunction with pauses or periods of paroxysmal ventricular tachycardia.
Statistical analysisA descriptive statistical analysis was carried out to characterize the profile of the study population. Continuous variables are presented as mean and standard deviation and categorical variables are expressed as count and percentage. The chi-square test was used to identify associations between each of the variables and a cardiac cause of syncope.
The EGSYS score was calculated for each patient and the population was divided into two groups: those with EGSYS <3 and those with EGSYS ≥3. The existence of a statistical association between each variable and the cause of syncope was assessed within each group by means of the Student's t test for continuous variables. The score's sensitivity, specificity, and positive and negative predictive value in the study population were determined and its predictive value was tested by receiver operating characteristic (ROC) curve analysis.
Two-year follow-up was performed via telephone contact by a cardiologist to determine mortality, which was compared between the two groups, and survival was assessed by the Kaplan-Meier method.
The level of significance was set at 95% for a p-value of <0.05. The statistical analysis was carried out using IBM SPSS version 24.0.
ResultsA total of 248 patients were observed at their first consultation during the study period, of whom 24 (9.7%) were excluded due to lack of sufficient data to calculate the EGSYS score. Of the remaining 224 subjects, 116 (51.8%) were male and mean age was 64.7±21.4 years (Table 1). Regarding cardiovascular risk factors, 140 (62.5%) were hypertensive, 101 (45.1%) had dyslipidemia, 42 (18.8%) had diabetes and 17 (7.6%) were active smokers. Structural heart disease was observed in 36 (18.1%) and 56 (25.0%) had an abnormal ECG. More than one episode of syncope was reported by 125 (55.8%) patients, presyncope without loss of consciousness by 36 (16.1%), syncope without prodrome by 46 (20.5%), and some form of trauma by 45 (20.1%).
Characteristics of the study population (n=224).
| Male gender | 116 (51.8%) |
| Age, years | 64.7±21.4 |
| Hypertension | 140 (62.5%) |
| Dyslipidemia | 101 (45.1%) |
| Diabetes | 42 (18.8%) |
| Smoking | 17 (7.6%) |
| Structural heart disease | 36 (16.1%) |
| Abnormal electrocardiogram | 56 (25.0%) |
| Recurrent syncope | 125 (55.8%) |
| Presyncope | 36 (16.1%) |
| No prodrome | 46 (20.5%) |
| Trauma | 45 (20.1%) |
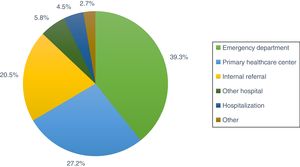
Referral to the syncope unit was from the ED in 39.3% of cases, from primary healthcare centers in 27.2% and internally from another department in 20.5% (Figure 1).
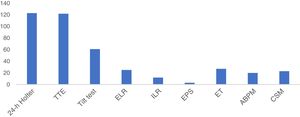
With regard to the diagnostic exams performed, 123 (54.9%) patients underwent 24-hour Holter monitoring, 122 (54.5%) transthoracic echocardiography, 61 (27.2%) tilt testing, 27 (12.1%) exercise testing, 25 (11.2%) external loop recorder monitoring, 23 (10.3%) carotid sinus massage, 20 (8.9%) ambulatory blood pressure monitoring, 12 (5.4%) implantable loop recorder monitoring, and three (1.3%) electrophysiological study (Figure 2).
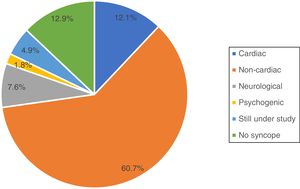
Of the total of 224 patients analyzed, 163 (72.8%) in fact had syncope, which was of cardiac cause in 27 (12.1%) of cases and non-cardiac cause in 136 (60.7%) (Figure 3). Of the remaining patients, 17 (7.9%) had suffered loss of consciousness of neurological cause and four (4.9%) of psychogenic cause, 11 (4.9%) were still under study with an implantable loop recorder, and in 29 (12.9%) cases it was established that there had in fact been no loss of consciousness.
The EGSYS score was calculated for the 163 patients who had suffered syncope. Of these, 120 (73.6%) had EGSYS <3 and 43 (19.2%) had EGSYS ≥3. Among those with EGSYS <3, the mean score was -0.2±1.1, compared to 3.7±1.3 in those with EGSYS ≥3 (p<0.001) (Table 2).
Comparison between patients with negative and positive EGSYS score.
| EGSYS <3 (n=120) | EGSYS ≥3 (n=43) | p | |
|---|---|---|---|
| Mean EGSYS score | −0.2±1.1 | 3.7±1.3 | <0.001 |
| Abnormal ECG or heart disease | 19 (15.8%) | 28 (65.1%) | <0.001 |
| Palpitations | 0 (0%) | 15 (34.9%) | <0.001 |
| Syncope during exertion | 0 (0%) | 5 (11.6%) | <0.001 |
| Syncope while supine | 3 (2.5%) | 2 (4.7%) | 0.483 |
| Autonomic prodromes | 17 (14.2%) | 2 (4.7%) | 0.095 |
| Precipitating factors | 60 (50%) | 2 (4.7%) | <0.001 |
| Cardiac cause | 14 (11.7%) | 13 (30.2%) | 0.005 |
| Tachyarrhythmia | 3 (2.5%) | 3 (7.0%) | 0.181 |
| Bradyarrhythmia | 10 (8.3%) | 8 (18.6%) | 0.065 |
| Structural | 1 (0.8%) | 2 (4.7%) | 0.11 |
| Non-cardiac | 106 (88.3%) | 30 (69.8%) | 0.005 |
| Reflex | 42 (35.0%) | 16 (37.2%) | 0.795 |
| Situational | 22 (18.3%) | 4 (9.3%) | 0.795 |
| Hypotension | 25 (20.8%) | 6 (14.0%) | 0.324 |
| Orthostatic hypotension | 12 (10.0%) | 2 (4.7%) | 0.283 |
| Dysautonomia | 2 (1.7%) | 2 (4.7%) | 0.278 |
| CSH | 3 (2.5%) | 0 (0%) | 0.295 |
| Died | 11 (9.2%) | 4 (9.3%) | 0.979 |
CSH: carotid sinus hypersensitivity; ECG: electrocardiogram.
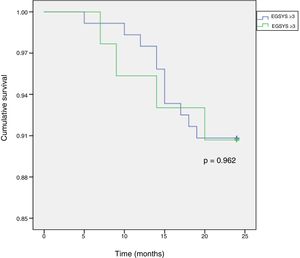
The score was significantly higher in patients with syncope of cardiac cause (1.85±2.3 vs. 0.64±2.0, p=0.005) and was more often positive in these patients (30.2% vs. 11.7%, p=0.005) (Table 3). There were no significant differences between the groups in terms of the individual causes of cardiac or non-cardiac syncope, or in mortality (9.2% vs. 9.5%, p=0.945) (Figure 4).
Comparison of elements of the EGSYS score between patients with cardiac and non-cardiac syncope.
| Individual elements of the EGSYS score | Cardiac syncope (n=27) | Non-cardiac syncope (n=136) | p |
|---|---|---|---|
| Mean EGSYS score | 1.85±2.3 | 0.64±2.0 | 0.005 |
| Abnormal ECG or heart disease | 12 (44.4%) | 35 (27.5%) | 0.05 |
| Palpitations | 3 (11.1%) | 12 (8.8%) | 0.707 |
| Syncope during exertion | 2 (7.4%) | 3 (2.2%) | 0.152 |
| Syncope while supine | 2 (7.4%) | 3 (2.2%) | 0.152 |
| Autonomic prodromes | 2 (7.4%) | 17 (12.5%) | 0.451 |
| Precipitating factors | 4 (14.8%) | 58 (42.6%) | 0.007 |
ECG: electrocardiogram.
In terms of the individual parameters of the EGSYS score, abnormal ECG or heart disease was significantly more common in patients with syncope of cardiac cause (44.4% vs. 25.7%, p=0.05), while precipitating factors were significantly less common (14.8% vs. 42.6%, p=0.007). No significant differences were seen between the two groups in the other parameters (Table 3).
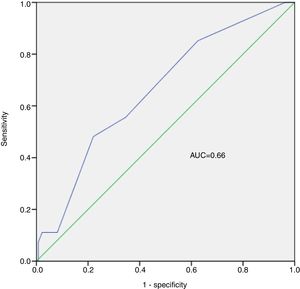
An EGSYS score ≥3 had sensitivity of 48.2% (95% confidence interval [CI]: 28.7%-68.1%), specificity of 77.9% (95% CI: 70.0%-84.6%), positive predictive value of 30.23% (95% CI: 20.8%-41.8%), negative predictive value of 88.3% (95% CI: 83.9%-91.7%), and diagnostic accuracy of 73.0% (95% CI: 65.5%-79.7%), to predict a cardiac cause (Table 4). The predictive ability of the EGSYS score in our population was low, with an area under the ROC curve of 0.66 (Figure 5).
Our syncope unit is an outpatient clinic that is part of the hospital's outpatient service to which patients are sent if they have had syncope of uncertain etiology following initial investigation by the referring physician. Most referrals are from the ED or primary healthcare centers. Patients with syncope of documented cardiac origin who have been referred for treatment are therefore not observed in this unit.
Participants in this study underwent assessment by a cardiologist that included a comprehensive history, physical examination and 12-lead ECG. The subsequent assessment process followed the protocol published by Sousa et al.19 In our study, the most frequently requested diagnostic exams were 24-hour Holter, transthoracic echocardiography, tilt testing, and external loop recorder monitoring. When loss of consciousness was suspected to be due to a neurological cause, the patient was referred to a neurologist and the appropriate diagnostic exams were requested. Using this methodology, a final diagnosis was obtained in 95% of patients during the study period. A cardiac cause was identified in 12.9% of cases, which is in line with the rates found in other studies.1,2,19–23
The usefulness of characterizing syncopal episodes by clinical history, physical examination and ECG for predicting their etiology and the risk of adverse events has been assessed in various studies.8,18,24 Several scores have been developed or proposed for this purpose. One of them, EGSYS, was created to meet the need to triage patients with recent syncope in the ED, in order to identify those with a high probability of a cardiac cause and thus to reduce the number of unnecessary hospitalizations.8 Follow-up at one month and two years showed higher mortality in patients with higher scores,18 and the score appears to have sensitivity for predicting mortality and adverse events of 80% and 56%, respectively.25
However, the validity of the EGSYS score in an outpatient setting for patients with previous syncopal episodes that have not been investigated has not been established. On the basis of the present study, an EGSYS score ≥3 has low sensitivity for predicting the cause of syncope in an outpatient setting, although its specificity is acceptable. The mean EGSYS score in patients with cardiac syncope was significantly higher (almost three-fold) than in non-cardiac syncope. Its negative predictive value was also high, which could make it a useful indicator of a low probability of a cardiac cause, identifying cases with less need for follow-up visits and diagnostic exams. However, its area under the curve was 0.66, which indicates a poor ability to predict a cardiac cause of syncope.
Among the score's parameters, the presence of heart disease has been identified as the most sensitive for a cardiac cause,23,26 although a significant proportion of patients with heart disease have neurocardiogenic syncope.8 In our population, the parameters with the closest association with the final diagnosis were abnormal ECG or heart disease and precipitating factors for syncope.
The two-year mortality of 9.2% found in our sample is comparable to that of the general population in other studies.8,18 However, unlike in these studies, in our analysis the EGSYS score was unable to identify patients at higher risk of adverse events. This may be due to differences in population characteristics, as ours was assessed in the outpatient setting and excluded patients already diagnosed in the ED or in primary healthcare.
This work has certain limitations. It was a retrospective study on a small sample. It was based on electronic records entered during the consultation, which may have been subject to coding errors. In addition, the population was selected, consisting only of patients referred to our unit due to syncope that was still of uncertain etiology after a previous medical assessment.
ConclusionThe EGSYS score is simple to calculate, being based on clinical history, physical examination and ECG, and has a high negative predictive value for syncope of cardiac cause in an outpatient setting. It may thus be useful to identify patients who do not need a more comprehensive investigation. The other information it provides appears to have limited usefulness in this setting.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: de Sousa Bispo J, Azevedo P, Mota T, et al. Score EGSYS para predição de etiologia cardíaca na síncope: tem utilidade no contexto de consulta? Rev Port Cardiol. 2020;39:255–262.