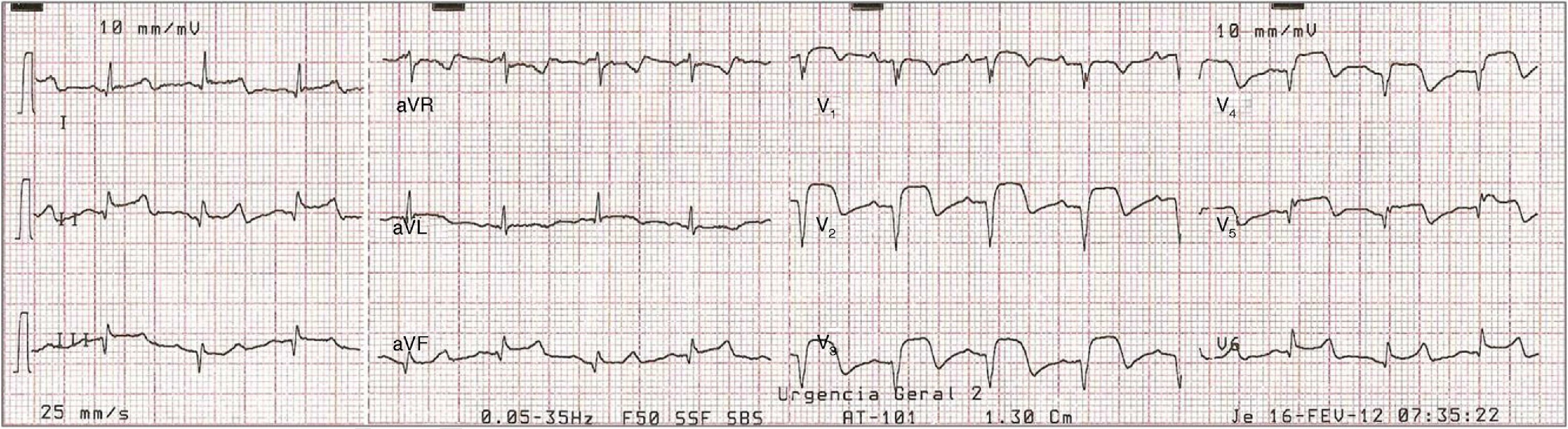
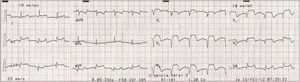
A 74-year-old woman with type 2 diabetes was admitted with malaise and dyspnea for a week. On initial observation she was cooperative; subcrepitant rales were heard in both lung fields and the electrocardiogram showed Q waves and ST-segment elevation in the precordial leads DII and DIII (Figure 1). She was diagnosed with subacute anterior myocardial infarction in Killip class III and coronary angiography was performed, followed by percutaneous coronary intervention of the mid anterior descending artery with stent implantation. An intra-aortic balloon pump was placed to maintain hemodynamic stability and dobutamine infusion (7 μg/kg/min) was begun.
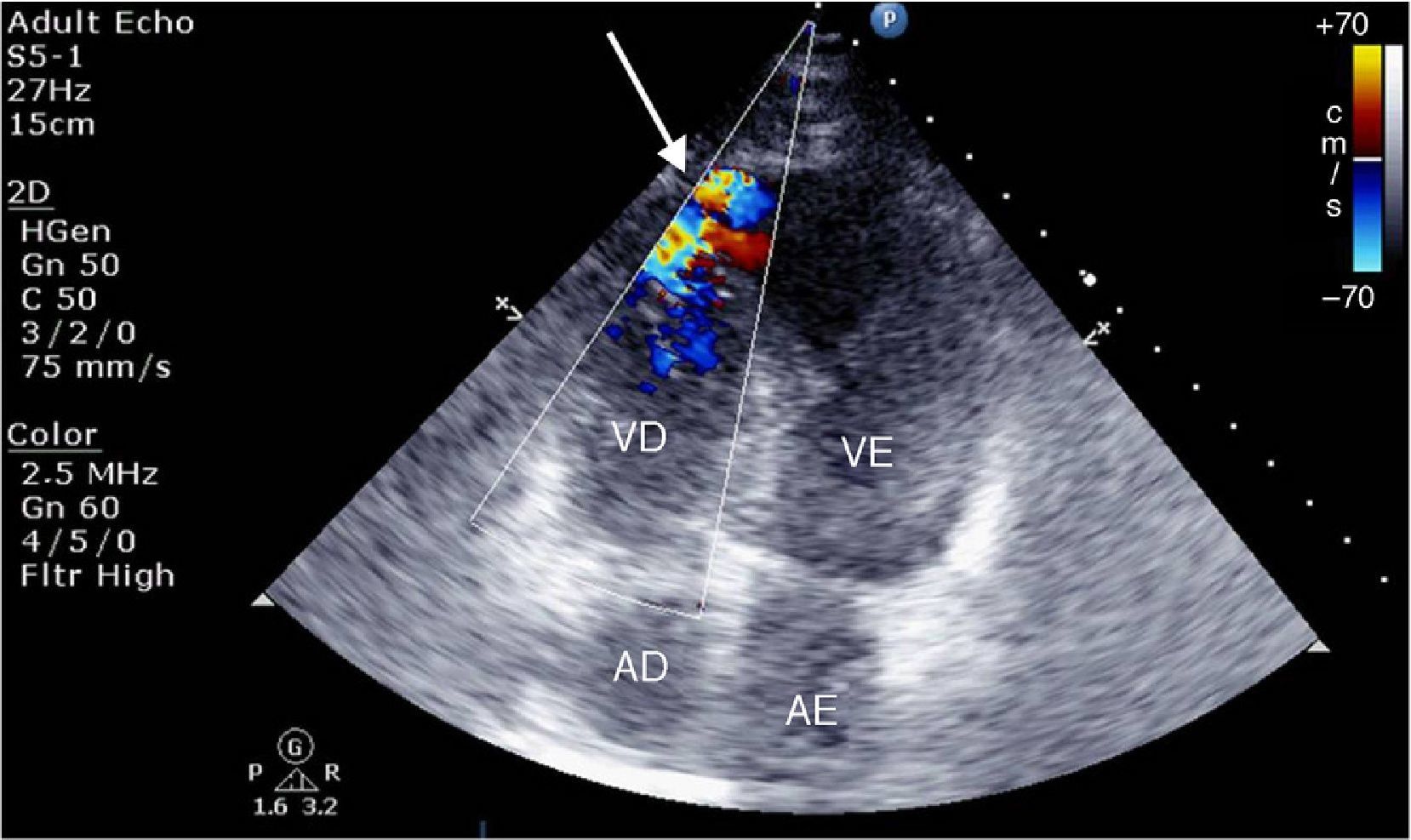
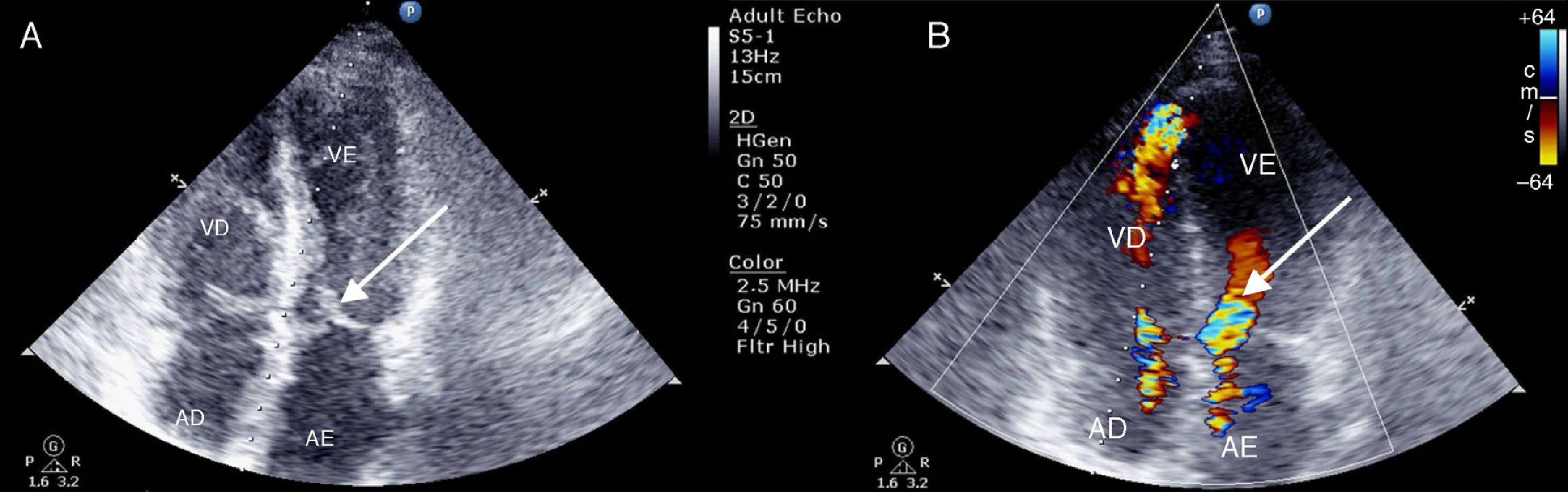
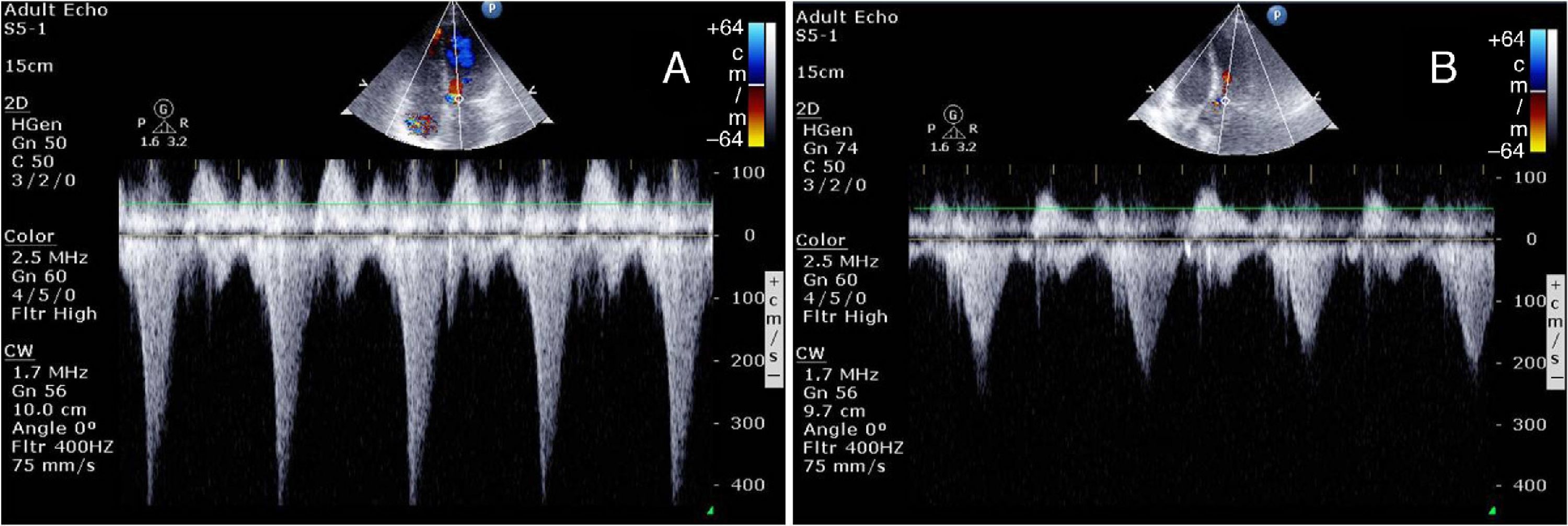
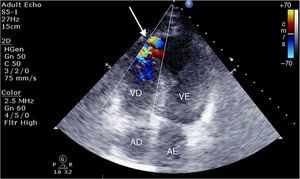
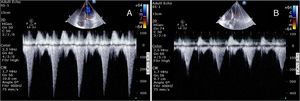
While in the coronary care unit she continued to experience malaise and faintness and her hypotension and oliguria worsened. On cardiac auscultation a grade III/VI holosystolic murmur was detected at the left sternal border, while the echocardiogram revealed akinesia of the apical segments and compensatory hypercontractility of the basal segments, with preserved global left ventricular (LV) systolic function, and a diagnosis was made of non-restrictive apical interventricular septal rupture (Figure 2). Turbulent flow was seen in the LV outflow tract, with a velocity of >4 m/s and systolic anterior motion (SAM) of the anterior leaflet of the mitral valve (Figure 3). In view of LV outflow tract obstruction associated with hypotension, it was decided to discontinue dobutamine perfusion and to administer intravenous propranolol. This resulted in symptomatic improvement and increased blood pressure, and the echocardiogram showed less turbulent and slower flow and improvement of SAM (Figure 4). It was thus possible to stabilize the patient and transfer her to a surgical center, but unfortunately she died of complications in the second week after surgery.
Quantification of dynamic gradients in the left ventricular outflow tract before (A) and after (B) discontinuation of dobutamine and administration of intravenous propranolol (1 mg/kg). The peak gradient in (A) is >64 mmHg with blood pressure of 90/60 mmHg; in (B) the peak gradient has fallen to 16 mmHg and blood pressure has risen to 110/70 mmHg.
We highlight the importance of thorough assessment of possible complications of myocardial infarction through echocardiography, in order to determine the best therapeutic approach, which in this case was to avoid positive inotropes and to use intravenous beta-blockers to reduce intraventricular obstruction.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cruz I, Caldeira D, Stuart B, Cotrim C, João I, Pereira H. Complicações de enfarte do miocárdio: ecocardiograma para diagnóstico diferencial de sopro cardíaco. Rev Port Cardiol. 2015;34:779–781.