The high prevalence and natural history of atherosclerosis make young people important targets for cardiovascular prevention. This study aimed to analyze changes over time in the cardiovascular risk profile of a population of healthy young adults.
MethodsWe studied 923 Portuguese Air Force applicants between 1991 and 2007, divided into two-year periods. In addition to cardiovascular risk factors, the Framingham score and HeartScore were calculated for age 65. Cochran-Armitage and Jonckheere-Terpstra tests for trend were used for categorical and continuous variables, respectively.
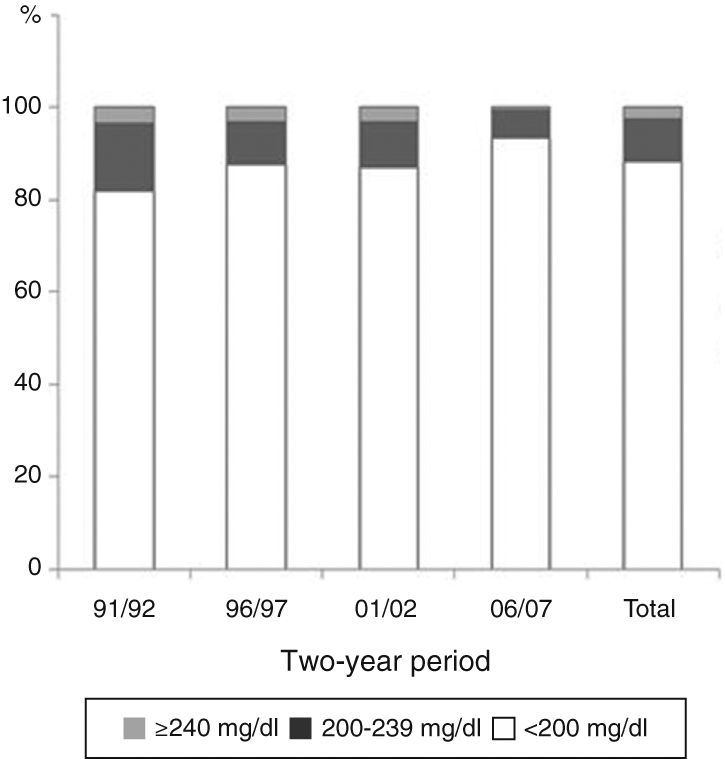
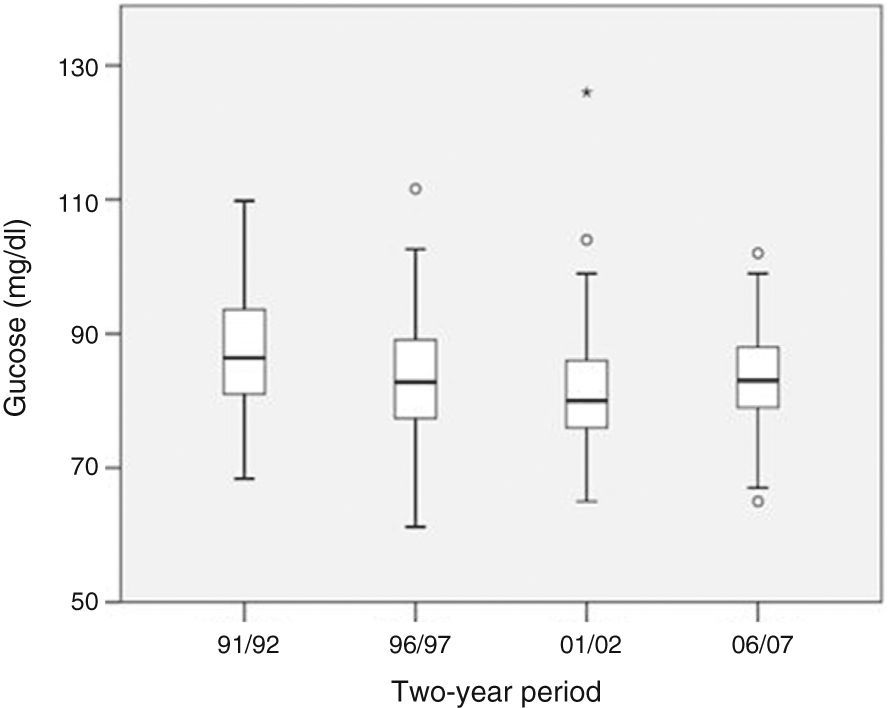
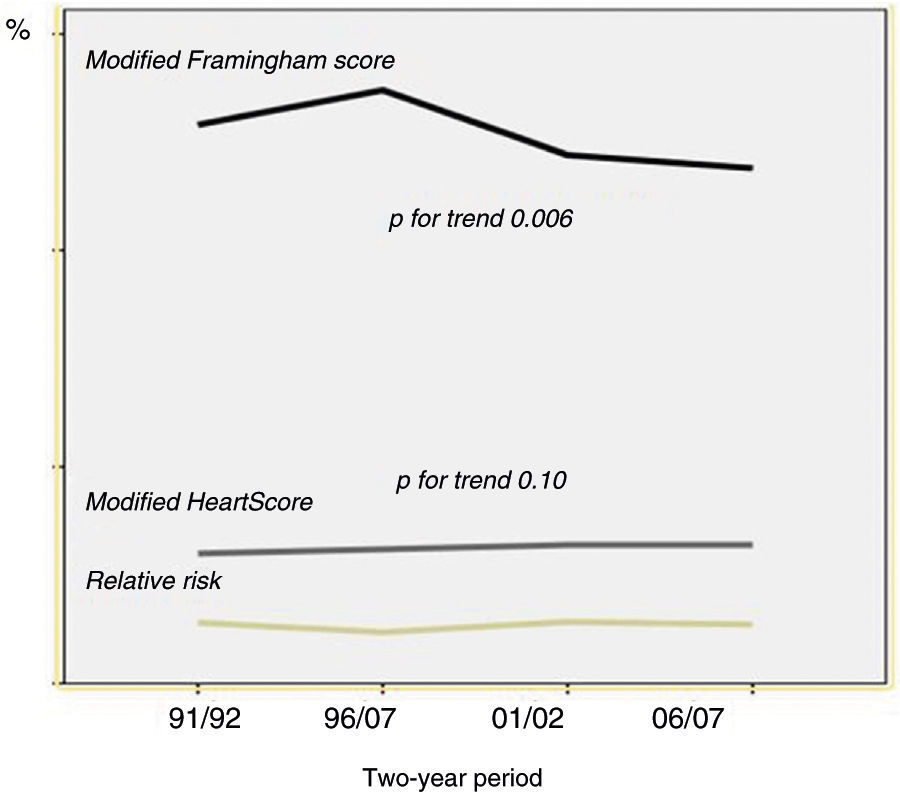
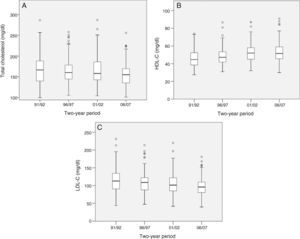
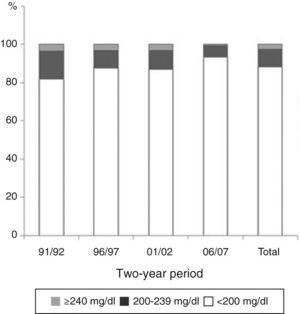
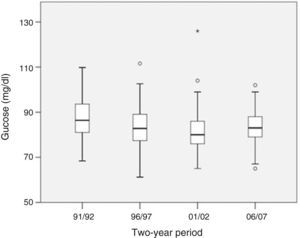
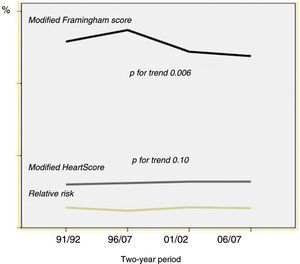
ResultsMean age was 19.2±2.3 years (p=0.34) and 55 applicants (6%) were female (p=0.56). Mean body mass index was 22.4±2.5 kg (p for trend 0.35). The number of smokers decreased over the study period (11.6 vs. 7.0%, p for trend 0.02). Of the total number of applicants, 122 (13.2%) were classified as hypertensive. Mean systolic blood pressure was 127±12 mmHg and increased significantly over time (122±13 vs. 128±11 mmHg, p for trend <0.001). Hypercholesterolemia was found in 108 applicants (11.7%) and total cholesterol showed an improvement (170±35 vs. 155±26 mg/dl, p for trend <0.001). The mean modified Framingham score was 12.6±5.1 and improved over the study period (12.9±5.9% vs. 11.9±4.7%, p for trend 0.006). The mean modified HeartScore was 3.2±1.4 and remained unchanged (p for trend 0.10).
ConclusionsIn our population, except for an increase in systolic blood pressure values, there was an overall improvement in cardiovascular risk from 1991 to 2007. Further studies are needed to better assess the situation in Portugal and help devise preventive strategies in young people.
A elevada prevalência e a história natural da doença aterosclerótica tornam os jovens um alvo importante da prevenção cardiovascular. O objetivo deste trabalho foi caracterizar a evolução temporal do perfil de risco cardiovascular de uma população de adultos jovens saudáveis.
MétodosForam estudados retrospetivamente 923 candidatos às especialidades aeronáuticas da Força Aérea, entre 1991-2007, divididos por biénios. Avaliaram-se os fatores de risco cardiovascular, score de Framingham e HeartScore, para uma idade modificada de 65 anos. Utilizaram-se os testes de Cochran-Armitage e de Jonckheere-Terpstra para tendência, em variáveis categóricas e contínuas, respetivamente.
ResultadosA idade média foi de 19,2±2,3 anos (p=0,34) e 55 (6%) dos candidatos eram do sexo feminino (p=0,56). O índice de massa corporal médio foi de 22,4±2,5 kg/m2 (p para tendência=0,35). O número de fumadores decresceu ao longo dos biénios (11,6 versus 7,0%, p para tendência=0,02). Cento e vinte e dois (13,2%) dos candidatos eram hipertensos. A pressão arterial sistólica média foi de 127±12 mmHg, observando-se um aumento temporal significativo (122±13 versus 128±11 mmHg, p para tendência <0,001). Cento e oito (11,7%) dos candidatos tinham hipercolesterolemia e o colesterol total melhorou (170±35 mg/dL versus 155±26 mg/dL, p para tendência <0,001). O score de Framingham modificado médio foi de 12,6±5,1 e melhorou ao longo dos biénios (12,9±5,9% versus 11,9±4,7%, p para tendência=0,006), não se observando alterações no valor médio do HeartSCORE modificado (3,2±1,4, p para tendência=0,10).
ConclusõesNa população estudada, excetuando os valores da pressão arterial sistólica, registou-se uma melhoria global do nível de risco cardiovascular entre 1991-2007. São necessários mais estudos para um melhor conhecimento da realidade portuguesa e otimização de estratégias preventivas nesta faixa etária.
Statistics for the last decade show that atherosclerotic cardiovascular (CV) disease is still the leading cause of death in Portugal, accounting for 31.9% of mortality in 2009.1 Despite a progressive decline in mortality rates from both coronary artery disease (CAD) and stroke, absolute numbers of deaths attributable to CV disease remain high and justify ongoing preventive measures.1,2
The subclinical stage of the atherosclerotic process begins long before the average age of symptom onset, as demonstrated by various autopsy studies that show an association between number of CV risk factors and severity of asymptomatic coronary and aortic lesions in adolescents and young adults.3,4 Despite these results, there have been few studies on CV risk in the young, particularly using risk scores.
Against this background, the aim of this study was to analyze recent changes in the main CV risk factors in a population of healthy young adults and to classify their risk through validated scores, namely the HeartScore and Framingham scores.
MethodsPopulation and study designThis was an observational, descriptive, retrospective study of 923 Portuguese Air Force applicants between 1991 and 2007, for four two-year periods – 1991/2, 1996/7, 2001/2 and 2006/7.
Study variablesThe following variables were analyzed: age, gender, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting glucose (in mg/dl), total cholesterol (in mg/dl), LDL cholesterol (in mg/dl), HDL cholesterol (in mg/dl), and smoking (any tobacco consumption in the previous year). Blood pressure was measured using a mercury sphygmomanometer after a five-minute rest period, readings being taken on the right arm with the subject seated. Plasma glucose and lipids were quantified in the Portuguese Air Force laboratory using an automated method.
Risk scoresThe Framingham online calculator was used to determine the score for 10-year absolute risk of CAD.5 The HeartScore was calculated using the model for 10-year absolute risk of CV mortality in a low-risk population, based on the following variables: age, gender, SBP, smoking and total cholesterol.6 In accordance with the latest version of the European Society of Cardiology (ESC) guidelines on cardiovascular disease prevention, the HeartScore was also calculated after inclusion of HDL cholesterol.8 The Framingham score includes diabetes as well as the above variables.
The lower age limit for both scores is 30, and so absolute risk was calculated for age 65, an option described in previous publications.7 In the light of recommendations in the latest European guidelines for CV disease prevention in the young, relative risk was also calculated.8
Statistical analysisIBM SPSS Statistics version 21.0 was used to analyze the data. For each two-year period, categorical variables were analyzed using a chi-square test for trend (Cochran-Armitage test), for a 5% level of significance. The Jonckheere-Terpstra test for trend was used to test the null hypothesis of no significant difference between the means of the continuous variables, for a 5% level of significance.
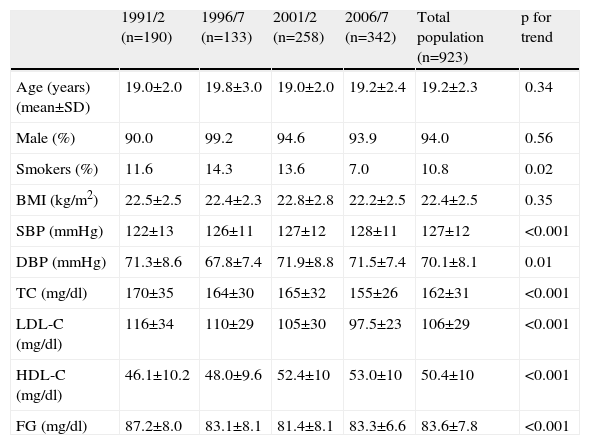
ResultsThe mean age of the study population (n=923) was 19.2±2.3 years, and 55 (6%) were female. The age and gender distributions did not vary significantly over the years (p for trend 0.34 and 0.56, respectively) (Table 1).
Demographic and clinical variables.
| 1991/2 (n=190) | 1996/7 (n=133) | 2001/2 (n=258) | 2006/7 (n=342) | Total population (n=923) | p for trend | |
| Age (years) (mean±SD) | 19.0±2.0 | 19.8±3.0 | 19.0±2.0 | 19.2±2.4 | 19.2±2.3 | 0.34 |
| Male (%) | 90.0 | 99.2 | 94.6 | 93.9 | 94.0 | 0.56 |
| Smokers (%) | 11.6 | 14.3 | 13.6 | 7.0 | 10.8 | 0.02 |
| BMI (kg/m2) | 22.5±2.5 | 22.4±2.3 | 22.8±2.8 | 22.2±2.5 | 22.4±2.5 | 0.35 |
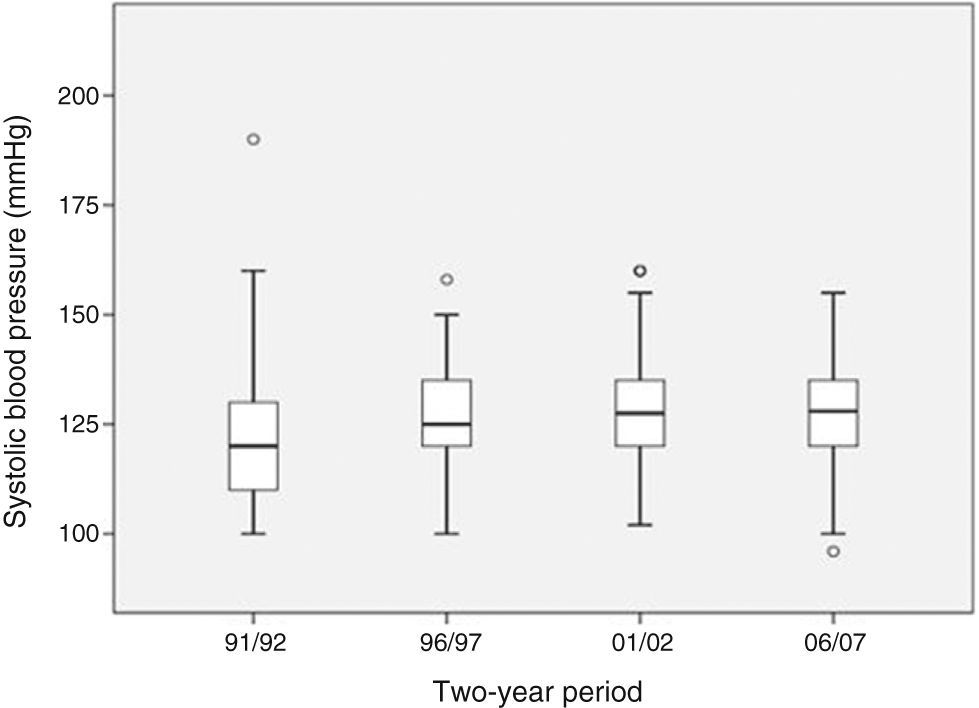
| SBP (mmHg) | 122±13 | 126±11 | 127±12 | 128±11 | 127±12 | <0.001 |
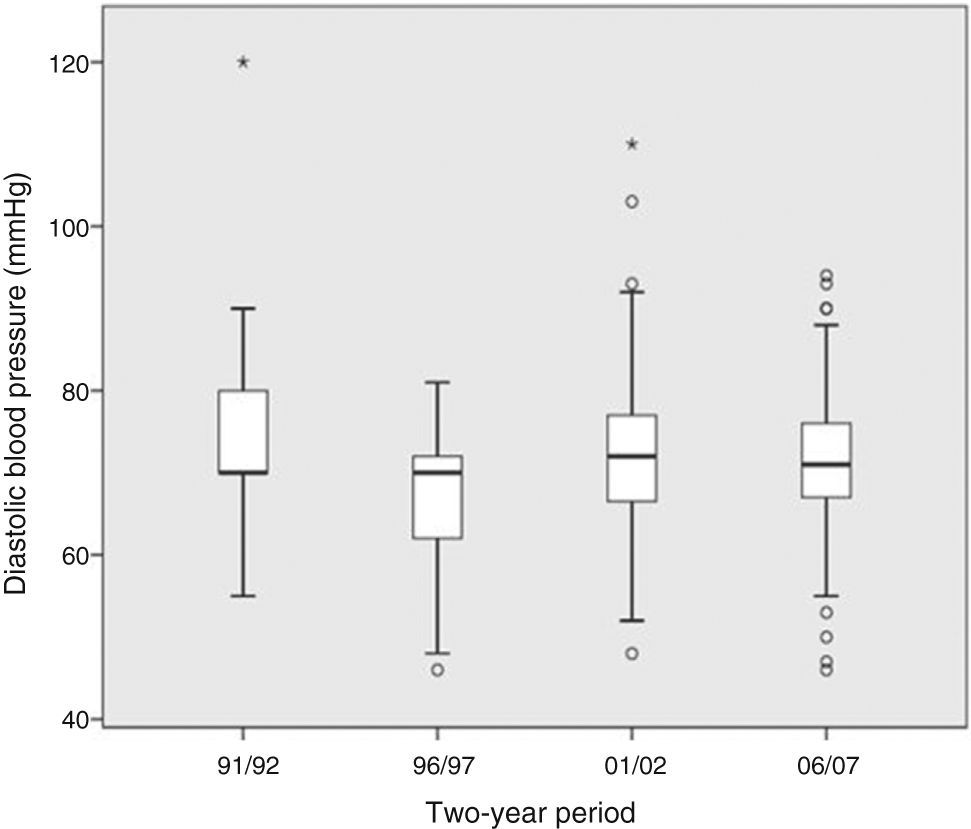
| DBP (mmHg) | 71.3±8.6 | 67.8±7.4 | 71.9±8.8 | 71.5±7.4 | 70.1±8.1 | 0.01 |
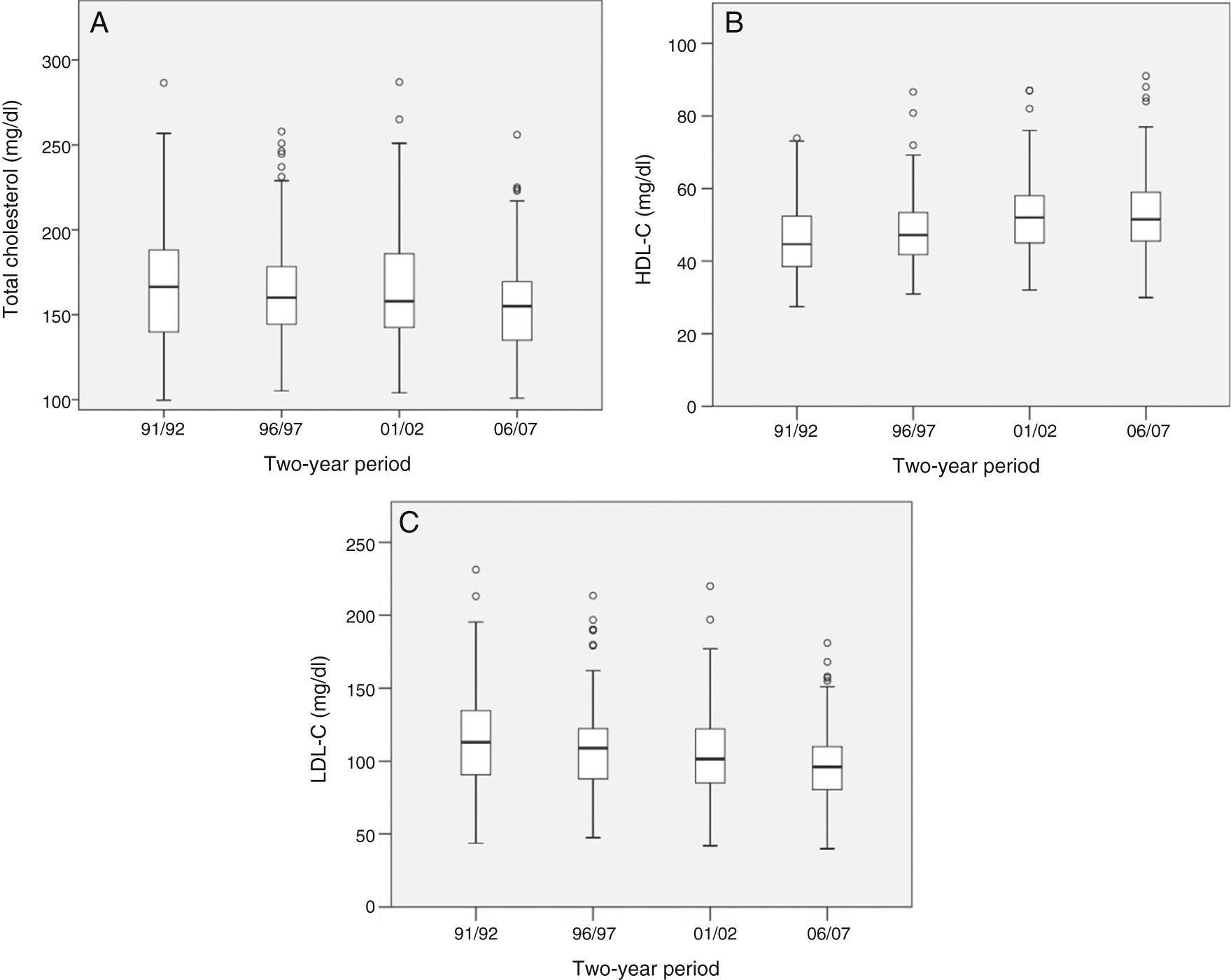
| TC (mg/dl) | 170±35 | 164±30 | 165±32 | 155±26 | 162±31 | <0.001 |
| LDL-C (mg/dl) | 116±34 | 110±29 | 105±30 | 97.5±23 | 106±29 | <0.001 |
| HDL-C (mg/dl) | 46.1±10.2 | 48.0±9.6 | 52.4±10 | 53.0±10 | 50.4±10 | <0.001 |
| FG (mg/dl) | 87.2±8.0 | 83.1±8.1 | 81.4±8.1 | 83.3±6.6 | 83.6±7.8 | <0.001 |
BMI: body mass index; DBP: diastolic blood pressure; FG: fasting glucose; HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; SBP: systolic blood pressure; TC: total cholesterol.
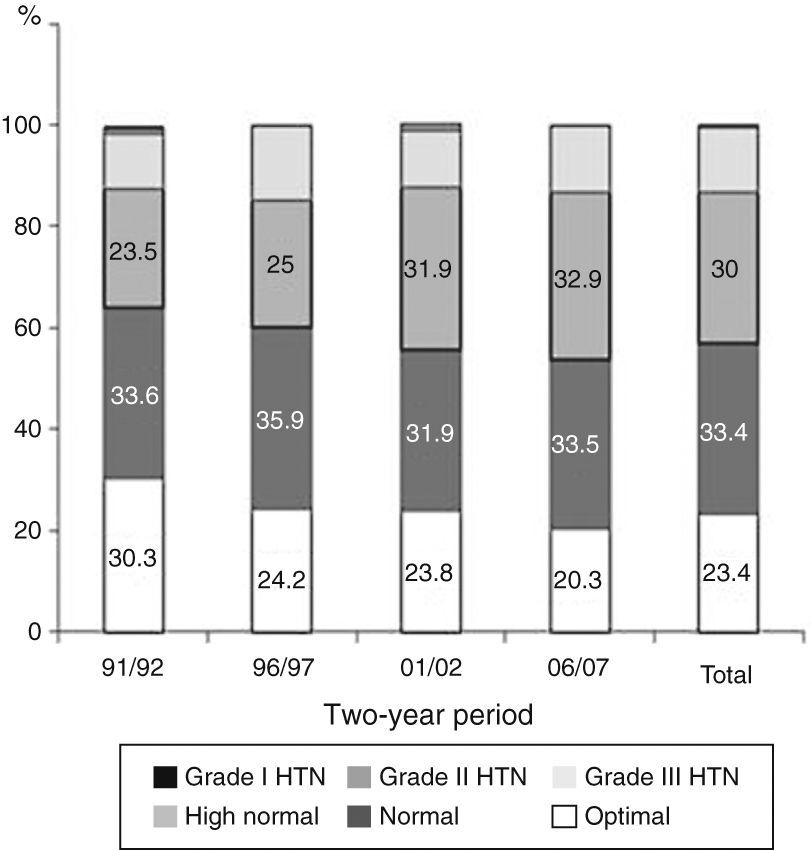
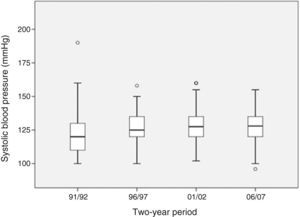
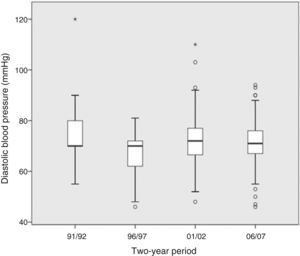
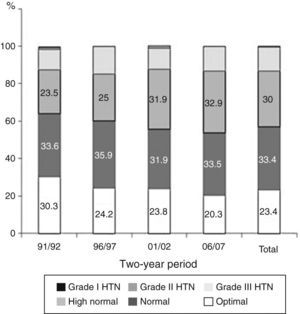
The proportion of smokers decreased significantly between 1991 and 2007 (p=0.02), the overall percentage being 10.8%. BMI remained relatively constant over the years, with a mean value for the total population of 22.4±2.5 kg/m2 (p for trend 0.35), with around 95% having a BMI within the normal range. With regard to blood pressure, we found a mean overall value for SBP of 127±12 mmHg, with an increase throughout the study period (p for trend <0.001) (Figure 1), while a significant decrease was seen in DBP (p for trend 0.011) (Figure 2). According to the ESC classification,8 23.4% of the 923 individuals had optimal blood pressure, 33.4% normal, 30% normal-high, and 12.6% grade I hypertension, 0.5% grade II and 0.1% grade III (Figure 3).
An improvement in plasma lipid profile was observed (Figure 4), as reflected in decreased total cholesterol (p for trend <0.001) and LDL cholesterol (p for trend <0.001) and increased HDL cholesterol (p for trend <0.001). The overall prevalence of hypercholesterolemia was 11.7% (Figure 5) based on the National Cholesterol Education Program – Adult Treatment Panel III (NCEP-ATP III) definition.9
There was a significant reduction in fasting glucose (p for trend <0.001) (Figure 6). Only one individual in the study population presented fasting glucose ≥126 mg/dl, which would indicate a diagnosis of type 2 diabetes if confirmed on a second assessment, in accordance with the International Diabetes Federation criteria.10 Eleven (1.2%) had fasting glucose between 100 mg/dl and 126 mg/dl, indicating impaired fasting glucose.
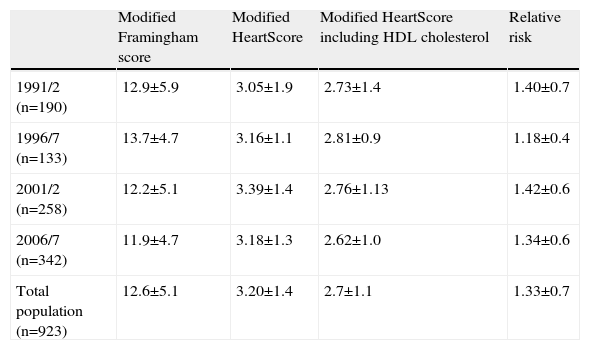
The overall mean modified Framingham score (Table 2 and Figure 7) was 12.6±5.1, with a statistically significant decrease over the study period (p for trend 0.006). The final modified HeartScore was 3.20±1.4 (intermediate risk) with no significant variation over time (p for trend 0.10). When HDL cholesterol was included, the HeartScore was lower (overall mean value 2.72±1.1), but no significant change was observed over time (p for trend 0.078). The mean relative risk based on the HeartScore was 1.33±0.7 for the total population (p for trend 1.0).
Changes over time in the mean modified Framingham score, modified HeartScore, modified HeartScore including HDL cholesterol, and relative risk.
| Modified Framingham score | Modified HeartScore | Modified HeartScore including HDL cholesterol | Relative risk | |
| 1991/2 (n=190) | 12.9±5.9 | 3.05±1.9 | 2.73±1.4 | 1.40±0.7 |
| 1996/7 (n=133) | 13.7±4.7 | 3.16±1.1 | 2.81±0.9 | 1.18±0.4 |
| 2001/2 (n=258) | 12.2±5.1 | 3.39±1.4 | 2.76±1.13 | 1.42±0.6 |
| 2006/7 (n=342) | 11.9±4.7 | 3.18±1.3 | 2.62±1.0 | 1.34±0.6 |
| Total population (n=923) | 12.6±5.1 | 3.20±1.4 | 2.7±1.1 | 1.33±0.7 |
Cardiovascular disease prevention should ideally begin in pregnancy and continue throughout life.8 Ever earlier exposure to CV risk factors and their tendency to accumulate and persist into adulthood, together with increased life expectancy, make young people important targets for preventive measures.8,13–15
The results of our study showed improvements in levels of smoking, lipid profile, BMI and fasting glucose over a 16-year period, and the modified Framingham score fell significantly. These favorable results are in line with the reduction in CV mortality observed in the Portuguese population in recent years.1
Various studies have documented advanced atheromatous lesions of the coronary vasculature in young adults. The PDAY study showed a 2% prevalence of advanced coronary lesions in young Americans aged 20–24 years,4 and Berenson et al. had previously demonstrated in the Bogalusa Heart Study that such lesions were associated with a higher number of CV risk factors.3
In Portugal, studies on the prevalence of hypertension, diabetes, smoking, dyslipidemia and obesity in the general population show that there is room for improvement.16–22 The VALSIM study estimated the prevalence of hypertension in the 18–29 age-group at 6.7%,16 while, surprisingly, in our study population it was nearly double that figure at 13.1%, most of whom had grade I hypertension, with a statistically significant increase throughout the study period. In a similar study of 508 Spanish military cadets aged 17–23 (the AGEMZA study) comparing the periods 1985–87 and 2000–03, mean SBP was 125±15 mmHg, with no difference between the groups, close to the 126±11 mmHg observed in our sample.23 According to Espiga de Macedo et al., mean SBP and DBP in Portuguese men aged 18–24 were 130 mmHg and 73 mmHg, respectively.24 However, even in those with so-called normal blood pressure there is scope for risk reduction, since differences in risk for vascular mortality have been found for values as low as 115/75 mmHg.25
Improvements in lipid profile were seen in total, LDL and HDL cholesterol throughout the study period. However, it should be noted that there is a certain amount of heterogeneity between Portuguese studies, partly explained by the different cut-offs used to define hypercholesterolemia.21 According to data from a 2010 study of Portuguese schoolchildren aged 15–18 years,26 mean total cholesterol in the 18-year-olds was 159 mg/dl, and 5% were classified as hypercholesterolemic (≥190 mg/dl). In our population, median total cholesterol was 162 mg/dl, with a 14.4% prevalence of hypercholesterolemia. In the AGEMZA study, median LDL and HDL cholesterol were 90.4±27 mg/dl and 56.1±11 mg/dl, respectively, in contrast to the 106±29 mg/dl and 50.4±10 mg/dl observed in our population, although lipid profile worsened over the course of the study.23 The latest data for the US population aged 6–19 years show a similar trend to our study, with decreases in total and LDL cholesterol and an increase in HDL cholesterol between 1988 and 2010.27
We found a low prevalence of obesity (0.7%), with mean BMI remaining stable over the study period, in contrast to a study by Padez et al., which reported an overall prevalence of 4.2% (obesity defined as BMI >30 kg/m2) and an increase in the number of obese men between 1996 and 2000 among Portuguese military conscripts.28
The blood glucose profile of the study population was favorable. Besides a significant decrease in fasting glucose levels between the first and the other periods, the prevalences of impaired fasting glucose and diabetes were 1.2% and 0.1%, respectively. The Portuguese PREVADIAB study (2009) showed prevalences of diabetes and impaired fasting glucose in the 20–39 age-group of 2.4% and 1.7%, respectively, similar to the results of the VALSIM study,17,18 although the wider age-range limits comparisons.
The significant decrease in the number of smokers over the study period contrasts with the trend seen among the general Portuguese population aged 15–24 years, in whom smoking prevalence increased between 1994 and 200620 from 26.6% to 31.4%, around three times higher than in our total population.
Control of modifiable CV risk factors is responsible for 44–76% of the reduction in mortality attributable to CAD, and has a greater impact than pharmacological therapy.11 While there has been a reduction in CAD mortality in the general US population, a study by Ford et al. showed that this trend has slowed and even reversed among those aged 35–54 years, and that mortality in this age-group rose between 1980 and 2002.12
The epidemiological importance of CV risk factors is related to the number of factors present, their severity and their persistence over time.3 The Framingham study, besides identifying CV risk factors, was the first to suggest that they tend to occur together.15 This clustering strengthens the effect of each risk factor on its own and increases overall CV risk.14 Their persistence over time and the relatively slow progression of CV disease are the rationale for the use of risk scores that include these factors to predict events and CV mortality, and that are now the basis for diagnostic and therapeutic strategies. The first model to stratify global risk of CV morbidity and mortality was based on the initial Framingham cohort.15 However, the cohort did not include individuals aged under 30, and furthermore the absolute risk calculated by the Framingham score is inevitably low, since it does not take account of a combination of factors that would place an individual in a higher risk category. For almost all combinations of CV risk factors, even with extreme values, non-smoking men aged under 45 and essentially all women aged under 65 have 10-year predicted risks below 10%.29
The more recent HeartScore, based on data on over 200 000 Europeans, although still subject to the same limitation in terms of absolute risk, estimates the relative risk of a young individual in relation to that of someone with an ideal risk profile, enabling improved assessment, communication and awareness of risk in this population.30,31
Although the age selected for risk projection in our study was older than the 60 years proposed by De Backer et al.,7 it corresponds to the upper age limit of the HeartScore risk tables and is thus the age of maximum risk. It is however a subjective cut-off and not ideal as an individual's risk will change over time.7,31 An alternative approach is to determine lifetime risk, which is a better measure of true risk and helps overcome the limitation of the influence of age. However, this method has not yet proved sufficiently reliable for use in everyday clinical practice.26,30
Based on the cut-offs for both the modified Framingham score and HeartScore, all of our study population were in the intermediate risk category (10–20% and 1–5%, respectively). Although it led to lower scores, the inclusion of HDL cholesterol in the HeartScore did not result in positive changes over the study period. Only the modified Framingham score identified a reduction in risk profile over time, although its significance is difficult to assess, since the finding may be related to its greater ability to detect differences and to predict nonfatal events rather than simply mortality, and to the fact that it includes fasting glucose. Based on the calculated risk, an average individual from this population would not require immediate treatment (for hypercholesterolemia, for example), even at age 65. The relative risk was so low that further stratification was not possible.
Of all the CV risk factors analyzed, only SBP showed an unfavorable change over time, contrasting with the improvements in lipid profile, fasting glucose, BMI, smoking and DBP. However, other studies on blood pressure changes in the young have also shown conflicting results.32,33 It is known that isolated systolic hypertension in young adults may not have prognostic significance or imply a higher risk of developing hypertension when central blood pressure is low, but merely reflects peripheral amplification of pulse waves.34 Nevertheless, hypertension is a major health problem in Portugal and its prevalence among the young should not be disregarded.35 One possible reason may be the high salt content of the Portuguese diet, which is double that recommended by the World Health Organization.36
The present study has certain limitations. The population was small and women were under-represented. The sample may have had a more favorable risk profile than that of an unselected population of young Portuguese adults, particularly in terms of obesity and smoking, making extrapolation difficult. Furthermore, it was a convenience sample of individuals from different regions of Portugal, which in itself would lead to discrepancies. Lastly, the findings should be interpreted in the light of recent favorable changes in CV mortality among the Portuguese population, which may indicate lower CV risk in the long term.
The results obtained, although encouraging, highlight the need for further studies of this age-group, in order to develop preventive measures that will lead to an effective reduction in CV risk.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Tralhão A, Sousa PJ, Ferreira A, et al. Perfil de risco cardiovascular de adultos jovens saudáveis – evolução temporal. Rev Port Cardiol. 2014;33:147–154.