Echocardiography is the most widely used imaging technique in modern cardiological clinical practice, since it is readily available, portable and safe, and provides a comprehensive morphological and functional assessment at low cost compared to other imaging modalities. Recent technological advances have introduced new echocardiographic techniques and widened the clinical applications of echocardiography. However, these developments have also led to an increase in information, rendering interpretation of the data provided by the exam more complex; this may result in assessment errors by less experienced operators. Standardization of procedures and training in echocardiography is therefore essential to ensure quality and safety for patients. The present document aims to contribute to this end, recommending quality requirements for operators and echocardiography laboratories in Portugal.
A ecocardiografia é o método de imagem mais usado na prática clínica diária da cardiologia moderna, dada a sua disponibilidade, portabilidade, ausência de efeitos biológicos deletérios relevantes e menor custo quando comparada com a maioria das outras modalidades de imagem. A evolução tecnológica das últimas décadas, com a introdução de novos e cada vez mais complexos métodos de avaliação ecocardiográfica, alargou ainda mais as indicações para a realização de um ecocardiograma; no entanto, conduziu igualmente ao aumento da informação produzida pelo exame e à maior complexidade da sua interpretação com potencial geração de erros de avaliação por operadores com menor experiência. De modo a assegurar a qualidade e a segurança dos exames minimizando os riscos para os pacientes e a necessidade de duplicação de exames, é necessário uniformizar a prática da ecocardiografia em Portugal. O presente documento pretende contribuir para este esforço, enumerando-se competências a adquirir e procedimentos a adotar de modo a garantir operadores e laboratórios qualificados.
Echocardiography is the most widely used imaging technique in cardiological clinical practice, since it is readily available and provides a comprehensive morphological and functional assessment in real time and at low cost. It is thus the first-line examination for the majority of cardiovascular conditions and has a significant effect on subsequent diagnostic and therapeutic strategies.1,2 Even a basic echocardiographic exam involves different imaging modes that provide supplementary data. Recent technological advances have further increased the information provided and widened the clinical applications of echocardiography. It is therefore essential to ensure that operators and echocardiographic laboratories fulfill quality requirements for performing and interpreting the exam.
ObjectiveThe aim of the present document is to improve and standardize echocardiographic procedures in Portugal, setting out the competences to be acquired and the procedures to be adopted by operators and echocardiographic laboratories in order to ensure the quality and safety of echocardiographic exams. The three elements essential to the final quality of the exam will be addressed: the exam itself (procedure and report); the echocardiography laboratory; and the operator.
This document deals only with transthoracic echocardiography (TTE) in adults. Transesophageal echocardiography (TEE), pediatric echocardiography (TTE and TEE), exercise and pharmacological stress echocardiography, and intraoperative echocardiography (TTE and TEE) in cardiac surgery or during percutaneous interventions are generally excluded from these standards, given their specific characteristics and complexity; in the future they will be the subject of separate guidelines. In addition, although some of the areas dealt with may be more applicable to a hospital setting, the main quality principles set out in this document should be equally applicable to echocardiography in outpatient settings, albeit with minor adaptations if required.
The statutory regulation of medical acts such as echocardiography does not come under the jurisdiction of scientific societies, so these recommendations cannot overrule current laws. Nevertheless, this document was presented to and discussed with the College of Cardiology of the Portuguese Order of Physicians, and their formal and explicit agreement was obtained.
The echocardiographic examTTE involves an integrated combination of two-dimensional (2D) imaging, with pulsed- and continuous-wave spectral Doppler, color Doppler, M-mode and tissue Doppler.3 Three-dimensional echocardiography is still at the consolidation stage for clinical purposes; its use when indicated is optional and depends on local availability and experience.4,5
A complete TTE study includes assessment of the morphology and function of all cardiac chambers, valves and great vessels from multiple views. This requires measurements using 2D, M-mode and spectral and tissue Doppler images; quantification of systolic and diastolic function; calculation of regurgitant and stenotic valve orifices; and estimation of filling pressures and pulmonary artery pressure.3
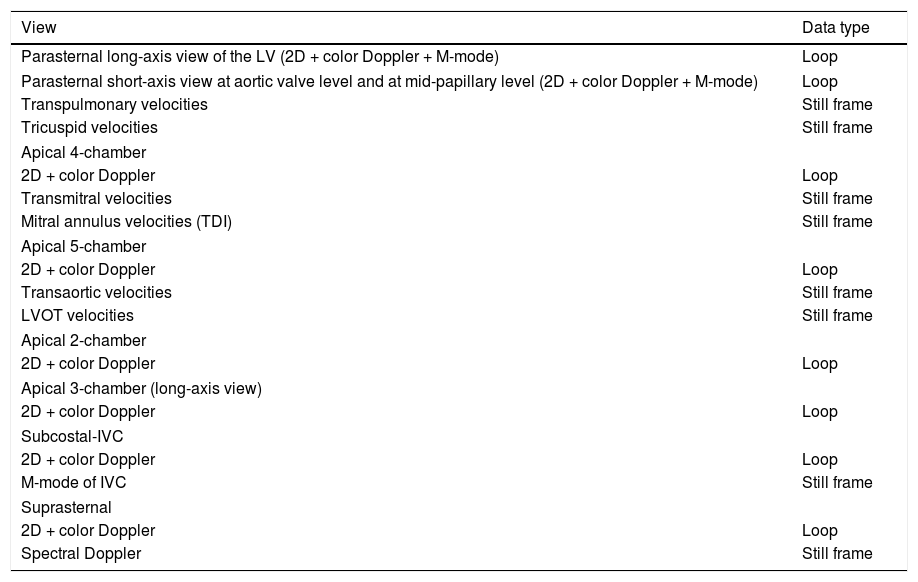
Although the sequence in which the information is acquired may vary depending on local practices and preferences,3,6,7 a minimum dataset of cine-loops or still frames in different views is required for a complete TTE exam from which a high-quality final report can be derived (Table 1).
Minimum dataset required for a complete transthoracic echocardiogram.
| View | Data type |
|---|---|
| Parasternal long-axis view of the LV (2D + color Doppler + M-mode) | Loop |
| Parasternal short-axis view at aortic valve level and at mid-papillary level (2D + color Doppler + M-mode) | Loop |
| Transpulmonary velocities | Still frame |
| Tricuspid velocities | Still frame |
| Apical 4-chamber | |
| 2D + color Doppler | Loop |
| Transmitral velocities | Still frame |
| Mitral annulus velocities (TDI) | Still frame |
| Apical 5-chamber | |
| 2D + color Doppler | Loop |
| Transaortic velocities | Still frame |
| LVOT velocities | Still frame |
| Apical 2-chamber | |
| 2D + color Doppler | Loop |
| Apical 3-chamber (long-axis view) | |
| 2D + color Doppler | Loop |
| Subcostal-IVC | |
| 2D + color Doppler | Loop |
| M-mode of IVC | Still frame |
| Suprasternal | |
| 2D + color Doppler | Loop |
| Spectral Doppler | Still frame |
IVC: inferior vena cava; LV: left ventricular; LVOT: left ventricular outflow tract; TDI: tissue Doppler imaging.
In each cine-loop, at least one and preferably three cardiac cycles, representative of a normal cycle, should be recorded. In cases of arrhythmias with significant R-R variability, a greater number of cycles or a longer acquisition time should be considered. Additional views and acquisitions may be required to aid diagnosis in the event of specific pathologies being identified during a basic exam. It is the responsibility of the interpreting physician to ensure that all relevant information is obtained before the final report is issued.
Images from the exam should be stored digitally, using systems that enable subsequent review. A complete patient record includes images and measurements as well as the final report. In some circumstances, such as emergencies or situations with technical limitations, complete acquisition of images and other data may not be performed. In such cases the exam should be classified as limited or focused and the reasons for performing such an exam should be clearly stated in the report.
Technological advances have led to the development of small portable and even hand-held echocardiographic imaging systems. These present significant advantages, potentially enabling echocardiographic exams to be performed in a wider range of settings and with greater ease of access and hence expanding the benefits of the technique.8 However, the use of these scanners must not be allowed to compromise the quality of the exam. The decision whether to use a portable system outside the echocardiography laboratory should be guided by the patient's clinical stability as assessed by the attending physician with the agreement of a cardiologist. The principles outlined above should also be applied to portable systems; the quality of the exam should not be affected by the particular imaging system being used, especially with regard to the acquisition and digital storage of the minimum dataset of loops and still images. Exceptionally, portable systems can be used by non-cardiologists in emergency situations as an adjunct to the physical examination to rule out shock. In such cases a structured report is not required but images must still be stored digitally and the echocardiographic data must be recorded in the patient's medical record.9
The echocardiography report should have a clear structure, use language comprehensible to non-cardiologists, and provide an objective answer the question that prompted the referral for the echocardiogram. The report structure may vary depending on local preferences, and findings may be organized by anatomic structure or imaging mode. However, all reports should include3,6:
- •
a heading that should contain at a minimum the patient's demographic and other identifying information, the date of the exam and the reason it was ordered, and the names of the individuals performing the study and interpreting the report. It is also recommended that other data be recorded, including weight, height and body surface area, heart rate and cardiac rhythm, and identification of the equipment used;
- •
a measurements section with a record of all the dimensions and values obtained using the different modalities;
- •
a description of the morphological and functional findings of the different anatomic structures assessed;
- •
a summary, which should be clear and comprehensible to any physician, responding objectively to the questions that prompted the exam and highlighting its main findings. Any limitation or factor that might have affected the conclusions should be clearly recorded.
The report should be written in digital form and/or as hard copy and signed by the cardiologist with competence in echocardiography who is responsible for the report, preferably with a password-protected digital signature. Reports of elective exams should preferably be available on the day of the test, or within five working days. In urgent or emergent cases, an interim report should be provided immediately. If the echocardiographic findings necessitate urgent therapeutic measures, the patient's attending physician should be informed personally.
According to the recommendations on training in echocardiography and standards for echocardiographic exams of the College of Cardiology of the Portuguese Order of Physicians,10 a TEE exam should preferably be performed and the report produced by a cardiologist; alternatively, the exam may be performed by a cardiac sonographer, who may also produce an interim report, but only under the supervision and with the approval of a cardiologist, who will in all cases be responsible for the final report.
To carry out these duties, the cardiologists involved require specialized competence in echocardiography (see below), and should be physically present so that they can give advice during the examination and, if necessary, reacquire images, as well as produce the final report. Regardless of whether the exam is performed by a cardiologist or cardiac sonographer, a final digital or hard-copy report must be produced, which is to be signed by the reporting cardiologist only.
The echocardiography laboratoryAlthough the internal organization of departments may vary in different locations, the echocardiography laboratory should ideally be part of a cardiac imaging laboratory that provides echocardiography as well as other noninvasive cardiac imaging facilities such as magnetic resonance imaging and computed tomography.
In order to be able to produce complete and reliable echocardiograms, appropriately trained operators must have a suitably structured and equipped workplace.11,12
Exam rooms should have sufficient space (at least 20 m2 in area) to allow adequate comfort, privacy and safety for patients and operators, and should be equipped with appropriate temperature control, ventilation and lighting. Although TEE under sedation and pharmacological stress echocardiography are beyond the scope of this document, laboratories offering these modalities must have on-site monitoring and advanced life support facilities and a recovery room with surveillance by appropriately trained and qualified personnel.13
To ensure that quality images and complete Doppler hemodynamic measurements are acquired, all echocardiography machines should have facilities for 2D harmonic imaging, pulsed and continuous-wave spectral Doppler, color Doppler and tissue Doppler and for digital storage of images in DICOM format, with the option to export to the local network. All machines and probes should undergo regular maintenance (at least twice a year), generally performed by representatives of the manufacturer in accordance with specific maintenance agreements or, alternatively, by specialized local staff. Maintenance should include specific procedures to ensure the safety of the equipment, such as cleaning filter systems and checking for any current leakage and/or interference with other equipment. Ideally, any machine in regular use should have undergone a software/hardware upgrade within the previous seven years.
The exam can be physically demanding for the operator, sometimes resulting in musculoskeletal strain. It is therefore important that the cardiac imaging laboratory be appropriately structured in order to minimize risk to personnel, according to the following recommendations:
- •
The room in which the exams are carried out should be separate and used only for that purpose. Patient waiting areas, changing rooms and recovery rooms should be physically separate from the exam room.
- •
There should be a separate room for viewing images offline and for producing the report.
- •
Within the exam room, there should be adequate lighting, ventilation, and seating for operators.
- •
The height of the echocardiography bed should be adjustable.
The prolonged close proximity of operator to patient poses a risk of infections spreading. Echocardiographic facilities within hospital settings should therefore maintain links with their local infection control department and follow standard recommendations. All staff should be regularly updated with respect to current recommendations. The following general rules should be followed:
- •
Probes should be cleaned between exams with an appropriate disinfectant wipe or solution.
- •
Operators should wash their hands thoroughly between exams. A sink for hand washing must be available in the exam room.
- •
Echographic machines should be cleaned daily.
- •
TEE probes require specific disinfection procedures with special areas and equipment, including appropriate air extraction systems to prevent contamination by volatile disinfectants of the environment and of cleaning personnel.
The echocardiography laboratory should have an organized scheduling system. The time allocated for a standard transthoracic study should be at least 30 min; when complex quantification and/or the use of advanced modalities is required the allotted time should be 60 min. The head of the laboratory should put in place a system for filtering and prioritizing requests for the exam. Quality control measures should also be implemented through periodic audits to assess the reasons for requesting echocardiograms, waiting and exam times, and the quality of the images and measurements acquired and reports produced.
There should be periodic departmental meetings, preferably weekly, to review clinical cases, ideally jointly with other imaging modalities. These meetings should be the responsibility of the clinical head of the laboratory. The level of scientific knowledge of the staff is also a quality criterion. Personnel should have access to relevant literature for their clinical work and research, via a local library with reference textbooks and with electronic access to the main cardiology and echocardiography journals.
The operatorVarious guidelines on training and competence in echocardiography have been issued in recent years by different medical societies.7,14,15 As shown by these documents, echocardiography is considered to be a highly operator-dependent imaging technique for which specific training is required to acquire competence. The operator's basic training should include:
- •
general training in cardiology, including in cardiac auscultation;
- •
detailed knowledge of cardiovascular anatomy, physiology and hemodynamics under normal conditions and in different disease states;
- •
sufficient knowledge of the physical principles and biological effects of ultrasound to use echocardiographic equipment correctly and to be aware of the indications for and limitations of the technique;
- •
the ability to use clinical information from the referring physician, medical records and patients in order to apply the most appropriate methodology to obtain adequate echocardiographic information;
- •
the ability to recognize abnormalities and to form a preliminary set of differential diagnoses, in order to exploit the views and to perform any necessary quantification;
- •
the ability to correlate and integrate echocardiographic findings with those of other diagnostic methods and to form an overall picture of the results;
- •
knowledge of potential complications of the different echocardiographic techniques.
There are differences between the programs and requirements for attribution of levels of competence specified by international medical societies, resulting from specific local factors and differences in the legal framework for postgraduate training. The former European Association of Echocardiography (now the European Association of Cardiovascular Imaging) proposed two levels of competence in echocardiography,15 which are generally accepted as valid in Portugal: basic and advanced.
- a)
Basic level
This level is a requirement in the training of every cardiologist. On completion, the operator should be able to independently perform a standard echocardiographic exam, be able to answer common clinical questions and to be helpful in urgent clinical situations.
A six-month training period in a high-volume hospital echocardiography laboratory is the minimum to achieve the basic level of expertise in TTE. The trainee should perform at least 350 complete exams autonomously with a case-mix covering the main cardiovascular diseases: valvular heart diseases, ischemic heart disease, cardiomyopathies, heart failure, hypertension, infective endocarditis, cardiac masses, common congenital heart defects, pulmonary embolism, pulmonary hypertension, and diseases of the aorta and of the pericardium. Normal exams should not exceed one third of the total. The six-month period should be extended if training is interrupted or carried out concurrently with other activities or if the number of exams performed is less than that stipulated in these recommendations.
Exposure to and execution of TEE and stress echocardiographic exams under the supervision of a cardiologist with advanced competence in echocardiography is recommended, so that at the end of basic level training, the trainee should be familiar with the indications, contraindications, diagnostic capabilities, limitations and potential complications of these modalities. However, this level does not confer competence to perform TEE or stress echocardiography independently.
With regard to the Portuguese regulatory framework, the recommendations for the basic level of competence are in line with Order in Council no. 46/2011, which governs the medical internship of cardiology, and with the recent document issued by the College of Cardiology of the Order of Physicians on training and standards in echocardiography,10 meaning that any cardiologist who completes the specialty internship must have attained this basic level. However, achieving this level of competence is not the same as maintaining it, which requires continuous training (see below). Similarly, accreditation awarded by a competent medical society recognized by the Portuguese Society of Cardiology and the Order of Physicians should be classified as a certificate of knowledge that may complement but cannot replace continuous training in an accredited echocardiography laboratory, which is essential for obtaining national certification of competence in echocardiography in Portugal.
- b)
Advanced level
Advanced level training is intended for cardiologists whose main area of interest and subspecialty is echocardiography. Operators at this level are able to independently perform complex TTE exams as well as those requiring advanced techniques such as complete hemodynamic assessment of complex valve disease, three-dimensional and contrast echocardiography, myocardial deformation imaging (strain and strain rate), and selection of candidates for percutaneous treatment of valvular and non-valvular structural heart disease. The advanced level of competence is required for operators who independently perform TEE and stress echocardiographic exams, intraoperative echocardiography during cardiac surgery, and echocardiographic monitoring of percutaneous procedures.
This level requires an additional six months of training and at least 750 complete TTE studies beyond those performed for basic training at an appropriate hospital echocardiography laboratory under the supervision of a cardiologist with advanced level competence.
During the training period for either level, trainees should regularly attend departmental meetings to discuss cases, as well as national and/or international accredited echocardiography meetings. It is recommended that the trainee be involved in the research projects of the laboratory.
- c)
Maintenance of competence
In order to maintain the competence acquired during training, operators should perform and interpret at least 250 TEE studies per year with an appropriate case-mix. The number of normal exams should not exceed 30% of the total in any year. This exposure should be verifiable by access to the digitally stored images acquired in each exam. In addition to the minimum number of exams, maintenance of competence should also involve regular participation in continuous training programs in echocardiography, preferably verifiable by obtaining credits.
Cardiologists who have not fulfilled the requirements for maintenance of competence in echocardiography for the previous two years should undergo at least one month of training in a high-volume (at least 20 cases per day) echocardiography laboratory with a varied case-mix.
As stated above, operators are encouraged to obtain reaccreditation by a competent medical society recognized by the Portuguese Society of Cardiology and the Order of Physicians, although by itself this is insufficient to prove maintenance of competence.
Levels of competence for non-cardiologists- a)
Cardiac sonographers: training
Cardiac sonographers, who are cardiopulmonary technicians specializing in echocardiography, are part of the team in most Portuguese echocardiography laboratories. Decree-Law 564/99 specifies that the work of cardiopulmonary technicians “focuses on technical aspects of the study of the functional state and anatomophysiological capacity of the heart, cardiac vessels and lungs, including planning, applying and assessing diagnostic techniques, as well as performing specific therapeutic actions, in cardiology, pulmonology and cardiothoracic surgery.” Cardiac sonographers, who must be graduates, are covered by the Ministry of Health's Regime for Diagnostic and Therapeutic Technicians, which is governed by different legal instruments (Decree-Law no. 261/93, Decree-Law no. 320/99, Decree-Law no. 564/99, and Order in Council 256-A/86 no. 3). However, all of these documents are general in nature and do not specify the precise degree of independence or responsibility attributable to cardiac sonographers in performing TTE.
The document on training and standards of the College of Cardiology of the Order of Physicians10 cited above acknowledges that the degree of autonomy granted to operators varies across institutions. It permits cardiac sonographers to perform TTE exams but recommends that such exams be supervised and validated by a cardiologist, who will also be responsible for the final report.
It is recommended that the competences required for cardiac sonographers working in an echocardiography laboratory should include the following:
- •
explaining the procedure to the patient before it is performed. However, obtaining pertinent clinical information required for the exam should remain the exclusive responsibility of the physician who is responsible for the final report;
- •
performing exams following the stipulated technical standards, obtaining the images and measurements that constitute a complete echocardiographic study according to the recommendations set out in this document. In the event of difficulty or inconsistency, the supervising cardiologist should be notified during the exam in order to provide direct assistance;
- •
recording still images and cine loops in digital format in a manner that allows full review of exams and long-term storage;
- •
interpreting images under the supervision of a cardiologist with competence in echocardiography;
- •
providing a preliminary interpretation when clinical circumstances require;
- •
participating in the production of the final report, together with the supervising cardiologist. This collaboration is essential to ensure that the technical and diagnostic information in the report is as complete as possible. It should be stressed that the cardiac sonographer is not responsible for validating the final report, which is the responsibility of the interpreting physician. Likewise, discussions of the findings of the exam with the patient or with the referring physician are the exclusive responsibility of the interpreting cardiologist who produced the final report;
- •
obtaining routine periodic quality assurance and safety checks on the ultrasonography equipment.
Any operator who performs TTE, including cardiac sonographers, should have mastered the basic principles and knowledge required for echocardiography set out at the beginning of this section.16
- b)
Cardiac sonographers: obtaining and maintaining competence
In recognition of the significant differences between countries and regions with regard to the role of echocardiographic technicians,17 the European guidelines do not differentiate between the training periods and number of exams to be performed to obtain competence in TEE for non-physicians as opposed to physicians.15 In the absence of this distinction, and bearing in mind that in most Portuguese institutions sonographers also participate in complex TTE, TEE and stress echocardiographic studies, a minimum one-year full-time postgraduate training period is recommended for cardiac sonographers, in a high-volume (at least 20 cases per day) hospital echocardiography laboratory, with a varied case-mix, under the supervision of a cardiologist with advanced competence in echocardiography. During this period the trainee should perform at least 350 complete exams, which should be verifiable by consultation of digitally stored images and recorded in a log book.
As for physicians specializing in cardiology, cardiac sonographers should preferably take an accreditation examination in echocardiography set by a competent society recognized by the Portuguese Society of Cardiology and the Order of Physicians following proposal by the clinical director of the laboratory or by another cardiologist with competence in echocardiography. In the same way as for cardiologists, such accreditation should be classified as a certificate of knowledge but not of competence in echocardiography and does not in itself qualify the sonographer to perform or interpret echocardiograms without the supervision and validation of a cardiologist with competence in echocardiography. This recommendation is made explicit in the document issued by the College of Cardiology of the Order of Physicians,10 which states that “European Association of Echocardiography accreditation should be taken as formal recognition of previous and continuing autonomy in performing echocardiograms and producing reports, functions which in Portugal can only be carried out by cardiologists.” As for cardiologists, maintenance of competence is dependent on continuous practice in a high-volume (at least 20 cases per day) echocardiography laboratory with a varied case-mix, including at least 250 TEE studies per year, of which normal exams should not exceed one third of the total. In the event of activity being interrupted for a period exceeding one year, a retraining period of at least one month in a high-volume echocardiography laboratory is recommended, with the sonographer performing at least eight TTE exams per day.
- c)
Non-cardiologist physicians
The document issued by the College of Cardiology of the Order of Physicians on training and standards in echocardiography10 recommends that the use of this technique by non-cardiologist physicians should be limited to 2D and M-mode echocardiography in emergency situations to diagnose potentially reversible causes of shock, particularly severe left ventricular dysfunction, severe hypovolemia, high-risk pulmonary embolism and cardiac tamponade. In such settings, a focused emergent echocardiogram is potentially life-saving. Using the internationally recognized FATE (focus assessed transthoracic echocardiography) and FoCUS (focus cardiac ultrasound) methodologies,18–20 this capability is based on a level of training and competence that requires the acquisition of basic knowledge of the physics of ultrasound, normal echocardiographic anatomy, typical images of patients in shock as referred to above, and – most importantly – recognition of the limitations of this level of competence and of the need to consult a cardiologist with basic or advanced competence in echocardiography if possible in such situations. The level of competence for emergency TTE requires the completion of at least 50 exams in a period of not more than one year and confirmation that the indication for these exams was appropriate in cases of shock as described above, as well as the acquisition of standard cine loops and/or still images in accordance with the FATE/FoCUS protocol, duly stored in digital format and validated by a cardiologist with competence in echocardiography. It should be noted that the Order of Physicians only recognizes basic and advanced training in echocardiography for “specialists in cardiology”.10
It should be stressed that, except for the focused exams for shock referred to above, echocardiography in emergency and intensive care situations can be a highly complex procedure.9 When performing a TTE exam with complete Doppler study as well as 2D and M-mode assessment, the need to obtain information and to make decisions rapidly, the frequent difficulty in obtaining high-quality images, and the hemodynamic variability caused by the clinical condition as well as by fluid management measures and inotropic support, can lead to errors in interpretation that could have serious implications for therapeutic decision-making. Such errors are even more likely when the operator is less experienced and less knowledgeable in cardiology. The Portuguese Society of Cardiology therefore recommends that before performing echocardiographic studies in emergency departments and intensive care units without a cardiologist being present, non-cardiologist physicians should undergo a six-month training period in a hospital echocardiography laboratory, performing 350 complete exams and interpreting an additional 150 echocardiograms, covering the main clinical entities found in emergency and intensive care settings. Of the 350 exams performed by the trainee, 50 should be performed in a general emergency department or an intensive care unit, under the supervision of a cardiologist with competence in echocardiography. It should be noted that the fact that an echocardiographic exam is performed in an emergency setting does not mean that recording of images in digital format is unnecessary, since these exams will need to be reassessed and the report validated as rapidly as possible by a cardiologist with competence in echocardiography. Maintenance of competence in emergency or intensive care TTE requires regular practice in the technique, with a recommended minimum of 50 cases per year.
As for other operators, passing an accreditation examination in echocardiography set by a competent society recognized by the Portuguese Society of Cardiology and the Order of Physicians should not be considered to confer certification of competence and does not in itself qualify the sonographer to perform or interpret echocardiograms without the supervision and validation of a cardiologist with competence in echocardiography.
With regard to TEE during cardiac surgery or in an intensive care setting, there may be specific local circumstances in Portugal, as in the rest of Europe, which result in such exams being conducted by non-cardiologist physicians such as anesthesiologists or intensivists. Regulation of training in this area to ensure exam quality and patient safety will be the subject of a document to be issued by the Order of Physicians in accordance with the recommendations of the Portuguese Society of Cardiology. In the meantime, the minimum training requirements to obtain competence in this area should in no case be less than those for cardiologists with advanced competence in echocardiography, i.e. complete training in TTE as described above and at least an additional 75 TEE exams. Maintenance of this competence requires a minimum of 50 TEE exams per year.
In conclusion, as echocardiography is a diagnostic imaging technique that leads to procedures and therapeutic options that are of considerable importance to the patient, it must be considered a medical act with significant medicolegal implications. The aim of the regulation of the practice of echocardiography introduced in the present document is to ensure the quality and safety of echocardiographic exams, minimizing diagnostic errors and risk to the patient, while also reducing duplication of exams and associated costs.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sampaio F, Ribeiras R, Galrinho A, Teixeira R, João I, Trabulo M, et al. Documento de Consenso e Recomendações para a realização de Ecocardiografia Transtorácica em Portugal. Rev Port Cardiol. 2018;37:637–644.