Do antiplatelet agents prevent cardiovascular or renal events in individuals with chronic renal disease?
Description of reviewThis is a systematic review and meta-analysis of clinical trials comparing any antiplatelet treatment versus placebo or no treatment, or direct head-to-head antiplatelet agent studies, in individuals with chronic renal disease with regard to cardiovascular events (myocardial infarction, stroke, all-cause mortality and bleeding) and renal outcomes (end-stage renal disease, kidney transplant graft loss, transplant rejection, and adverse events associated with vascular access).1
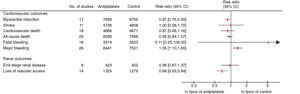
ResultsOf 1093 articles identified by the search criteria, only 44 on antiplatelets versus placebo or no treatment were eligible for inclusion in the systematic review, with a total of 21 460 patients. Mean sample size and follow-up were 100 patients (16–4087) and nine months (1–61), respectively. Studies on patients with renal disease, and those on acute or chronic coronary disease with a subgroup of patients with renal disease, were included. The main antiplatelets analyzed were aspirin (11 studies), dipyridamole (4), aspirin/dipyridamole (6), clopidogrel (5), clopidogrel/aspirin (1), ticlopidine (8), and glycoprotein IIb/IIIa inhibitors (7). The results are summarized in Figure 1.
Main results of the systematic review.1 CI: confidence interval.
There were no significant differences between the different antiplatelet agents in prevention of myocardial infarction (p=0.20), all-cause mortality (p=0.46) or major bleeding (p=0.88).
With regard to severity of renal failure, there were no significant differences between the effects of antiplatelet agents on patients requiring dialysis and those with earlier stages of chronic renal disease in terms of myocardial infarction (p=0.94), all-cause mortality (p=0.30) and major bleeding (p=0.12).
ConclusionsThis systematic review concluded that antiplatelet agents significantly reduce risk for myocardial infarction in individuals with chronic renal disease, but this effect is accompanied by a significant increase in major bleeding. The benefit of antiplatelets was not seen in all-cause or cardiovascular mortality or stroke, and they do not prevent progression to end-stage renal disease; although they reduce the incidence of loss of vascular access due to thrombosis or loss of patency, there is no evidence that they improve fistula maturation or suitability for dialysis.1
CommentThe prevalence of chronic renal disease is increasing in developed countries and is now estimated at 10%; the rise in risk factors such as diabetes and hypertension contributes to this situation.2 The severity of renal disease is directly related to the risk of cardiovascular events.3 It has been suggested that this association is due to the alterations typical of renal disease: inflammatory state, dyslipidemia, hyperhomocysteinemia, hypercoagulability, anemia, left ventricular hypertrophy, endothelial dysfunction and increased vascular rigidity with arterial calcification.4
This systematic review concluded that the best available evidence shows that antiplatelet agents significantly reduce risk for myocardial infarction, but that the protective effect is relatively small, with a reduction in risk ratio of 0.9% and a number needed to treat of 110 patients. There is even uncertainty regarding the size of the effect, since the 95% confidence interval is wide and includes values close to 1 (0.76–0.99). Moreover, no differences were found in cardiovascular and all-cause mortality. Further, the benefit must be weighed against the significant bleeding risk of these drugs and the fact that they do not prevent stroke or fatal events. The authors conclude that in patients without clinically significant cardiovascular disease and low risk for cardiovascular events, such as those in the early stages of renal disease, the risks of antiplatelet therapy outweigh the benefits.
These conclusions should be interpreted in the light of the limitations of this systematic review and meta-analysis and of the studies (of primary and secondary prevention) included, particularly methodological considerations – blinding and/or randomization techniques were inadequate in more than half of the studies analyzed.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Caldeira D, Vaz-Carneiro A, Costa J. Antiagregantes plaquetários na doença renal crónica. Avaliação da revisão sistemática. Rev Port Cardiol. 2013;32:917–918.