Valvular aortic stenosis is the most common valvular disorder in Europe. Although recommended, stress exams are still underused in its evaluation. We report the case of a 60-year-old man who, following a routine electrocardiogram with abnormal ventricular repolarization, underwent stress testing, which was positive for myocardial ischemia, and an echocardiogram that revealed moderate aortic stenosis. Cardiac catheterization showed no angiographic coronary lesions and an intraventricular gradient of 45mmHg. In view of the latter, stress echocardiography was performed, which documented an increase in the intraventricular gradient from 30mmHg to 131mmHg. Repeated stress echocardiography under treatment with bisoprolol showed an increase in test duration and a maximum intraventricular gradient at peak exercise of 36mmHg. Stress exams may have an important role in the diagnostic and therapeutic management of patients with aortic stenosis.
A estenose aórtica constitui a valvulopatia mais frequente na Europa. Embora recomendada, a realização de exames de esforço continua a ser pouco utilizada na sua avaliação. Doente do sexo masculino, de 60 anos, que na sequência de um eletrocardiograma de rotina com alterações da repolarização ventricular realiza prova de esforço positiva para isquémia do miocárdio e ecocardiograma que revelou estenose aórtica moderada. O cateterismo cardíaco revelou coronárias sem lesões angiograficamente aparentes e presença de gradiente intraventricular de 45mmHg. Perante a presença de gradiente intraventricular realizou ecocardiograma de esforço que documentou aumento do gradiente intraventricular de 30mmHg para 131mmHg. Repetiu ecocardiograma de esforço sob terapêutica com bisoprolol verificando-se um aumento do tempo do esforço e um gradiente intraventricular máximo no pico de esforço de 36mmHg. Os exames de esforço podem ter um papel importante na abordagem diagnóstica e terapêutica dos doentes com estenose aórtica.
Valvular aortic stenosis (VAS) is the most common valvular disorder in Europe, with an estimated prevalence of 2–7% in those aged over 65 years. Valve replacement surgery is the treatment of choice for severe symptomatic VAS, and is associated with low mortality.1
While the management of symptomatic patients is clearly defined in the latest European Society of Cardiology (ESC) guidelines,1 there is still considerable disagreement concerning asymptomatic VAS. In such cases, closely monitored stress testing can be useful by triggering symptoms and thus aid prognostic stratification. However, despite being recommended in the evaluation of asymptomatic VAS, stress testing is still underused in clinical practice; data from the Euro Heart Survey show that only 5.7% of these patients undergo such tests.2
Stress echocardiography is a dynamic and reproducible exam that reflects patients’ daily activities and can thus provide important prognostic information that is useful in deciding the best therapeutic approach and in revealing other possible etiologies of patients’ symptoms.3
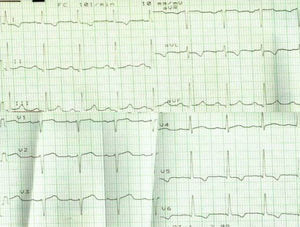
Case reportWe report the case of a 60-year-old man with a history of dyslipidemia, asymptomatic, who following a routine consultation with his family doctor was referred for an electrocardiogram (ECG) which showed sinus rhythm at 95bpm, poor R-wave progression in V1–V3 and abnormal ventricular repolarization with negative T waves in V5–V6, DI and aVL (Figure 1). No other significant alterations were observed.
The patient then underwent stress testing, interrupted after 5min due to asymptomatic ST-segment depression of approximately 2mm in V5–V6. M-mode, two-dimensional and Doppler echocardiography revealed an undilated left ventricle (LV) with concentric wall hypertrophy (septum 13mm, posterior wall 11mm), a calcified aortic valve with restricted opening and a peak aortic valve gradient of 73mmHg and mean of 34mmHg.
In view of these findings, the patient was referred for a cardiology consultation.
At the consultation, the patient was asymptomatic; physical examination revealed blood pressure of 136/78mmHg at rest, heart rate of 85bpm and a grade III/VI aortic ejection murmur radiating to the carotid arteries.
Given stress testing is positive for myocardial ischemia in an asymptomatic patient with moderate VAS, it was decided to perform myocardial perfusion scintigraphy, which revealed LV dilatation following exercise and no myocardial perfusion defects.
A year later, the patient began to experience dyspnea on moderate exertion, without angina. Cardiac catheterization (Figure 2) revealed no angiographically significant lesions, increased LV end-diastolic pressure (20mmHg), an aortic valve gradient of 20mmHg (Figure 2A), and an intraventricular gradient of 40mmHg between the chamber of the LV and the LV outflow tract (Figure 2B).
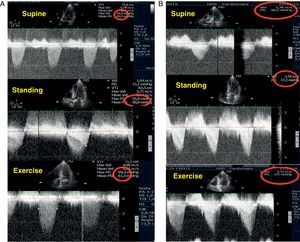
Since the patient's exertional dyspnea was worsening, he was referred for exercise stress echocardiography using the modified Bruce protocol. Echocardiographic images were recorded first with the patient supine, then standing and during exercise (Figure 3). The test was halted after 9min due to fatigue, the patient having attained a maximum heart rate of 160bpm. The following changes from the baseline echocardiogram were seen at peak exercise:
- -
increase in mean aortic valve gradient from 40.3 to 61.3mmHg (Figure 3A);
- -
increase in intraventricular gradient from 30 to 131mmHg (Figure 3B).
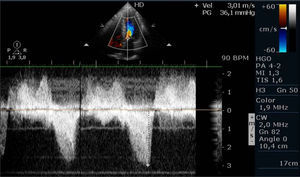
In view of the significant intraventricular gradient, the patient was medicated with bisoprolol 10mg/day, and improvement was seen in exertional dyspnea. Stress echocardiography was repeated under beta-blocker therapy following the same protocol; the test was interrupted after 14min due to fatigue, the maximum heart rate attained being 132bpm. The echocardiogram showed a maximum intraventricular gradient of 36mmHg at peak exercise, only 6mmHg more than when supine (Figure 4) and only a 16mmHg increase in mean aortic gradient. After two years of follow-up following this evaluation the patient was still asymptomatic. The approach adopted was based on the rise of only 16mmHg in aortic gradient under beta-blocker therapy.
DiscussionVAS is the most common valvular disorder in Europe and its prevalence increases with age. Its clinical presentation is often dominated by subjective symptoms such as dyspnea, and thus assessment should include complementary exams, particularly echocardiography, which is the best method of confirming clinical suspicion and of assessing the severity of valve disease and prognosis.1
At present, the only permanent treatment for symptomatic VAS is valve replacement surgery, but there is still disagreement concerning the management of patients with asymptomatic VAS, especially with regard to the best timing for surgery. Stress testing is strongly recommended by the ESC in such cases, but it is still underused.2,3
Stress testing can trigger symptoms in a third of previously asymptomatic patients and thus identify those at greater risk for cardiac events. In an analysis of 69 consecutive patients with severe VAS, Lancellotti et al.4 found that stress echocardiography identified three independent predictors of cardiac events: an increase of ≥18mmHg in mean aortic gradient; an abnormal response to exercise (defined as angina, dyspnea, ST-segment depression of ≥2mm; or a fall or <20mmHg rise in systolic arterial pressure); and an aortic valve area of <0.75cm2. A normal stress test is associated with excellent one-year prognosis. In the case presented, the mean aortic valve gradient rose by 21mmHg with exercise, although according to Picano et al.2 further prospective studies are needed to assess whether such an increase constitutes an indication for elective surgical valve replacement.
Given the diagnostic and prognostic value of stress tests in assessment of VAS, Piérard and Lancellotti recommend that they be used routinely in these patients, preferably by treadmill or cycle ergometer exercise.3
In our patient, initially asymptomatic but with an intraventricular gradient detected on cardiac catheterization, stress echocardiography using the method recommended by Piérard and Lancellotti revealed a significant increase of around 100mmHg in this gradient on exercise.
The prevalence of subvalvular intraventricular gradients in patients with VAS is estimated at 48% by Laskey et al.5 The same authors found that stress testing led to increased intraventricular gradients and that this increase was inversely related to cardiac output.5
Beta-blockers are traditionally contraindicated in VAS. However, their use in our patient led to improvement in symptoms, improved functional capacity reflected in an increase in test duration during stress echocardiography, and a significant reduction in the intraventricular gradient during exercise. This apparent paradox is explained by Cotrim et al., who assessed the efficacy of beta-blockers in symptomatic athletes with exercise-induced intraventricular gradients and observed a reduction in the gradient and improvement in symptoms when they repeated stress echocardiography under beta-blocker therapy.6
The present case highlights the importance of stress exams in assessing patients with valve disease, by revealing other possible causes of symptoms and guiding the therapeutic approach.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cordeiro Piçarra B, et al. Dispneia na estenose aórtica: nem tudo o que parece é. doi:10.1016/j.repc.2011.06.001.