Behavioral and emotional factors are triggers of cardiovascular events (CVEs). It is uncertain whether soccer fans, particularly individuals with coronary artery disease (CAD), are at increased risk for CVEs.
ObjectivesTo assess the effect of watching soccer matches in patients with known CAD on the incidence of CVEs according to the match result.
MethodsWe prospectively assessed 82 male soccer fans with a history of acute coronary syndrome during 23 matches of the 2015/2016 season. Each individual was assessed by Holter monitoring on the day of their team's match and on the control day. The primary endpoint was the composite of death, stroke, reinfarction, angina or sustained arrhythmia. Secondary endpoints assessed were episodes of non-sustained supraventricular or ventricular arrhythmia and mean heart rate (HR).
ResultsParticipants’ mean age was 61±10 years. Compared with the control day, despite a significant increase in HR (p<0.001) that was independent of the result (p>0.97), the number of CVEs did not differ according to the result (p>0.05). Moreover, the number of non-sustained episodes of supraventricular and ventricular arrhythmia did not differ when stratified according to the match result (p>0.05).
ConclusionsThe match result was not associated with a difference in incidence of CVEs in patients with a past history of CAD, with ischemic and arrhythmic substrate, who watched soccer matches on television.
Fatores comportamentais e emocionais são desencadeantes de eventos cardiovasculares (ECV). Permanece incerto se espetadores de jogos de futebol, em particular indivíduos com doença arterial coronária (DAC), estão expostos a maior risco de ECV.
ObjetivosAvaliar o efeito da assistência a jogos de futebol em doentes com DAC na incidência de ECV de acordo com o resultado obtido pela equipa de apoio.
MétodosAvaliados prospetivamente 82 adeptos de futebol do sexo masculino com antecedentes de síndrome coronária aguda, durante 23 jogos de futebol da época 2015/2016. Cada indivíduo foi monitorado com Holter no dia do jogo da sua equipa e em dia controlo em período homólogo à hora do jogo. Avaliado como endpoint primário o composto de morte, acidente vascular cerebral, re-enfarte, angor ou arritmias mantidas. Avaliados ainda como endpoints secundários, episódios de disritmia supraventricular ou ventricular não mantida e frequência cardíaca média.
ResultadosA idade média foi 61 ± 10 anos. Comparado com o dia controlo, apesar do aumento significativo da frequência cardíaca na hora de jogo (p < 0,001) que foi independente do resultado (p > 0,97), o número de eventos cardiovasculares não foi diferente tendo em conta o resultado (p > 0,05). Também o número de episódios de disritmia supraventricular e ventricular não mantida não foi diferente estratificando de acordo com o resultado (p > 0,05).
ConclusãoO resultado do jogo não se associou a diferente incidência de eventos cardiovasculares em doentes com substrato isquémico e arrítmico por antecedentes de DAC que assistiram a jogos de futebol na televisão.
The incidence of sudden cardiac death in Europe is around 1/1000 population. Ventricular arrhythmias resulting from coronary artery disease (CAD) are responsible for most of these cases. There is also plentiful evidence that patients who are not completely revascularized are at higher risk of malignant arrhythmias than those who undergo complete revascularization.1–3
The environmental, behavioral and emotional effects of events such as war, terrorist attacks or earthquakes can trigger cardiovascular events (CVEs).4–10
Soccer is an immensely popular sport worldwide, and often arouses intense emotional involvement in fans. There is a common belief that this can potentially trigger CVEs.
However, previous studies involving soccer fans are conflicting. While several reports show an increase in CVEs associated with major soccer games, other authors report a protective effect on the incidence of CVEs in the period around the same matches.11–18
For example, Leeka et al.19 and Culic20 stress the importance of the match, its intensity and the final result as contributing factors to CVEs.
A major limitation of all previous studies is that they are based not only on retrospective records, but also on the assumption that a sporting event affects the entire population equally, regardless of cardiac status, actual exposure to the game, or the level of emotional attachment to the sport and the team.
It is therefore unclear whether soccer spectators, and in particular individuals with CAD, are at greater risk of CVEs.
The aim of this study was to prospectively assess the effect of watching soccer games on the incidence of CVEs in CAD patients, according to the game result for the team supported.
MethodsThis was a prospective single-center study including subjects with a history of ST-elevation myocardial infarction (STEMI) (with or without complete revascularization) or non-ST-elevation myocardial infarction (NSTEMI) with incomplete revascularization, who were fans of one of the three largest soccer clubs in Portugal (Sporting Clube de Portugal [SCP], Sport Lisboa e Benfica [SLB] or Futebol Clube do Porto [FCP]), or of the Portuguese national soccer team, and who were assessed at soccer games during one sports season (Table 1).
Games and results included in the study.
| Game, date, and kick-off time | Teams and result |
|---|---|
| Supertaça de Portugal 08/09/2015 – 8:45 pm | SCP vs. SLB 1-0 |
| Portuguese national league 09/20/2015 – 7:15 pm | FCP vs. SLB 1-0 |
| Portuguese national league 10/25/2015 – 5:00 pm | SLB vs. SCP 0-3 |
| Portuguese Cup 11/21/2015 – 8:00 pm | SCP vs. SLB 2-1 |
| Portuguese national league 01/02/2016 – 8:45 pm | SCP vs. FCP 2-0 |
| Portuguese national league 02/12/2016 – 8:30 pm | SLB vs. FCP 1-2 |
| UEFA Europa League 02/18/2016 – 8:05 pm | SCP vs. Bayer Leverkusen 0-1 |
| Portuguese national league 03/05/2016 – 8:45 pm | SCP vs. SLB 0-1 |
| Portuguese national league 04/16/2016 – 8:45 pm | Moreirense vs. SCP 0-1 |
| Portuguese national league 04/24/2016 – 8:30 pm | Rio Ave vs. SLB 0-1 |
| Portuguese national league 04/30/2016 – 6:30 pm | FCP vs. SCP 1-3 |
| Portuguese national league 05/08/2016 – 8:30 pm | Marítimo vs. SLB 0-2 |
| Portuguese national league 05/15/2016 – 5:00 pm | SLB vs. Nacional 4-1 |
| Portuguese Cup Final 05/22/2016 – 5:15 pm | FCP vs. Braga 2-4 |
| Euro 2016 06/14/2016 – 8:00 pm | Iceland vs. Portugal 1-1 |
| Euro 2016 06/18/2016 – 8:00 pm | Austria vs. Portugal 0-0 |
| Euro 2016 06/22/2016 – 5:00 pm | Hungary vs. Portugal 3-3 |
| Euro 2016 06/25/2016 – 8:00 pm | Croatia vs. Portugal 0-1 |
| Euro 2016 06/30/2016 – 8:00 pm | Poland vs. Portugal 1-1 (3-5 PSO) |
| Euro 2016 07/06/2016 – 8:00 pm | Portugal vs. Wales 2-0 |
| Euro 2016 07/10/2016 – 8:00 pm | Portugal vs. France 1-0 (AET) |
| Supertaça de Portugal 08/07/2015 – 8:45 pm | SLB vs. Braga 3-0 |
| Portuguese national league 08/28/2016 – 6:00 pm | SCP vs. FCP 2-1 |
AET: after extra time; Euro 2016: UEFA European Championship 2016; FCP: Futebol Clube Porto; PSO: penalty shoot-out; SCP: Sporting Clube de Portugal; SLB: Sport Lisboa e Benfica; Supertaça de Portugal: match between the previous year's winners of the national league and the Cup.
All of the subjects had been hospitalized due to an acute CVE prior to the study. Demographic characteristics, previous personal history (including cardiovascular risk factors, transthoracic echocardiography at discharge and coronary anatomy by angiography), relevant laboratory tests performed during hospital stay, current drug therapy and baseline chronic stress score assessed by the Perceived Stress Scale (PSS)21 were collected from each individual.
All subjects reported regularly watching soccer on television, and specifically watching the team they supported. The validated Football Supporter Fanaticism Scale, which consists of seven items each scored between 1 and 5, was used to assess subjects’ degree of fanaticism (Table 2).22–24 The inclusion criterion was a score of ≥15 on this scale.
Football Supporter Fanaticism Scale.23
| Concept | Category | Indicators | Score |
|---|---|---|---|
| Team preference | Support | Self-image as supporter | 1-5 |
| Watching the team regularly, at the stadium or on television | 1-5 | ||
| Importance of being a supporter | 1-5 | ||
| How much of a supporter your friends think you are | 1-5 | ||
| How important it is that the team wins | 1-5 | ||
| How often you wear team clothing | 1-5 | ||
| Aversion | The team you dislike the most | 1-5 |
The soccer matches included in this study were derbies or classics from the 2015/2016 season, the 2015 and 2016 Supertaça de Portugal matches (between the previous year's winners of the national league and the Cup), the finals of the 2015 and 2016 Portuguese Cup, the last five rounds of the 2015/2016 Portuguese national soccer championship, and Portuguese national soccer team games, starting from the group stage, in the 2016 UEFA European Championship (Euro 2016), which took place in France.
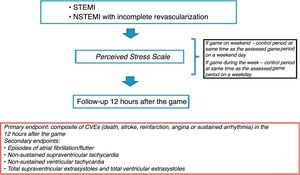
Each individual underwent Holter monitoring on the day of his team's game and on the control day during the same period as the game (if the game took place on a weekday, the control day was also a weekday; if the game took place on the weekend, the control day was also on the weekend) (Figure 1).
The primary endpoint was a composite of CVEs (death, stroke, reinfarction, angina or sustained arrhythmia) in the 12 hours after the game.
Secondary endpoints assessed were episodes of atrial fibrillation/flutter, non-sustained supraventricular tachycardia (SVT), non-sustained ventricular tachycardia (VT), and the total number of supraventricular extrasystoles (SVEs) and of ventricular extrasystoles (VEs) during the game (Figure 1).
Statistical analysisContinuous variables were expressed as mean ± standard deviation or median with interquartile range (IQR) depending on whether the distribution was normal. Categorical variables were expressed as number or percentage. The Wilcoxon test or chi-square test was used for comparison between multiple variables on the game day and the control day. The Kruskal-Wallis test was used for comparison of differences in relation to the game result. IBM SPSS version 22.0 for Windows (IBM SPSS Inc., Chicago, IL) was used for the statistical analysis. The results of the statistical tests were considered statistically significant for p<0.05.
ResultsA total of 82 male patients were enrolled and assessed at 23 games. Their baseline characteristics are summarized in Table 2. Mean age was 61±10 years and 100% were male; 59% had previous STEMI (56% with complete revascularization). Of the study population, 28% were fans of SCP, 35% of SLB, 20% of FCP and 17% of the Portuguese national team.
The median time from the acute CVE to the game assessed was 186 days (IQR 48-596). A history of CAD before the index event was recorded in 21% of participants, hypertension in 53.7%, dyslipidemia in 56.1%, and diabetes in 23.2%, while 56.1% were smokers or ex-smokers and 9.8% had a family history of CAD (Table 2).
At the time of the previous acute event, 89% of participants were in Killip class I, peak troponin I during hospital stay was 32 ng/ml (IQR 1.2-99), and mean left ventricular ejection fraction at discharge was 55±9%. On coronary angiography, 32.9% had single-vessel disease, 24.4% had two-vessel disease, 40.2% had three-vessel disease, and 2.4% had both left main and three-vessel disease. Percutaneous coronary intervention was performed in 76.8% and coronary artery bypass grafting in 2.4%, while 20.7% received optimal medical treatment.
When assessed according to game result, there were no significant differences in the study population in relation to diagnosis, personal history or clinical course during hospital stay (p>0.05) (Table 3).
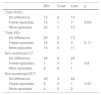
Baseline and clinical characteristics of the study population by game result.
| Total (n=82) | Win (n=51) | Draw (n=4) | Loss (n=27) | p | |
|---|---|---|---|---|---|
| Age, years | 61±10 | 62±11 | 53±14 | 60±9 | 0.17 |
| Male gender | 100% | 100% | 100% | 100% | - |
| Time from CVE to game, days | 186 (48-596) | 235 (54.5-728) | 207 (121-324) | 181 (44.5-551) | 0.88 |
| Team supported | <0.001 | ||||
| SCP | 28% | 35.3% | - | 18.5% | |
| FCP | 19.5% | 11.8% | - | 37% | |
| SLB | 35.4% | 33.3% | - | 44.4% | |
| National team | 17.1% | 19.6% | 100% | - | |
| History | |||||
| CAD | 20.7% | 23.5% | - | 18.5% | 0.5 |
| Hypertension | 53.7% | 52.9% | 50% | 55.6% | 0.97 |
| Dyslipidemia | 56.1% | 56.9% | 50% | 55.6% | 0.96 |
| Diabetes | 23.2% | 19.6% | - | 33.3% | 0.21 |
| Obesity | 9.8% | 11.8% | - | 7.4% | 0.66 |
| Smoking | 56.1% | 55% | 75% | 55.6% | 0.49 |
| PAD | 4.9% | 5.9% | - | 3.7% | 0.82 |
| Family history | 9.8% | 7.8% | 25% | 11.1% | 0.51 |
| Diagnosis | 0.74 | ||||
| STEMI | 58.5% | 56.9% | 50% | 63% | |
| NSTEMI | 25.6% | 25.5% | 50% | 22.2% | |
| Unstable angina | 15.9% | 17.6% | - | 14.8% | |
| Killip class | 0.1 | ||||
| I | 89% | 96.1% | 75% | 77.8% | |
| II | 9.8% | 3.9% | 25% | 18.5% | |
| III | 1.2% | - | - | 3.7% | |
| IV | - | - | - | - | |
| Peak troponin I, pg/ml | 32 (1.2-99) | 12.7 (0.7-50) | 64.8 (39-142) | 42.6 (4.7-125.6) | 0.16 |
| LVEF, % | 55±9 | 54±10 | 57±10 | 56±8 | 0.85 |
| CAD extent | 0.96 | ||||
| 1 vessel | 32.9% | 33% | 25% | 33.3% | |
| 2 vessels | 24.4% | 23.5% | 25% | 25.9% | |
| 3 vessels | 40.2% | 39.2% | 50% | 40.7% | |
| LM and 3 vessels | 2.4% | 3.9% | - | - | |
| Treatment | 0.16 | ||||
| Optimal medical | 20.7% | 29.4% | 0% | 7.4% | |
| PCI | 76.8% | 68.6% | 100% | 88.9% | |
| CABG | 2.4% | 2% | 0% | 3.7% | |
| Medication | |||||
| Aspirin | 97.6% | 98% | 100% | 96.3% | 0.85 |
| Clopidogrel | 26.8% | 27.5% | 0% | 29.6% | 0.45 |
| Ticagrelor | 54.9% | 47.1% | 100% | 63% | 0.07 |
| OAC | 2.4% | 2% | 0% | 3.7% | 0.85 |
| ACEI/ARB | 89% | 86.3% | 100% | 92.6% | 0.54 |
| Beta-blocker | 87.8% | 88.2% | 50% | 92.6% | 0.05 |
| Statin | 97.6% | 96.1% | 100% | 100% | 0.54 |
| OAD | 19.5% | 21.6% | 0% | 18.5% | 0.57 |
| Insulin therapy | 6.1% | 3.9% | 0% | 11.1% | 0.39 |
| Nitrates | 19.5% | 25.5% | 0% | 11.1% | 0.19 |
| Amiodarone | 2.4% | 2% | 0% | 3.7% | 0.85 |
| Diuretic | 17.1% | 19.6% | 0% | 14.8% | 0.56 |
| Difference in mean HR (game-control), bpm | 3.9±7.6 | 3.7±7.2 | 3.5±9.8 | 3.7±7.3 | 0.97 |
| PSS score | 19.6±5.6 | 19.7±6 | 19±2.4 | 19.4±5.4 | 0.89 |
Values expressed as percentages, mean ± standard deviation (95% confidence interval), or median (interquartile range). The Kruskal-Wallis and chi-square tests were used for comparison of variables, as appropriate.
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CVE: cardiovascular event; HR: heart rate; LM: left main; LVEF: left ventricular ejection fraction; NSTEMI: non-ST-elevation myocardial infarction; OAC: oral anticoagulant; OAD: oral antidiabetic; PAD: peripheral artery disease; PCI: percutaneous coronary intervention; PSS: Perceived Stress Scale; SCP: Sporting Clube de Portugal; SLB: Sport Lisboa e Benfica; STEMI: ST-elevation myocardial infarction.
There were also no statistically significant differences in current medication according to game result (p>0.05) (Table 3). Patients’ mean heart rate (HR) increased at the time of the game by an average of 3.9±7.6 bpm compared to the same time on the control day; this increase was independent of the game result (p=0.97) (Table 3 and Figure 2).
The mean PSS score was 19.6±5.6 (Table 3), similar in both study groups (p=0.89).
Primary endpointThere was no statistically significant association between CVEs and the game result (p=0.85).
No death, stroke, reinfarction or sustained arrhythmia was recorded in the 12-hour follow-up. Two participants suffered episodes of angina during the game (one fan of the national team during the Euro 2016 game on July 6, 2016 between Portugal and Wales, won by Portugal, and one FCP fan on August 28, 2016 during a match between SCP and FCP, which FCP lost), neither of which registered on the electrocardiogram.
Secondary endpointsDuring the study period, five episodes of non-sustained VT occurred, in five different individuals (three episodes during the game and two during the control period) (Table 4). In addition, six episodes of non-sustained SVT occurred during the game, in six individuals. No episodes of atrial fibrillation or atrial flutter were detected during the game or control periods (Table 4).
When the secondary endpoints were assessed according to game result, there was no difference in relation to episodes of SVEs, VEs, non-sustained VT or non-sustained SVT (p>0.05). Table 5 shows the number of secondary endpoint events assessed according to game result, with three episodes of non-sustained VT in three individuals whose team won (two of these episodes during the game) and two episodes of non-sustained VT in two individuals whose team lost (one of the episodes during the game).
Stratification of participants according to number of episodes of supraventricular extrasystoles, ventricular extrasystoles, non-sustained supraventricular tachycardia and non-sustained ventricular tachycardia and game result, during the game compared to the control period.
| Win | Draw | Loss | p | |
|---|---|---|---|---|
| Total SVEs | ||||
| No difference | 12 | 2 | 10 | |
| Fewer episodes | 15 | 1 | 7 | 0.64 |
| More episodes | 24 | 1 | 10 | |
| Total VEs | ||||
| No difference | 20 | 2 | 13 | |
| Fewer episodes | 18 | 2 | 3 | 0.11 |
| More episodes | 13 | 0 | 11 | |
| Non-sustained VT | ||||
| No difference | 48 | 4 | 26 | |
| Fewer episodes | 1 | 0 | 1 | 0.8 |
| More episodes | 2 | 0 | 1 | |
| Non-sustained SVT | ||||
| No difference | 45 | 4 | 24 | |
| Fewer episodes | 2 | 0 | 1 | 0.97 |
| More episodes | 4 | 0 | 2 | |
SVEs: supraventricular extrasystoles; VEs: ventricular extrasystoles; VT: ventricular tachycardia; SVT: non-sustained supraventricular tachycardia.
This is the first prospective study in Portugal of patients with known CAD to assess the relationship between watching soccer games and CVEs according to the game result for the team supported by the patient.
There have been various studies of the incidence of CVEs on days when major soccer matches are played, but they are conflicting. For example, Berthier et al. reported a reduction in the occurrence of CVEs during matches, although this study was of subjects in the country that won the competition (the 1998 FIFA World Cup in France). There were significantly fewer deaths due to myocardial infarction (MI) in men in this study on the day of the final match of the competition compared to control days (23 vs. 32.6 cases, relative risk [RR] 0.71, 95% confidence interval [CI]: 0.55-0.98), while in women there was a non-significant decrease (RR 0.65, 95% CI: 0.45-1.16).11
Marques-Vidal et al.16 and Barone-Adesi et al.17 found no increase in CVEs triggered by soccer games. In the population studied by Barone-Adesi et al., there was no increase in MI in soccer-loving Italy on days when the Italian national team played in three major tournaments (the 2002 and 2006 World Cup and the 2004 UEFA European Championship).17
It is interesting to note that two studies on populations watching the same international event, but conducted in different countries, produced opposite results. During the 1996 European Championship, when The Netherlands was eliminated by France, cardiovascular mortality increased among Dutch men, but decreased in the French population.12,13
Conversely, similarly to Wilbert-Lampen et al.,14 who reported an increased rate of cardiac events in Bavaria on days when the German team played during the 2006 World Cup, Borges et al.15 found that World Cup soccer games in 1998, 2002, 2006 and 2010, and in particular matches involving the Brazilian side, were associated with an increased incidence of MI, although not of mortality.
The games included in this study are considered by the public to be major matches and are therefore more emotionally charged. Accordingly, given the fibrotic arrhythmogenic foci of the patients included (patients with STEMI and NSTEMI with incomplete revascularization), it is plausible that these games could be associated with CVEs.
Several mechanisms have been proposed to explain the relationship between emotional triggers and CVEs, including acute physiological changes such as heightened HR and blood pressure, which can transiently increase the risk of plaque rupture and thrombosis and lower the threshold for ventricular fibrillation.25
In our study there was an increase in mean HR during the game compared with the same time on the control day (Figure 2), irrespective of whether the supported team won or lost. Nevertheless, the increased catecholaminergic load assumed to be associated with increased HR did not lead to an increase in major CVEs (death, reinfarction, stroke or sustained arrhythmia), although two episodes of angina did occur during the game, in one supporter whose team won and in another whose team lost.
Various authors have demonstrated that the result of the game can be a key factor in the incidence of CVEs. Differing results in different populations for the same event, as reported by Witte et al.12 and Toubiana et al.,13 were also found by Kirkup et al.,18 in whose population death due to MI and stroke increased significantly in men (RR 1.28; 95% CI: 1.11-1.47) on days when the local soccer team lost at home.
In addition to adrenergic stimulation, some authors argue that watching sports events may contribute to cardiovascular risk due to other behaviors, such as smoking or excessive drinking.26 This was not considered a confounding factor in our study, as there is no consensus that food, alcohol or adherence to medication can contribute to cardiovascular events associated with watching soccer games, and hospital admissions due to CVEs during several soccer tournaments involving the same teams do not show consistent patterns.27
Chronic stress is also believed to contribute to the development and progression of cardiovascular disease and mortality. The mechanisms underlying this association are complex and include a combination of physiological as well as behavioral factors, such as increased blood pressure and HR, reduced insulin sensitivity and endothelial dysfunction. There is evidence that high levels of perceived stress are associated with worse prognosis.28–33
In our study, the mean PSS score was 19.6±5.6. The PSS score in the two patients in whom angina was recorded during the game was 17 in one and 23 in the other, well within the mean and standard deviation range.
Since these participants had a history of previous coronary events, they might be more likely to behave cautiously and calmly during a potentially stressful event, due to their fear of another event, which may partly explain their lower anxiety profile while watching a soccer game, decreasing the risk of triggering a CVE.
Factors such as regular medical monitoring and good adherence to prescribed therapy, particularly optimal anti-ischemic therapy (such as the fact that 90% of the study population were taking beta-blockers, assumed to be at the highest tolerated dose, as suggested by the European guidelines), may explain the low incidence of CVEs. This raises the question whether these findings can be extrapolated to patients without known CAD but with major cardiovascular risk factors.
This study does not answer the question (which would require a larger study to resolve) whether the catecholaminergic surge that occurs during a soccer match can lead to an increase in CVEs, especially in populations at high or very high cardiovascular risk, regardless of whether they have documented CAD and whatever their current medication. If so, there is the potential to apply non-pharmacological or pharmacological prophylactic measures in this population.
LimitationsThis study has some limitations. First, it was designed as a pilot study, so the number of individuals studied was small. Second, it was a single-center study. Third, it did not take into account behaviors often associated with watching soccer games, such as smoking and drinking; these should obviously be considered in a larger study, in order to rule out confounding factors. Patients who watch games in the stadium or who listen to them on the radio were not included, and these might be associated with different anxiety profiles and consequently a different risk of triggering CVEs. The study was designed to assess emotional triggers while watching sporting events, but it was impossible to exclude the existence of other types of emotional triggers for CVEs on the control day which could have biased the results.
ConclusionIn our study, the game result was not associated with a difference in incidence of CVEs in men with a past history of CAD, with ischemic and arrhythmic substrate, who watched soccer matches on television. Preventive measures (such as optimal medical therapy) or behavioral factors could explain the low incidence of cardiovascular events observed.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martins JL, Adrega T, Santos L, Afreixo V, Viana J, Santos J. Jogos de futebol impróprios para cardíacos (HeartAtaque trial) – Estudo piloto prospetivo. Rev Port Cardiol. 2018;37:645–653.