Fulminant myocarditis associated with influenza A virus is exceedingly rare, with only a few cases reported in the literature. We describe a previously healthy 10-year-old boy, with a three-day history of flu-like symptoms without antiviral treatment. He was hospitalized with dehydration and hypothermia in the context of persistent vomiting, when he suddenly developed heart failure secondary to fulminant myocarditis. Despite aggressive management, including circulatory support and cardiopulmonary resuscitation measures, the patient died of cardiogenic shock. The postmortem histopathology was compatible with a multisystem viral infection with myocarditis and pulmonary involvement, and H1N1v polymerase chain reaction was positive.
The prevalence of influenza-associated fulminant myocarditis remains unknown. Findings reported in the literature raise the possibility that the novel H1N1 influenza A virus is more commonly associated with a severe form of myocarditis than previously encountered influenza strains.
A miocardite fulminante associada ao vírus Influenza A é extremamente rara, com apenas alguns casos relatados na literatura. Descrevemos um rapaz de 10 anos, previamente saudável, com história de sintomas gripais com 3 dias de evolução, sem terapêutica antiviral. Foi internado por desidratação e hipotermia, no contexto de vómitos persistentes após o que, subitamente, desenvolveu insuficiência cardíaca secundária a miocardite fulminante. Apesar da intervenção imediata, incluindo suporte circulatório e reanimação cardiorrespiratória, o doente faleceu por choque cardiogénico. O exame histopatológico post-mortem foi compatível com o diagnóstico de infecção viral multissistémica, com miocardite e envolvimento pulmonar e a PCR para o H1N1v foi positiva.
A prevalência de miocardite fulminante associada ao vírus Influenza permanece desconhecida. Relatos na literatura levantam a hipótese de o vírus Influenza A H1N1 estar mais frequentemente associado a formas graves de miocardite do que as estirpes sazonais anteriores.
Acute myocarditis, albeit rare and potentially lethal, is a well-recognized manifestation of numerous viral infections with a broad spectrum of symptoms and clinical features.1 The etiological agents of viral myocarditis include enteroviruses, adenoviruses, parvoviruses, hepatitis C virus, human immunodeficiency virus, influenza, and others.2 Coxsackie B virus has been described as the most common pathogen of viral myocarditis and hepatitis C virus is associated with many different forms of heart disease worldwide; however, influenza myocarditis is relatively rare.3,4 Many people are affected by seasonal influenza every year, but the myocarditogenicity of this virus seems to be fairly low. The frequency of myocardial involvement in influenza infection is unclear,5 but some studies report that it ranges from 0 to 11%, depending on the diagnostic criteria used to define myocarditis.6
Myocarditis is an inflammatory disorder characterized by myocyte necrosis and inflammatory infiltrate of the myocardium.7 The pathogenesis of influenza myocarditis is also unclear. Host immune response may play a role, as well as direct cytolysis by viral infection.5 Fulminant myocarditis is an uncommon complication, typically diagnosed in association with circulatory collapse or at autopsy in patients with influenza-associated fatal outcomes. It may present with fatal arrhythmias, atrioventricular block and/or varying degrees of heart failure, cardiogenic shock being the most severe.1
A few case reports and series present incidental diagnoses of influenza-associated acute fulminant myocarditis, but the true prevalence remains unknown.1 We present a case of rapidly fatal fulminant pandemic influenza A (H1N1) virus (H1N1v)-associated myocarditis, with no previous cardiac symptomatology.
Case reportA previously healthy 10-year-old boy presented to the emergency department with a three-day history of a flu-like syndrome: fever, cough, headache, generalized myalgia, vomiting and diarrhea. He had no known risk factors for complications of influenza, he was not previously vaccinated for seasonal or pandemic influenza viruses and he was not receiving any antiviral treatment.
At admission, he was pale and had signs of dehydration. Body temperature was 34.7°C, pulse rate 120beats/min and blood pressure 84/65mmHg (median arterial pressure: 65mmHg). Pulse oximetry showed oxygen saturation of 96–98% and cardiac physical examination was normal. Chest radiography revealed diffuse bilateral alveolar infiltrates. Laboratory findings included 11300leukocytes/mm3 (84.5% neutrophils), C-reactive protein 2.41mg/dl, and elevated creatinine (1.4mg/dl), glucose (217mg/dl) and phosphorus (8.1mg/dl), with no other abnormalities. The patient's clinical condition improved significantly after intravenous fluid administration; however, when he was hemodynamically stable, sudden asystolic cardiac arrest occurred. Advanced life support was immediately started but was ineffective and the patient died.
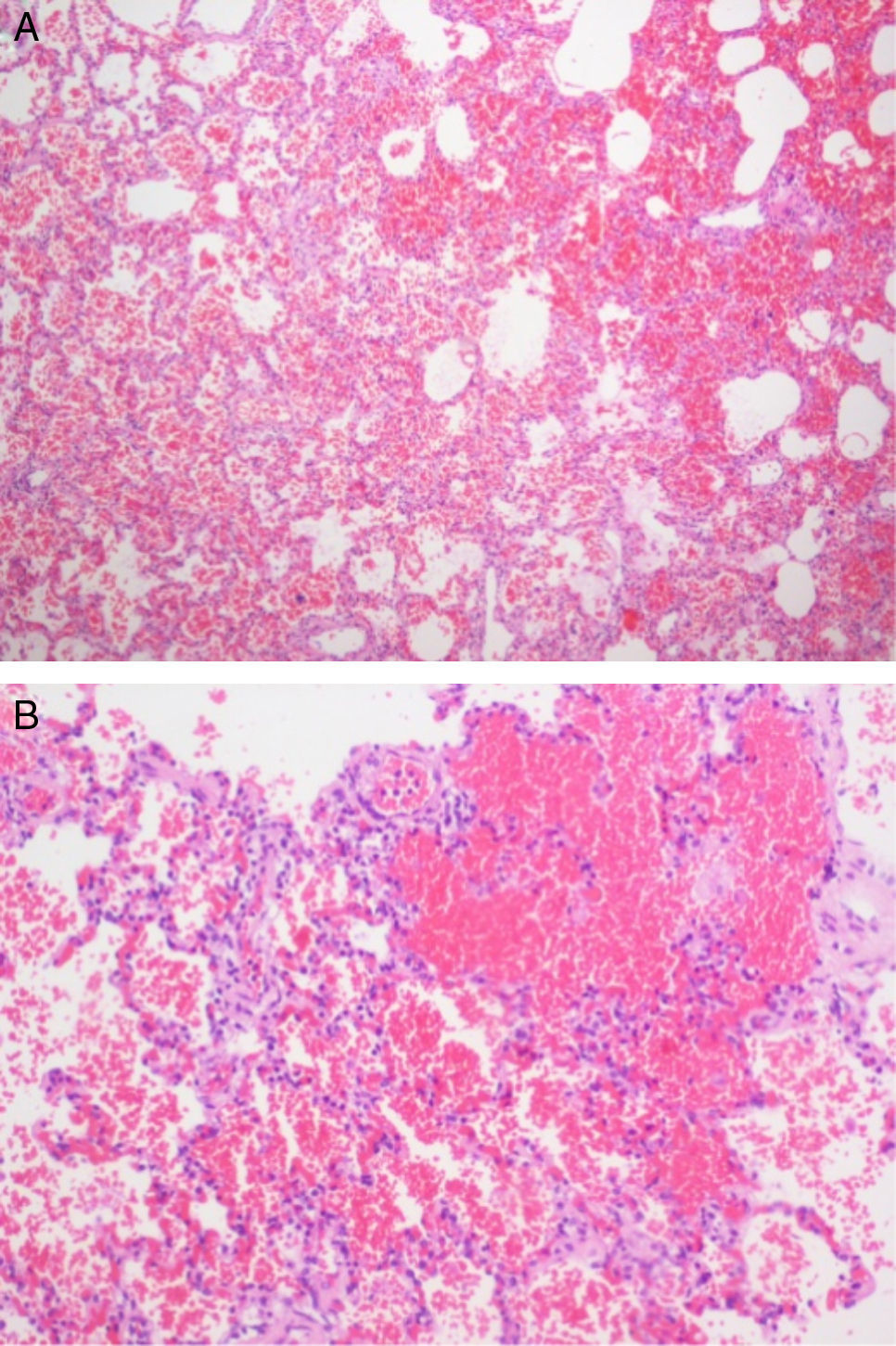
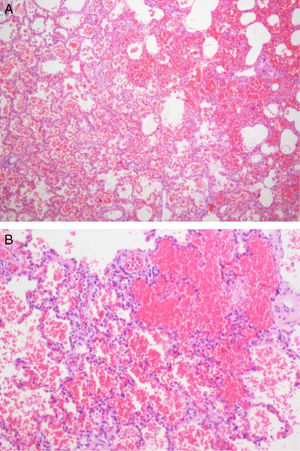
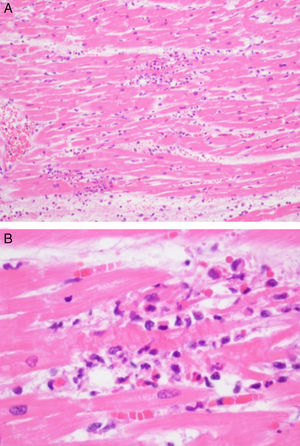
Further investigation showed mild elevation of CK, CK-MB and myoglobin. Reverse transcriptase polymerase chain reaction assay from nasopharyngeal swab samples was positive for H1N1v. The autopsy showed multifocal infiltrates composed mostly of lymphocytes but also some neutrophils, macrophages, plasma cells and eosinophils, associated with myocyte necrosis and ischemia, which was compatible with myocarditis (Figure 2) and excluded the diagnosis of hypertrophic cardiomyopathy. The lung tissue specimen obtained at autopsy showed diffuse pulmonary vascular congestion and extensive alveolar hemorrhage (Figure 1). Additionally, multisystem histological changes including the cardiac and pulmonary alterations described above, and tracheobronchial and intestinal involvement associated with viral infection were evident, leading to a definite postmortem diagnosis of fulminant viral myocarditis.
DiscussionThe prevalence of fulminant myocarditis associated with H1N1v is unknown because of the lack of comprehensive screening, with only a handful of case reports and autopsy findings in the literature.1 Bratincsak et al. reported four fulminant myocarditis cases associated with H1N1v in children and suggested that the 2009 pandemic influenza virus was more commonly associated with myocarditis than seasonal influenza.1 The Japanese pandemic influenza registry reported 15 patients with H1N1v-associated myocarditis, ranging from a child to a man over 70 years old.2 According to a report from Canada, only two of 505 children hospitalized with severe influenza infection had myocarditis.5 There are few individual case reports of fulminant myocarditis from the USA and Europe,8–12 and a single fatal case was reported in a multicenter pediatric study conducted in Spain.13 This is the first report in Portugal.
Common cardiac symptoms of myocarditis include dyspnea, chest discomfort, hypotension, peripheral edema and syncope.2 In the case of myocarditis caused by H1N1v, clinical manifestations vary greatly. Ukimura et al. reported that cardiac dysfunction had progressed rapidly in 12 out of 15 patients, and developed after recovery from flu-like symptoms in two patients. Ten patients with fulminant myocarditis had fatal arrhythmias and/or cardiogenic shock.2 Cardiopulmonary arrest as the first cardiac symptom was described in only two patients, as happened with our patient.2
Small autopsy-based studies have shown complication rates of myocarditis in fatal cases of 39.4% with Asian flu and 48% with Spanish flu.5 All these fatal cases with myocarditis had severe pneumonia and multiple organ involvement, implying that myocarditis was likely to be a terminally ill state of influenza infection,5 as could have been the case with our patient, according to the histopathological findings on autopsy (Figures 1 and 2). By contrast, severe viral pneumonia did not precede myocarditis in the 15 cases reported by Ukimura et al.2 Some patients complained only of high fever, without respiratory symptoms before the onset of myocarditis. The findings imply that the H1N1v may have a high affinity for heart tissue in some susceptible patients. In this patient there was initially thought to be an underlying cardiac disease (hypertrophic cardiomyopathy), which could have increased his susceptibility to cardiac complications, but this comorbidity was excluded by histopathology findings. Despite the presence of tachycardia, hypotension and hypothermia secondary to dehydration at admission, the patient was hemodynamically stable immediately before asystolic cardiac arrest and death.
Data on the clinical benefits of antiviral treatment for H1N1v are limited and different authorities have different recommendations. The Hong Kong Hospital Authority Central Committee on Infectious Disease and Emergency Responses (CCIDER) recommend that empirical antiviral treatment be started immediately in patients who are at higher risk for developing complications,14 including those younger than six years, morbidly obese, asthmatic, immunocompromised or pregnant subjects, patients showing no improvement in symptoms 48h after medical treatment and in patients in whom H1N1v infection has been confirmed.15 There are compelling indications for the use of beta blockers and/or angiotensin-converting enzyme inhibitors for the treatment of a subacute phase of the illness; additional supportive intervention is essential as first-line therapy for myocarditis patients with heart failure.
The recent application of intra-aortic balloon pump and/or veno-venous extracorporeal membrane oxygenation (ECMO) in serious cases has yielded good outcomes,2,16,17 but in this case, despite aggressive management, circulatory resuscitation was not successful. This patient did not receive antiviral treatment, which has been convincingly shown to decrease morbidity and mortality in H1N1v infection. However, as this was a case of fulminant evolution, with rapid progression of inflammatory infiltration, antiviral treatment probably would not have had sufficient time to be effective.
Early detection of myocarditis in patients during influenza pandemics is difficult, as there are no specific symptoms or signs.5 To avoid misdiagnosis it is essential to determine the characteristic symptoms, signs and laboratory findings of acute myocarditis,2 but it is also important to remember that it can occur suddenly, without any previous suspicious symptom or sign, as was seen in our patient.
This was the first death in the Portuguese pediatric population during the 2009 H1N1v pandemic, and provided arguments for more stringent indications for antiviral therapy in the context of influenza pandemics.
ConclusionThe fulminant form of myocarditis associated with H1N1v may present in the form of fatal arrhythmia, atrioventricular block and/or cardiogenic shock, usually diagnosed in the context of circulatory collapse or autopsy in patients with H1N1v infection, as occurred in this patient.
As the incidence of H1N1v infection continues to rise, physicians should be aware of this rare and potentially fatal complication, since early diagnosis and aggressive supportive measures are essential.
Conflict of interestThe authors have no conflict of interest to declare.