To evaluate the efficacy and safety of a heart rate (HR) reduction protocol using intravenous esmolol as bailout for failed oral metoprolol regimens in patients undergoing coronary computed tomography angiography (CCTA) with 64-slice multidetector computed tomography (64-MDCT).
MethodsPatients who underwent cardiac 64-MDCT in a single institution between 2011 and 2014 were analyzed. Those with HR above 60 beats per minute (bpm) on presentation received oral metoprolol (50-200 mg) at least one hour before CCTA. Intravenous esmolol 1-2 mg/kg was administered as a bolus whenever HR remained over 65 bpm just before imaging. The primary efficacy endpoint was HR <65 bpm during CCTA. The primary safety endpoint was symptomatic hypotension or bradycardia up to hospital discharge.
ResultsDuring the study period CCTA was performed in 947 cases. In 86% of these, oral metoprolol was the only medication required to successfully reduce HR <60 bpm. Esmolol was used in the remaining 130 patients (14%). For esmolol-treated patients mean baseline and acquisition HR were 74±14 bpm and 63±9 bpm, respectively (p<0.001). The target HR of <65 bpm was achieved in 82 of the 130 esmolol-treated patients (63%). Considering the whole population, esmolol use led to a significant increase in the primary efficacy endpoint from 86% to 95% (p<0.001). Esmolol also resulted in a statistically, but not clinically, significant reduction in systolic blood pressure (144±22 to 115±17 mmHg; p<0.001). The combined primary safety endpoint was only observed in two (1.5%) patients.
ConclusionDespite optimal use of oral beta-blockers, 14% of patients needed intravenous esmolol for HR control. The pre-medication combination of oral metoprolol and on-demand administration of intravenous esmolol was safe and effective and enabled 95% of patients to be imaged with HR below 65 bpm.
Avaliar a eficácia e segurança de um protocolo de redução de frequência cardíaca (FC) utilizando esmolol endovenoso após falência de metoprolol oral, em doentes submetidos a angiografia coronária por tomografia computorizada (CCTA) de 64 cortes.
MétodosDe 2011 a 2014 foram avaliados os indivíduos submetidos a CCTA num único centro. Os indivíduos com FC >60 bpm à admissão receberam 50-200 mg de metoprolol oral pelo menos uma hora antes da CCTA. Esmolol endovenoso em bólus (1-2 mg/kg) foi administrado se FC >65 bpm imediatamente antes da aquisição de imagem. O endpoint primário de eficácia foi FC <65 bpm durante a aquisição de imagem com contraste. O endpoint primário de segurança foi hipotensão ou bradicardia sintomática durante a permanência no hospital.
ResultadosForam efetuadas 947 CCTA durante o período de estudo. Em 86% dos casos, metoprolol oral foi o único fármaco utilizado. Foi necessária a administração de esmolol em 130 (14%) doentes. Nos doentes que receberam esmolol, a FC basal reduziu em média de 74±14 bpm para 63±9 bpm (p<0,001). O objetivo primário de FC <65 bpm foi alcançado em 82 desses 130 doentes (63%). Considerando toda a população, o recurso a esmolol permitiu um aumento significativo da proporção de CCTA realizados com FC <65 bpm (86% para 95% [p<0,001]). A administração de esmolol esteve associada a redução estatisticamente, mas não clinicamente, significativa da pressão arterial sistólica (144±22 para 115±17 mmHg; p<0,001). O endpoint combinado de segurança foi observado em dois (1,5%) dos doentes.
ConclusãoApesar da utilização sistemática de betabloqueante oral, 14% dos casos necessitaram de esmolol endovenoso para controlo adequado de FC. Pré-medicação combinada de metoprolol oral e esmolol endovenoso quando necessária foi segura e eficaz, e permitiu que 95% dos doentes apresentassem FC <65 bpm no momento da aquisição de imagem.
Adequate heart rate (HR) control is paramount for optimal cardiac imaging using single-source 64-slice multidetector computed tomography (64-MSDT).1–5 For these scanners, HR during image acquisition should be below 65 beats per minute (bpm) and preferably lower than 60 bpm for optimal image quality.6 However, commonly used pre-medication regimens with oral or intravenous metoprolol are frequently unsatisfactory.7–9 Side effects, including hypotension and bradycardia, are also points of concern.
Intravenous esmolol, due to its rapid onset and short half-life, has been reported as a valuable option for adequate HR control, either alone or in combination with oral beta-blockers.10–12
The aim of the present study is to evaluate the efficacy and safety of an HR reduction protocol using intravenous esmolol as bailout for failed oral metoprolol regimens in patients undergoing coronary computed tomography (CT) angiography (CCTA).
MethodsStudy populationPatients undergoing CCTA in a tertiary academic medical center between August 2011 and June 2014 were analyzed. Those presenting in sinus rhythm and without contraindications for beta-blockers were included. All patients had indication for coronary anatomy assessment. Nineteen patients also had associated secondary indications: percutaneous aortic valve implantation (two), paroxysmal atrial fibrillation ablation (sinus rhythm during CCTA) (three), assessment of left ventricular morphology (two), evaluation of valve heart disease (three) or ascending aorta (two), and morphological studies for congenital heart disease (seven).
Patient preparationOral metoprolol was not used for patients presenting with HR <60 bpm, who proceeded directly to the CT table. Individuals with baseline HR of 60-65 bpm or >65 bpm received 50 mg or 100 mg oral metoprolol, respectively. An additional dose of 100 mg metoprolol was administered one hour later if HR was still above 65 bpm. After repeated oral metoprolol administration another 60 min interval was allowed. Patients were then moved to the CT table. After sublingual nitrate administration and just after scouting or calcium score image acquisition (Figure 1), an intravenous (IV) bolus of esmolol 1 or 2 mg/kg was administered if HR was >65 bpm or >70 bpm, respectively. A second bolus of esmolol was administered 1 min later if HR remained above 65 bpm using the same dosage.
Blood pressure and HR were assessed at baseline, in the CT room before and after scanning, and before discharge until systolic blood pressure (SBP) was >100 mmHg and HR >50 bpm or had returned to baseline.
Scan protocol and image reconstructionA single scanner was used for all cases (LightSpeed VCT XT, GE Healthcare, Milwaukee, USA). First, unenhanced prospective heart rate-triggered axial scanning of the heart was performed for calcium scoring (slice thickness 2.5 mm; voltage 120 kV, tube current 70 mA; 0.35 s partial rotation) just after sublingual nitrate administration. In view of the requirement for esmolol administration (HR on the CT table >65 bpm) a conservative acquisition approach was used and retrospective gating with dose modulation was selected for all these patients. The contrast-enhanced scan was obtained using Visipaque™ (iodixanol) 320 mg injected through a peripheral vein at 5 ml/s followed by a saline bolus chase. The scan parameters used were 0.625 mm collimation, rotation time 350 ms, pitch adjusted to each patient's HR, tube voltage 80-120 mV, and effective mA 100-600.
Estimated effective radiation dose was calculated by applying a factor of 0.014 to the volumetric CT dose. Calcium scoring was included in the total effective radiation dose. Electrocardiographically gated datasets were reconstructed from 40% to 80% of the R-R cycle length in 10% increments.
EndpointsThe primary efficacy endpoint was HR <65 bpm during contrast image acquisition and the secondary efficacy endpoint was HR <60 bpm during contrast image acquisition.
The primary safety endpoint was symptomatic hypotension (SBP <90 mmHg) or bradycardia (heart rate <45 bpm) up to hospital discharge, while the secondary safety endpoints were SBP <90 mmHg or HR <45 bpm (with or without symptoms) up to hospital discharge.
Statistical analysisThe statistical analysis was performed using IBM SPSS Statistics (version 22; IBM SPSS, Chicago, IL). Continuous variables were expressed as mean ± standard deviation or median ± interquartile range. Normality was tested by the Kolmogorov-Smirnov test. Study group characteristics were compared using the Student's t test or the Wilcoxon-Mann-Whitney test for continuous variables, and Pearson's chi-square test or Fisher's exact test for categorical measures, as appropriate.
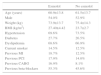
ResultsOf the 947 CCTAs performed (76% of all CCTAs performed in the study period), HR <65 bpm during CCTA acquisition was achieved in 830 cases (86%) using the oral metoprolol regimen alone. Intravenous esmolol was necessary in the other 130 patients (54% male, mean age 60.9±13.8 years and body mass index 27.40±4.42 kg/m2) (Table 1). Nearly half (53%) of the esmolol-treated patients had been pre-medicated before admission with oral beta-blockers in accordance with the indications of the referring physician.
Clinical characteristics of patients receiving and not receiving esmolol.
| Esmolol | No esmolol | |
|---|---|---|
| Age (years) | 60.9±13.8 | 61.5±13.7 |
| Male | 54.0% | 52.9% |
| Weight (kg) | 73.9±13.7 | 75.4±14.3 |
| BMI (kg/m2) | 27.40±4.42 | 23.7±2.7 |
| Hypertension | 69.6% | 73.5% |
| Diabetes | 27.7% | 26.5% |
| Dyslipidemia | 68.6% | 66.9% |
| Current smoker | 14.5% | 12.5% |
| Previous MI | 18.7% | 12.5% |
| Previous PCI | 17.9% | 14.0% |
| Previous CABG | 16.9% | 8.1% |
| Previous beta-blockers | 55.3% | 45.6% |
BMI: body mass index; CABG: coronary artery bypass grafting; MI: myocardial infarction; PCI: percutaneous coronary intervention.
In about one third (35%) of esmolol-treated patients, HR on presentation was <60 bpm and thus they received no oral metoprolol, but on the CT table HR increased to >65 bpm requiring IV esmolol as per protocol. The remaining 65% (84 patients) had received in-hospital oral metoprolol (mean dose 0.69 mg/kg) according to the predefined study protocol. The mean time between first oral dose of metoprolol and intravenous esmolol administration was 82±39 min. The mean esmolol dose administered was 1.54 mg/kg.
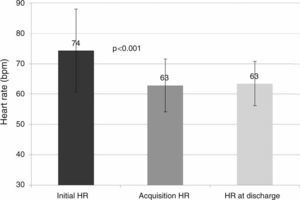
Initial mean HR in esmolol-treated patients was 74±14 bpm, which decreased to 63±9 bpm during CCTA acquisition (p<0.001), corresponding to a significant mean reduction in HR of 15±13% (Figure 2). During CCTA HR variability, defined as (maximum HR - minimum HR)/mean HR, was 6.3±7.1 in esmolol patients.
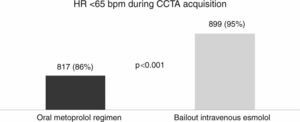
HR <65 bpm was achieved in 82 of the 130 esmolol-treated patients (63%). Thus, considering the entire CCTA population, the combined metoprolol/esmolol regimen led to a significant increase in the primary efficacy endpoint, from 86% to 95% (p<0.001) (Figure 3).
The secondary efficacy endpoint (HR <60 bpm) was reached in 47 of the 130 esmolol patients (36%).
Four of the esmolol-treated patients (3%) had minimum HR below 45 bpm. Mean time to HR recovery to >60 bpm in these patients was 37.8±32.3 min. During CCTA, HR above 80 bpm was observed in five (4%) patients. Mean HR at discharge was 64±7 bpm (Figure 2) in the esmolol group.
Esmolol use resulted in a significant reduction in mean SBP (143±21 to 115±17 mmHg; p<0.001). In 11 patients (8%) SBP decreased to levels below 90 mmHg. Mean SBP at discharge was 119±18 mmHg (Figure 4A). Initial diastolic blood pressure was 80±12 mmHg, decreasing to 62±11 mmHg after intravenous esmolol (p<0.001). Diastolic blood pressure at discharge was 69±10 mmHg (Figure 4B).
The combined primary safety endpoint (symptomatic hypotension or symptomatic bradycardia) was only observed in two patients (1.5%). Both cases resolved with supine positioning, intravenous fluids and atropine (1 mg) administration, without further complications.
In esmolol-treated patients 113 scans (87%) were of good image quality, 10 (8%) were of moderate quality, and seven (5%) were of poor quality and considered non-diagnostic. In the latter group HR during CCTA was 75±9 bpm and HR variability was 5.3 (42.6).
Retrospective gating with dose modulation was selected for all esmolol-treated patient due to high baseline HR. Mean estimated radiation dose was 9.8±10.6 mSv.
DiscussionHR while scanning should be less than 65 bpm and ideally less than 60 bpm for optimal image quality when a 64-slice MDCT scanner is to be used.6 Despite this recommendation, in 2007 an American survey showed that there were differences in beta-blocker protocols and that a cutoff higher than 65 bpm was used by 80% of centers.13
Metoprolol is the most common beta-blocker agent used to achieve HR control during CCTA. However, due to its low oral bioavailability, variable metabolism and inter-subject variability, the results are often suboptimal. This has led to the use of several alternate regimens including intravenous metoprolol, other beta-blockers such as atenolol, ivabradine, or calcium channel blockers.14,15 Nevertheless intravenous metoprolol, the most commonly used parenteral beta-blocker, has demonstrated limited efficacy in lowering HR.
Ivabradine has been suggested as an alternative to beta-blockers. Regimens of oral ivabradine proved more effective in reducing HR than oral metoprolol16 and an intravenous protocol demonstrated efficacy and safety in patients ineligible for intravenous beta-blockers.17
Esmolol may be at least as efficacious as intravenous metoprolol to achieve optimal HR.12 However, to our knowledge there are no studies reporting on esmolol use as bailout when previous oral HR regimens have failed.
In our study the oral metoprolol regimen used enabled 86% of patients to achieve target HR <65 bpm. This percentage is higher than described in previous studies. De Graaf et al. demonstrated optimal beta-blockade in 73% of CCTA patients using oral metoprolol.18 Intravenous metoprolol, also commonly used, again demonstrated limited efficacy in lowering HR. In a study by Jimenez-Juan et al. only 42% of patients who did not achieve HR <60 bpm with oral metoprolol reached target HR with additional intravenous metoprolol.19 These findings highlight the need for a more effective protocol for HR control. In addition, the rapid action and short half-life of esmolol make it an attractive drug in this setting. Similarly to data reported by Degertekin et al.,10 in our study bolus esmolol produced HR below 65 bpm in 63% (82/130) of patients. Thus, the introduction of bailout intravenous esmolol enabled 95% of the entire cohort to be imaged with HR below 65 bpm. The mean HR reduction was 11 bpm, 4% of patients were imaged with HR greater than 80 bpm and only 5% of CCTA exams were considered to be non-diagnostic.
Our study suggests that despite an aggressive beta-blocker strategy, the risk of side effects was relatively small. Only 1.5% of patients had symptomatic hypotension or bradycardia. Wang et al. reported 0.4% incidence of adverse events in a Chinese population treated with intravenous esmolol only.11 In our cohort, however, esmolol was used on top of oral metoprolol in 64% of cases, which could explain the higher incidence of side effects. Contraindications for beta-blockers are often considered a limitation for CCTA in patients with relatively high HR. Esmolol's short half-life could make it useful for patients who cannot tolerate prolonged beta-blockade.
We reported a higher effective radiation dose than some real-world registries.20 Unlike these studies, in which both prospective and retrospective acquisition protocols are reported, herein we report on a specific population subset in which only a retrospective acquisition protocol was chosen for all patients (because of high baseline HR). Also, in our registry about 15% of esmolol-treated patients had secondary indications for scanning, such as study for transcatheter aortic valve implantation, in which the scan range is significantly greater.
The introduction of high temporal resolution (83 ms) dual-source CT in clinical practice in 2005 has enabled high image quality diagnostic CCTA studies at increased HR with less dependency on HR lowering agents.21 However, the latest generation of dual-source scanners has introduced a new scan mode, prospectively ECG-triggered helical data acquisition with very high pitch values. The high pitch enables acquisition with very low radiation exposure (<1 mSv) but low and regular HR is critical for this technique. Consequently, effective HR reduction strategies are yet again pivotal if such very low dose acquisition protocols are to be followed.22
Study limitationsThis is a retrospective study with inherent limitations including potential selection bias. However, the HR control protocol was prospectively designed and uniformly applied to all eligible patients. Also, this was a single-center experience with a relatively small sample of esmolol-treated patients. Larger multicenter trials using placebo or intravenous metoprolol as active controls will be needed to clearly establish the role of intravenous esmolol in this setting.
ConclusionDespite optimal use of oral metoprolol for HR control before CCTA, 14% of cases still required intravenous esmolol for HR control. Bailout administration of intravenous esmolol on the CT table was safe and effective and enabled 95% of patients to be imaged with HR below 65 bpm.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.