Congenital coronary artery anomalies are one of the causes of myocardial ischemia and sudden death in the young, mainly during sports. Origin of the right coronary artery from the left anterior descending artery is very rare, with a prevalence of 0.015%, corresponding to 1.2% of all coronary artery anomalies. The authors present the case of a 22-year-old man, with a history of cocaine use, admitted to hospital with a non-ST elevation acute myocardial infarction. Coronary angiography revealed the presence of this rare coronary anomaly and the absence of atherosclerotic luminal stenosis, and so it was assumed to be a type II infarction caused by cocaine-induced vasospasm of the anomalous vessel.
As anomalias coronárias congénitas são uma das causas de isquemia miocardica e morte súbita em jovens, principalmente durante a prática desportiva. A origem da artéria coronária direita na descendente anterior é muito rara, com uma prevalência de 0,015% e correspondendo a 1,2% das anomalias coronárias congénitas. Os autores apresentam o caso clínico de um homem de 22 anos, consumidor de cocaína, internado por enfarte agudo do miocardio sem supradesnivelamento de ST. O cateterismo mostrou a presença desta anomalia coronária rara e a ausência de lesões ateroscleróticas luminais, pelo que se assumiu tratar-se de um enfarte agudo do miocárdio tipo II secundário a vasospasmo do vaso anómalo induzido pela cocaína.
Congenital coronary artery anomalies (CAAs) are a heterogeneous group of anatomical entities. Their clinical significance varies widely, from an incidental finding on coronary angiography to acute presentation in the form of myocardial infarction (MI) or sudden death, typically in young adults following intense exercise or exposure to other types of physiological stress. Single coronary artery is a rare anomaly and is associated with risk for adverse cardiac events. The authors present the case of a rare anatomical subtype of single coronary artery that manifested as an acute coronary syndrome in a young man.
Case reportA 22-year-old man, white, a smoker and sporadic cocaine user, with a family history of ischemic heart disease, was admitted to the emergency room (ER) with crushing chest pain of three hours’ evolution that had begun at rest around 24 hours after cocaine use. He was initially asymptomatic in the ER following administration of sublingual nitrates. He was hemodynamically stable (blood pressure 123/67mmHg; heart rate 92 bpm), with no signs of hypervolemia; oxygen saturation was 97% on pulse oximetry, and he was apyretic. The admission electrocardiogram (ECG) showed no significant alterations. Laboratory tests revealed elevated markers of myocardial necrosis (troponin I: 7ng/ml) but no other abnormalities. Echocardiography performed in the ER showed posterior and inferior wall hypokinesia, with good biventricular global systolic function. The pain recurred in the ER, repeat ECG showing transient 1-mm ST-segment elevation in the inferior leads; following further administration of sublingual nitrates, the pain disappeared and the ECG returned to the initial pattern.
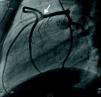
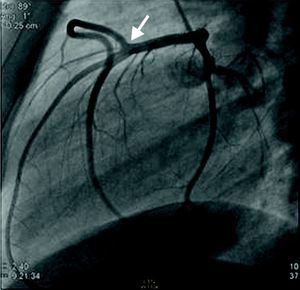
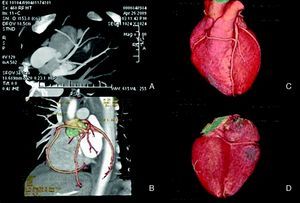
The patient was admitted to the coronary care unit with a diagnosis of non-ST elevation acute coronary syndrome and underwent urgent catheterization. Coronary angiography excluded atherosclerotic luminal stenosis, but revealed a CAA – a single coronary ostium in the left sinus of Valsalva, giving rise to the left main coronary artery. This vessel had a normal course, dividing into the left anterior descending artery (LAD) and the circumflex artery with normal anatomical distributions, while the right coronary artery (RCA) had an anomalous origin in the mid segment of the LAD and then coursed to the right to vascularize its usual territory (Figure 1). CT angiography was performed to clarify the anatomical relations of the RCA, which excluded a malignant course between the aorta and the pulmonary artery and showed reduced epicardial blood flow in the posterior and inferior walls, due to absence of the posterior and posterolateral descending arteries (Figure 2). The calcium score was zero.
64-slice cardiac CT: (A) (maximum-intensity projection reconstruction) and (B) (volume-rendered reconstruction) show anomalous origin of the right coronary artery in the mid segment of the left anterior descending artery; (C) (volume-rendered reconstruction) shows the right coronary artery coursing anterior to the great vessels; (D) (volume-rendered reconstruction) shows reduced epicardial blood flow in the posterior and inferior walls due to absence of posterolateral and posterior descending arteries.
The patient remained asymptomatic and hemodynamically stable, and was discharged on the sixth day of hospitalization. Peak troponin T was 1.40ng/ml. Screening for prothrombotic disease was negative. The ECG showed no Q waves and the discharge echocardiogram showed normalization of wall motion abnormalities.
The patient underwent single-photon emission computed tomography with exercise testing as an outpatient in order to exclude residual myocardial ischemia, which was negative. Medical therapy was therefore continued with aspirin 100mg and diltiazem 120mg per day. He was advised to avoid strenuous physical activity, smoking and cocaine.
After a 23-month follow-up the patient remains asymptomatic and abstaining from cocaine.
DiscussionThe criteria for considering an anatomical variant as an anomaly are still the subject of debate but a prevalence of less than 1% is one requirement found in the literature.1 The prevalence of CAAs in published series ranges between 0.3% and 5.6%.1–4 In the largest series to date (126595 patients), Yamanaka et al. reported a prevalence of 1.3%,2 while in a study of 3660 patients in a single Portuguese center by Correia et al., it was 0.68%.3
CAAs have been identified as a relatively common cause of sports-related sudden death in young adults, being documented on autopsy in 12% of such cases.5
Single coronary artery is a rare anomaly (prevalence of 0.049%, and 3.31% of CAAs) that is associated with adverse cardiac events, including myocardial ischemia and sudden death. The subtype of an anomalous RCA arising from the LAD (type RII in Lipton's classification) is extremely rare (prevalence of 0.015%, and 1.2% of CAAs).2 The RCA courses between the great vessels in 38% of cases,6 this variant being associated with a high risk of myocardial ischemia and death due to its vulnerability to extrinsic compression. It is also frequently associated with atherosclerotic coronary disease, being reported in 54% of cases published.7
Cocaine's cardiotoxicity can lead to serious complications, which may be chronic or acute. There are various mechanisms by which cocaine can cause myocardial ischemia, including coronary vasospasm, and atherogenic and thrombogenic effects, as well as increased oxygen demand.8,9 The risk of MI is greatest within an hour of taking cocaine and occurs within three hours in two-thirds of cases, although there are reports of infarction up to four days after use.9 Evidence suggests that events occurring late after exposure may be due to impaired endothelium-dependent vasorelaxation, since endothelial dysfunction has been demonstrated in cocaine users, with reduced nitric oxide production10 and increased release of endothelins.11
With regard to the pathophysiology of myocardial necrosis in the case presented, the absence of angiographic evidence of atherosclerotic luminal stenosis means that it was unlikely to have been caused by a plaque event (type I infarction). There were thus only two factors identified that could have contributed to infarction in this patient: (1) CAA, a single vessel, with the RCA arising in the LAD; and (2) recent cocaine use. As stated above, a single coronary artery is associated with risk for adverse cardiac events.2 The course of the RCA in our patient was anterior to the aortic root, and so extrinsic compression by the great vessels was not the pathophysiological mechanism. Other mechanisms described as potential causes of myocardial ischemia in patients with CAA and no atherosclerotic disease include reduced functional coronary reserve, abnormal flow patterns, and autonomic and/or endothelial dysfunction causing spasm and/or thrombosis.1 The location of the ECG and echocardiographic alterations at admission (transient ST-segment elevation in the inferior wall and posterior and inferior hypokinesia) suggests that the myocardial ischemia and necrosis occurred in the territory supplied by the RCA, which indicates that this artery was directly involved in the process, reduced epicardial blood flow in its territory playing an important role in the pathophysiology of ischemia. The late presentation, as well as pain recurrence without re-exposure, may be interpreted as vasospasm induced not only by the direct vasoconstrictive action of cocaine but also by the more persistent endothelial dysfunction caused by the drug.10,11
We therefore consider this to be a case of type II infarction, in which a rare coronary artery anomaly provided a substrate that was highly vulnerable to the cardiotoxic effects of cocaine. The absence of atherosclerotic coronary disease, thrombus or an anatomical course associated with risk of extrinsic compression, suggests that vasospasm in the anomalous vessel was the principal pathophysiological mechanism.
ConclusionThis case illustrates a rare form of CAA that is associated with adverse clinical events, including MI and sudden death. Since CAAs are one cause of sports-related sudden death in young adults, they should be considered in differential diagnosis of young patients who present with syncope, chest pain or cardiopulmonary arrest.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Antunes N, et al. Origem anómala da coronária direita e enfarte agudo do miocárdio: causa ou coincidência? Rev Port Cardiol. 2012;31(7-8):509-512.