Takotsubo cardiomyopathy is a reversible form of left ventricular dysfunction with an apparently benign natural history after left ventricular recovery. Rarely there are complications such as arrhythmias and apical thrombus. We describe a case of takotsubo cardiomyopathy complicated with apical thrombus and persistent complete atrioventricular block after improvement of left ventricular wall motion.
A miocardiopatia de takotsubo constitui uma forma transitória e aparentemente benigna de disfunção ventricular esquerda. Raramente cursa com complicações como arritmias e trombos apicais. Descrevemos um caso de miocardiopatia de takotsubo complicada com trombo apical e bloqueio aurículo-ventricular completo persistente após a normalização da contractilidade do ventrículo esquerdo.
Takotsubo cardiomyopathy (TC), or transient left ventricular apical ballooning syndrome, was first recognized in Japan in 1991.1 It is characterized by self-limited left ventricular mid and apical akinesia, usually precipitated by profound physical or emotional trauma.1–4 The natural history of TC appears to be benign, requiring supportive therapy until the ventricular dysfunction has resolved,2,4 but occasionally it has been identified as a precipitant of serious arrhythmias.2,6–8 Ventricular dyskinesia combined with increased sympathetic activation which alters the coagulation cascade may explain the apical thrombus formation sporadically reported in these patients.5 We present a case of TC associated with apical thrombus and complete heart block. To our knowledge this is the first report of an association of these two complications simultaneously in the same patient.
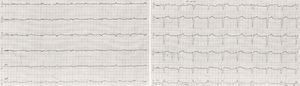
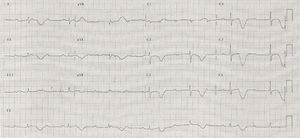
Case reportA 78-year-old woman with unremarkable cardiac and medical history was admitted to our hospital because of dyspnea, chest discomfort and dizziness lasting for a week, since she had been physically assaulted by her husband. On physical examination, she was hemodynamically stable and rales were detected in both lungs. The ECG showed complete heart block with wide QRS complexes (Figure 1).
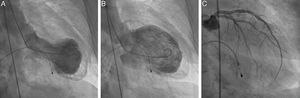
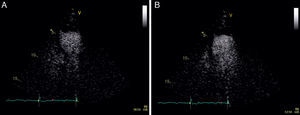
A transthoracic echocardiogram revealed severe left ventricular (LV) systolic dysfunction with akinesia of the mid-apical segments and hyperkinesis of the basal segments. Assuming a possible previous infarction with post-infarction angina and severe conduction abnormalities, cardiac catheterization was performed and temporary transvenous pacing was instituted. The coronary angiography excluded significant coronary vascular disease: 40% stenosis of the mild left anterior descending artery (LAD) and 50% of the distal circumflex coronary artery (Figure 2). The left ventriculography demonstrated typical “apical ballooning” and an apical thrombus (Figure 2, video 1). Contrast echocardiography confirmed the presence of apical thrombus and hypocoagulation therapy was initiated (Figure 3).
Results of cardiac catheterization. Left ventriculography at end-systole (A) and end-diastole (B) demonstrating typical apical ballooning and double outline apex suggestive of apical thrombus. Results of selective coronary angiography of the left main coronary artery (C) showing no significant stenosis.
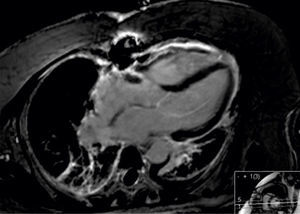
The patient's clinical evolution was favorable, however the LV dysfunction, wall motion abnormalities and AV conduction abnormalities did not improve significantly during the week after admission. Troponin level was maximum at admission (0.79ng/ml). Due to the lack of LV function improvement a temporary coronary occlusion could not be ruled out as the cause of apical ballooning. To better clarify the diagnosis cardiac magnetic resonance imaging was performed, almost two weeks after admission, and showed global (ejection fraction: 50%) and regional (hypokinesis of the 17th segment, lateral and inferior apical segments) improvement of LV function. There was no apical thrombus or delayed enhancement, consistent with the diagnosis of TC (Figure 4).
The echocardiography performed at this time confirmed the resolution of LV systolic function and wall-motion abnormalities. However, the complete AV block persisted and, consequently, a dual-chamber pacemaker was implanted (Figure 5). Pacemaker check at one year identified persistent complete heart block but the patient was asymptomatic.
DiscussionThis case demonstrates that complete AV block associated with takotsubo cardiomyopathy may persist after improvement of left ventricular wall motion, and pacemaker implantation may be needed.
The physiopathology of TC remains unclear, as does the involvement of the conduction system. It is still not known if in these cases the conduction system is primarily involved or if it suffers the consequence of an acutely distorted cardiac structure. It seems that the remodeling of the ventricle after the acute TC phase recovers within weeks, while the conduction system may take years to recover.6–8 Further follow-up of this patient will help determine whether the conduction disorder is permanent or will resolve over time.
AuthorshipAna Sofia Correia and Nuno Moreno contributed equally to the paper.
Conflicts of interestThe authors have no conflicts of interest to declare.