Monitoring of disease activity and the best therapeutic approach are a challenge in Takayasu arteritis (TA). When associated with acute coronary syndromes (ACS), the best interventional treatment has not been established. The objective of this study was to describe the baseline characteristics, clinical manifestations, treatment and long-term outcome of patients with TA and ACS.
MethodsWe retrospectively analyzed eight patients between 2004 and 2010. The following data were obtained: age, gender, clinical and electrocardiographic manifestations, Killip class, risk factors for ACS, markers of myocardial necrosis (CK-MB and troponin), creatinine clearance, left ventricular ejection fraction, inflammatory markers (C-reactive protein and erythrocyte sedimentation rate [ESR]), medication during hospital stay, angiographic findings, treatment (medical, percutaneous or surgical) and long-term outcome. Statistical data were expressed as percentages and absolute values.
ResultsAll eight patients were women, median age 49 years. Typical chest pain was present in 37.5%. Elevated ESR was observed in 85.7%. Three patients underwent coronary artery bypass grafting, three underwent percutaneous coronary angioplasty (two with bare-metal stents and one with a drug-eluting stent) and two were treated medically. In-hospital mortality was 25%. There were no deaths during a mean follow-up of 30 months.
ConclusionsIn our study, patients who were discharged home had good outcomes in long-term follow-up with medical, percutaneous or surgical treatment. ESR appears to be associated with ACS in TA.
A monitoração da atividade da doença e o melhor esquema terapêutico ainda têm sido um desafio em pacientes com arterite de Takayasu (AT). Em síndromes coronárias agudas (SCA) a melhor forma de tratamento intervencionista mantém-se indefinido. Dessa forma, descrevemos as características basais, manifestações clínicas, achados angiográficos, tratamento definitivo adotado e a evolução a longo prazo de pacientes com AT que apresentaram SCA.
MétodosEntre 2004 e 2010, foram analisados retrospectivamente 8 pacientes com AT que apresentaram SCA. As seguintes informações foram obtidas: idade, sexo, manifestações clínicas e eletrocardiográficas, estado hemodinâmico, fatores de risco para SCA, marcadores de necrose miocárdica, clearance de creatinina, fração de ejeção de ventrículo esquerdo, marcadores inflamatórios, medicações utilizadas, achados angiográficos, tratamento definitivo adotado e evolução a longo prazo.
ResultadosOs 8 pacientes eram mulheres. A mediana de idade foi 49 anos. Dor precordial típica esteve presente em 37,5%. Cerca de 85,7% apresentaram aumento de velocidade de hemossedimentação. O seguimento mais acometido foi o tronco da coronária esquerda em 62,5%. Em 3 casos optou-se por revascularização cirúrgica, em 2 pacientes realizou-se angioplastia com stent convencional, em 1 com stent farmacológico e em 2 doentes manteve-se tratamento clínico. Obteve-se mortalidade intra-hospitalar de 25% e em seguimento médio de 30 meses não houve mortes.
ConclusãoEm pacientes que sobreviveram ao quadro agudo e receberam alta hospitalar, bons resultados a longo prazo foram obtidos principalmente com tratamento clínico ou cirúrgico. A velocidade de hemossedimentação parece estar mais relacionada à ocorrência de quadros de SCA em pacientes com AT.
Takayasu arteritis (TA) is a chronic inflammatory disease of unknown etiology that affects large blood vessels, mainly the aorta and its main branches and the pulmonary and coronary vessels.1 Its rarity means that monitoring of disease activity and the best therapeutic approach are a challenge. When associated with acute coronary syndromes (ACS), the best interventional treatment has not been established. The results in case series of treatment by percutaneous transluminal coronary angioplasty (PTCA) and/or coronary artery bypass grafting (CABG) are inconsistent.1 Against this background, we describe the baseline characteristics, clinical manifestations, angiographic findings, treatment and long-term outcome of patients with TA and ACS.
MethodsWe retrospectively analyzed eight patients with TA and ACS (unstable angina or myocardial infarction [MI]) between 2004 and 2010. The diagnosis of TA was based on the 1990 criteria of the American College of Rheumatology (age at disease onset <40 years, difference in blood pressure between limbs >10 mmHg, bruit over aorta, arteriogram abnormality on arteriography, Doppler ultrasound or computed tomography (CT) angiography.1
All patients with typical chest pain were immediately classified as having ACS and stratified according to clinical presentation. Those with atypical pain and/or equivalent ischemic symptoms, such as dyspnea, were managed on the basis of a chest pain protocol, remaining under observation for 12hours with ECG and testing of markers of myocardial necrosis (troponin and CK-MB) every three hours. Those with ST-segment depression on the ECG and/or positive myocardial necrosis markers were diagnosed with ACS and thus included in the study. The three cases with typical chest pain had normal ECG and myocardial necrosis markers, while the other five, with atypical pain and/or dyspnea, had ECG alterations or positive necrosis markers.
The following data were obtained: age, gender, clinical and electrocardiographic manifestations, Killip class, risk factors for ACS, markers of myocardial necrosis (CK-MB and troponin), creatinine clearance, left ventricular ejection fraction, inflammatory markers (C-reactive protein and erythrocyte sedimentation rate [ESR]), medication during hospital stay, angiographic findings, treatment (medical, percutaneous or surgical) and long-term outcome.
Data were also acquired on anatomical arterial lesions detected by conventional and/or CT angiography. Stenosis of ≥70% was considered significant in both systemic and coronary vessels.
In cases of PTCA, the type of stent (bare-metal or drug-eluting) was recorded, as were types of arterial or venous grafts used in CABG.
Statistical analysisStatistical data were expressed as percentages and absolute values.
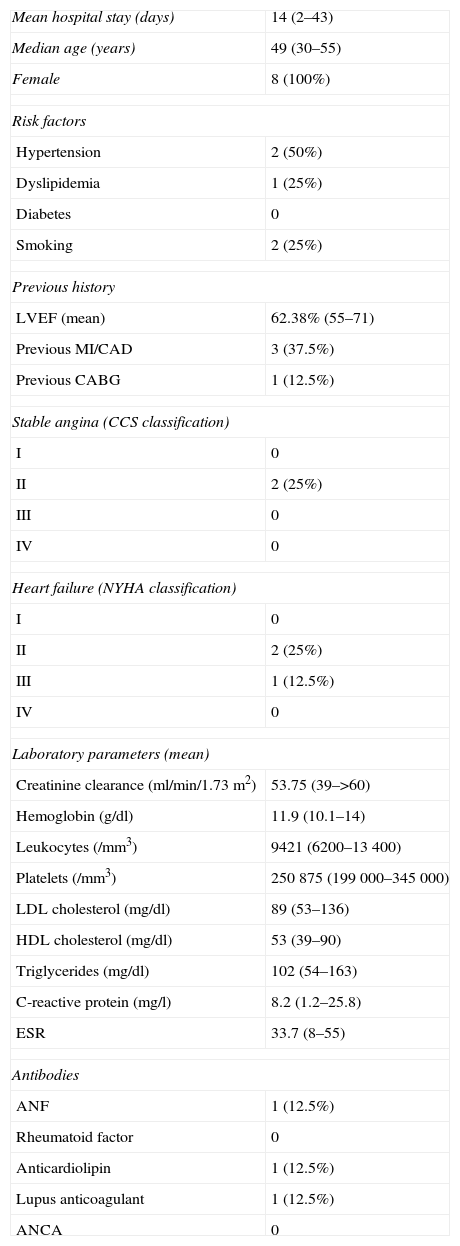
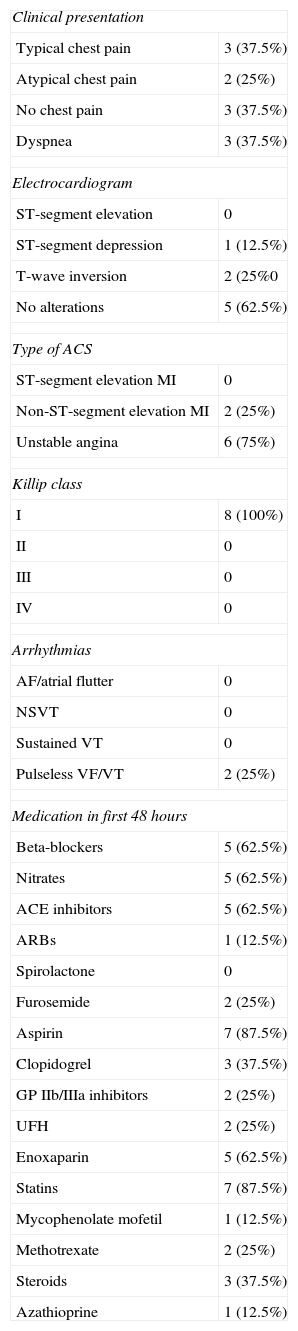
ResultsAll eight patients were women, median age 49 years. The baseline characteristics of the population are described in Table 1. The most common clinical presentation was unstable angina, in 75% of cases; the ECG was normal in 62.5% of cases (Table 2).
Baseline characteristics of the study population with Takayasu arteritis and acute coronary syndrome.
| Mean hospital stay (days) | 14 (2–43) |
| Median age (years) | 49 (30–55) |
| Female | 8 (100%) |
| Risk factors | |
| Hypertension | 2 (50%) |
| Dyslipidemia | 1 (25%) |
| Diabetes | 0 |
| Smoking | 2 (25%) |
| Previous history | |
| LVEF (mean) | 62.38% (55–71) |
| Previous MI/CAD | 3 (37.5%) |
| Previous CABG | 1 (12.5%) |
| Stable angina (CCS classification) | |
| I | 0 |
| II | 2 (25%) |
| III | 0 |
| IV | 0 |
| Heart failure (NYHA classification) | |
| I | 0 |
| II | 2 (25%) |
| III | 1 (12.5%) |
| IV | 0 |
| Laboratory parameters (mean) | |
| Creatinine clearance (ml/min/1.73m2) | 53.75 (39–>60) |
| Hemoglobin (g/dl) | 11.9 (10.1–14) |
| Leukocytes (/mm3) | 9421 (6200–13400) |
| Platelets (/mm3) | 250875 (199000–345000) |
| LDL cholesterol (mg/dl) | 89 (53–136) |
| HDL cholesterol (mg/dl) | 53 (39–90) |
| Triglycerides (mg/dl) | 102 (54–163) |
| C-reactive protein (mg/l) | 8.2 (1.2–25.8) |
| ESR | 33.7 (8–55) |
| Antibodies | |
| ANF | 1 (12.5%) |
| Rheumatoid factor | 0 |
| Anticardiolipin | 1 (12.5%) |
| Lupus anticoagulant | 1 (12.5%) |
| ANCA | 0 |
ANCA: antineutrophil cytoplasmic antibody; ANF: antinuclear factor; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CCS: Canadian Cardiovascular Society; ESR: erythrocyte sedimentation rate; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NYHA: New York Heart Association.
Clinical and electrocardiographic characteristics of the study population with Takayasu arteritis and acute coronary syndrome.
| Clinical presentation | |
| Typical chest pain | 3 (37.5%) |
| Atypical chest pain | 2 (25%) |
| No chest pain | 3 (37.5%) |
| Dyspnea | 3 (37.5%) |
| Electrocardiogram | |
| ST-segment elevation | 0 |
| ST-segment depression | 1 (12.5%) |
| T-wave inversion | 2 (25%0 |
| No alterations | 5 (62.5%) |
| Type of ACS | |
| ST-segment elevation MI | 0 |
| Non-ST-segment elevation MI | 2 (25%) |
| Unstable angina | 6 (75%) |
| Killip class | |
| I | 8 (100%) |
| II | 0 |
| III | 0 |
| IV | 0 |
| Arrhythmias | |
| AF/atrial flutter | 0 |
| NSVT | 0 |
| Sustained VT | 0 |
| Pulseless VF/VT | 2 (25%) |
| Medication in first 48hours | |
| Beta-blockers | 5 (62.5%) |
| Nitrates | 5 (62.5%) |
| ACE inhibitors | 5 (62.5%) |
| ARBs | 1 (12.5%) |
| Spirolactone | 0 |
| Furosemide | 2 (25%) |
| Aspirin | 7 (87.5%) |
| Clopidogrel | 3 (37.5%) |
| GP IIb/IIIa inhibitors | 2 (25%) |
| UFH | 2 (25%) |
| Enoxaparin | 5 (62.5%) |
| Statins | 7 (87.5%) |
| Mycophenolate mofetil | 1 (12.5%) |
| Methotrexate | 2 (25%) |
| Steroids | 3 (37.5%) |
| Azathioprine | 1 (12.5%) |
ACS: acute coronary syndrome; ACE: angiotensin-converting enzyme; AF: atrial fibrillation; ARBs: angiotensin receptor blockers; GP: glycoprotein; MI: myocardial infarction; NSVT: nonsustained ventricular tachycardia; UFH: unfractionated heparin; VF: ventricular fibrillation; VT: ventricular tachycardia.
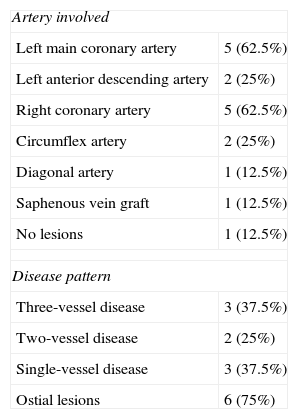
The vessels most affected were the subclavian and renal arteries in 62.5% of cases, followed by the carotid arteries and aorta in 50% and the iliac arteries in 25%. Of the coronary arteries, the segments most affected were the left main and the right coronary artery in 62.5% of cases, followed by the left anterior descending and circumflex arteries in 25% of patients. In one case (12.5%) no obstructive coronary lesions were detected. Ostial lesions were observed in 75% of patients. There were three cases (37.5%) of three-vessel disease and two (25%) of two-vessel disease (Table 3).
Angiographic characteristics of the study population with Takayasu arteritis and acute coronary syndrome.
| Artery involved | |
| Left main coronary artery | 5 (62.5%) |
| Left anterior descending artery | 2 (25%) |
| Right coronary artery | 5 (62.5%) |
| Circumflex artery | 2 (25%) |
| Diagonal artery | 1 (12.5%) |
| Saphenous vein graft | 1 (12.5%) |
| No lesions | 1 (12.5%) |
| Disease pattern | |
| Three-vessel disease | 3 (37.5%) |
| Two-vessel disease | 2 (25%) |
| Single-vessel disease | 3 (37.5%) |
| Ostial lesions | 6 (75%) |
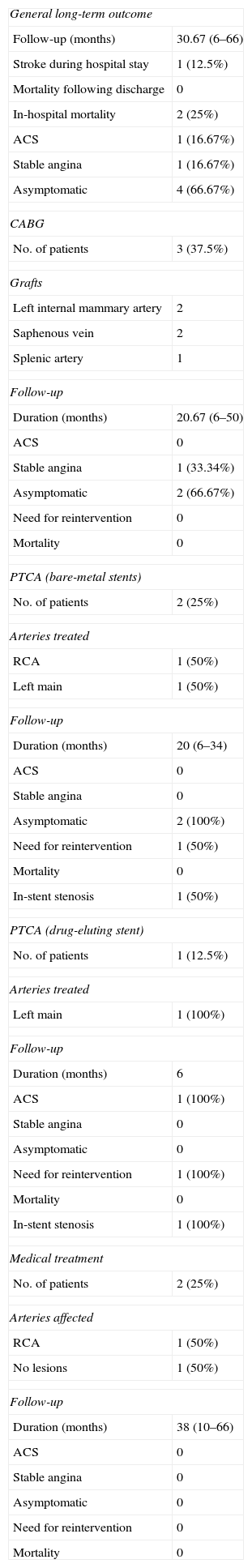
Three patients were treated by CABG, three by PTCA (two with bare-metal stents and one with a drug-eluting stent), and two were treated medically. In-hospital mortality was 25% and there were no deaths during a mean follow-up of 30 months. One patient treated by CABG presented stable angina without needing reintervention and one case treated by PTCA with a bare-metal stent underwent reintervention due to unstable angina (Table 4).
Treatment and long-term outcome of the study population with Takayasu arteritis and acute coronary syndrome.
| General long-term outcome | |
| Follow-up (months) | 30.67 (6–66) |
| Stroke during hospital stay | 1 (12.5%) |
| Mortality following discharge | 0 |
| In-hospital mortality | 2 (25%) |
| ACS | 1 (16.67%) |
| Stable angina | 1 (16.67%) |
| Asymptomatic | 4 (66.67%) |
| CABG | |
| No. of patients | 3 (37.5%) |
| Grafts | |
| Left internal mammary artery | 2 |
| Saphenous vein | 2 |
| Splenic artery | 1 |
| Follow-up | |
| Duration (months) | 20.67 (6–50) |
| ACS | 0 |
| Stable angina | 1 (33.34%) |
| Asymptomatic | 2 (66.67%) |
| Need for reintervention | 0 |
| Mortality | 0 |
| PTCA (bare-metal stents) | |
| No. of patients | 2 (25%) |
| Arteries treated | |
| RCA | 1 (50%) |
| Left main | 1 (50%) |
| Follow-up | |
| Duration (months) | 20 (6–34) |
| ACS | 0 |
| Stable angina | 0 |
| Asymptomatic | 2 (100%) |
| Need for reintervention | 1 (50%) |
| Mortality | 0 |
| In-stent stenosis | 1 (50%) |
| PTCA (drug-eluting stent) | |
| No. of patients | 1 (12.5%) |
| Arteries treated | |
| Left main | 1 (100%) |
| Follow-up | |
| Duration (months) | 6 |
| ACS | 1 (100%) |
| Stable angina | 0 |
| Asymptomatic | 0 |
| Need for reintervention | 1 (100%) |
| Mortality | 0 |
| In-stent stenosis | 1 (100%) |
| Medical treatment | |
| No. of patients | 2 (25%) |
| Arteries affected | |
| RCA | 1 (50%) |
| No lesions | 1 (50%) |
| Follow-up | |
| Duration (months) | 38 (10–66) |
| ACS | 0 |
| Stable angina | 0 |
| Asymptomatic | 0 |
| Need for reintervention | 0 |
| Mortality | 0 |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; PTCA: percutaneous transluminal coronary angioplasty; RCA: right coronary artery.
TA mainly affects women (90% of cases) aged between 10 and 40 years. In the literature some form of coronary disease is reported in 6–30% of patients with TA.1–4 Its pathogenesis is not fully understood; it is thought to result from chronic autoimmune inflammation of the large arteries, although other factors, including infectious agents and genetic predisposition, may also be involved. The disease develops in two stages: an initial phase characterized by elevation of inflammatory markers, followed by a chronic phase with vascular damage.3
It is not known exactly when coronary lesions appear. Most studies show a correlation between ACS and elevated inflammatory markers such as C-reactive protein and ESR.1 However, some case reports have shown no direct relationship between active inflammation and coronary symptoms.5 In our series, elevated C-reactive protein was observed in 50% of patients and elevated ESR in 87%, suggesting that the latter is more strongly associated with ACS in patients with TA.
Clinical manifestations range from stable angina to MI, and must be promptly diagnosed in order to begin immunosuppressive therapy together with appropriate cardiological treatment, which will improve prognosis.4 The few case reports in the literature indicate that myocardial ischemia is one of the main causes of death in TA, with mortality of up to 50% at five years.3 Only three patients in our series (37.5%) had typical chest pain, while five (62.5%) had no ECG alterations suggesting acute ischemia. Only two patients (25%) were diagnosed with MI, most being categorized as having unstable angina. In-hospital mortality was 25%, in both cases due to cardiogenic shock. There were no deaths during a mean follow-up of 30 months, in contrast to the mortality reported in the literature, although the small sample size makes comparisons difficult. The high in-hospital mortality may have been due to the severity of cases with ostial lesions in the left main coronary artery. The low long-term mortality may be partly due to better control of TA-related inflammation following ACS.
Ostial lesions in the right and left coronary arteries are the most common findings, in 87.5% of TA cases with coronary involvement. In these diseased vessels, luminal narrowing is caused by extension of intimal proliferation and contraction of the fibrotic media and adventitia from the ascending aorta. Ostial involvement was found in 75% of our patients, in agreement with the literature. However, lesions may also occur in more distal segments, the chronic inflammation found in TA accelerating the development of atherosclerosis, as seen in 50% of the patients in our series.4 Diagnosis is usually based on clinical features and cine coronary angiography, although recent studies have demonstrated excellent results with CT angiography in TA.4
Implantation of bare-metal stents in patients with TA is followed by restenosis in up to 78% of cases. In the few reports of drug-eluting stents being used in this population, short- and long-term restenosis rates are also high, casting doubt on their effectiveness in these patients. Some authors suggest that drug-eluting stents are only useful as a bridge while immunosuppression is optimized and until CABG can be performed.2,4,6,7 Yokota et al.,4 reported the case of a 52-year-old woman who underwent PTCA of the left anterior descending artery four times using drug-eluting stents. Restenosis occurred three times, the problem only being overcome after the fourth intervention; the authors considered that vessel patency was preserved due to the addition of steroid therapy at that time.4,8 In our series in-stent restenosis occurred in one of two cases even with only mild inflammatory activity, further fueling the debate over which type of stent to use in these patients. Once again, the small study population severely limits the ability to establish correlations between stent use and outcome.
The best type of graft for CABG has yet to be established for these patients, and the presence of ostial lesions of the aorta and possible involvement of the subclavian arteries makes the decision more complex. Unlike most CABG procedures, saphenous vein grafts are generally used in TA patients, except in cases of severe aortic calcification. Survival with saphenous vein-to-left anterior descending artery grafting is 80% at 10 years, with event-free survival of 77%. Internal mammary in-situ grafts are not totally contraindicated but should be avoided, and if used should be preceded by imaging studies of the subclavian arteries to ensure their patency.1,9 In two cases in our series in which left internal mammary artery in-situ grafts were used, the patients were still asymptomatic after 20 months. Only one saphenous vein graft lesion was detected, which did not require reintervention.
ConclusionCoronary involvement in TA is rare but extremely serious due to the complexity of the lesions. Knowledge of patients’ clinical, ECG, angiographic and hemodynamic characteristics is essential to decide on the best form of treatment, but this is still the subject of debate given the paucity of cases reported. In our study, patients who survived the acute phase and were discharged home had good long-term outcomes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: de Matos Soeiro A, et al. Características clínicas, angiográficas e evolução a longo prazo em pacientes com arterite de Takayasu e síndrome coronária aguda. Rev Port Cardiol. 2013. http://dx.doi.org/10.1016/j.repc.2012.06.020.