Anomalous pulmonary venous return (APVR) is a rare cardiac anomaly defined as one or more pulmonary veins draining into a structure other than the left atrium, with venous return directly or indirectly to the right atrium. The most common form is partial APVR, in which one to three pulmonary veins drain into systemic veins or into the right atrium. We report the case of a woman diagnosed with partial APVR by magnetic resonance imaging during pregnancy.
A drenagem venosa pulmonar anômala (DVPA) é uma rara anomalia cardíaca definida como drenagem de uma ou mais veias pulmonares fora do átrio esquerdo, com retorno venoso direta ou indiretamente para o átrio direito. A situação mais comum é a DVPA parcial, na qual de uma a três veias pulmonares drenam para veias sistêmicas ou para o átrio direito. É descrito um caso de paciente diagnosticada com DVPA parcial através da ressonância magnética cardíaca (RMC) realizada durante a gestação.
Anomalous pulmonary venous return (APVR) is a rare cardiac anomaly arising from malformation of the pulmonary veins and accounts for less than 1% of congenital cardiac defects.1 APVR is classified as total when all four pulmonary veins drain into a structure other than the left atrium (LA), and partial when one to three veins drain into a systemic vein or into the right atrium (RA). Partial APVR is the most common form in adults and is generally associated with atrial septal defect (ASD).2,3
Partial APVR is usually diagnosed by echocardiography or conventional angiography, but since complete and selective characterization of the pulmonary veins may not be possible with these methods, other noninvasive exams are increasingly used, including magnetic resonance imaging (MRI) and computed tomography angiography.4 We present the case of a pregnant woman diagnosed with partial APVR by cardiac MRI.
Case reportA 22-year-old woman had a history of worsening exertional dyspnea, chest pain, palpitations, dizziness and syncopal episodes for six years. Following an outpatient consultation with a general practitioner, transthoracic Doppler echocardiography (Hewlett-Packard/Philips SONOS 5500 scanner with 2.5 and 5–7.5 MHz transducers) was performed, which revealed mild to moderate right ventricular (RV) dilatation, mild tricuspid regurgitation, and mild to moderate pulmonary hypertension.
In view of the patient's worsening symptoms, she was referred for cardiological consultation. On physical examination, she was in good general health, eupneic with normal pulses, and blood pressure of 120/80 mmHg. Cardiac auscultation revealed a high-pitched systolic murmur over the left sternal border. There was no lower limb edema or hepatomegaly. Transesophageal Doppler echocardiography was then requested, which showed RV dilatation, as well as dilatation of the RA and the venous coronary sinus, and anomalous interventricular septal motion. Global systolic function was preserved. Right atrial pressure was estimated at 5 mmHg as assessed by the inferior vena cava collapsibility index in subcostal view in M mode. Pulmonary artery systolic pressure was estimated at 33 mmHg by analysis of tricuspid regurgitation. The echocardiographer suggested persistent left superior vena cava as a possible explanation for the dilatation of the venous coronary sinus.
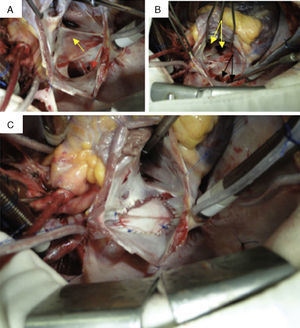
Cardiac MRI (Philips Achieva® 1.5 T system) was performed for diagnostic clarification, using balanced steady-state free precession cine sequences and phase contrast to assess valve function. Since at the time of the exam the patient was in the third month of pregnancy, it was decided not to use a contrast agent and so magnetic resonance angiography of the pulmonary veins was not possible. Cine MRI showed the right pulmonary veins, with adjacent ostia, apparently draining into the RA, while the left pulmonary veins drained normally into the LA. No atrial or ventricular septal defects were observed, but there was right chamber and venous coronary sinus dilatation and RV hypertrophy. Partial APVR was suggested as a possible explanation for the MRI findings; the echocardiographer's suspicion of persistent left superior vena cava was confirmed. Medical treatment was begun with diuretics and it was decided to continue with the pregnancy. Eight months after childbirth, cardiac MRI was repeated, this time with angiography of the pulmonary veins (Figure 1), which confirmed the diagnosis of partial APVR. The exam also showed a reduction in right chamber diameters and volumes compared to the previous MRI exam, which may be explained by the patient's pregnancy-induced hypervolemic state.
Magnetic resonance angiography of the pulmonary veins: three-dimensional images in superior (A) and posterior (B) views, confirming partial anomalous pulmonary venous return, with two pulmonary veins draining into each atrium. VPID: right inferior pulmonary vein; VPIE: left inferior pulmonary vein; VPSD: right superior pulmonary vein; VPSE: left superior pulmonary vein.
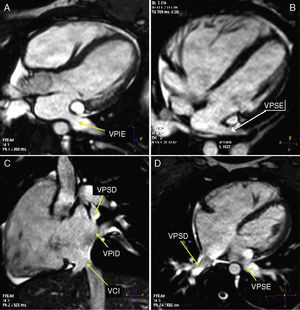
In view of these findings, the patient was referred for total surgical repair of APVR, which was performed with extracorporeal circulation, hypothermia (24°C) and administration of cardioplegic solution. Following right atriotomy, the right pulmonary veins were visualized draining into the RA (Figure 2). The intact atrial septum was resected and the anomalous veins were tunneled to the LA using a bovine pericardial patch. The patient is currently recovering well from the procedure, with regression of symptoms.
Surgical repair of partial anomalous pulmonary venous return: confirmation of anomalous drainage of the right pulmonary veins into the right atrium, with intact atrial septum. (A) Right pulmonary veins draining into the right atrium, with no atrial septal defect. Red arrow: venous coronary sinus; yellow arrow: fossa oval, intact atrial septum; (B) atrial septum opened surgically, showing left atrium and left pulmonary veins. Black arrows: right pulmonary veins; yellow arrows: left pulmonary veins; (C) correction complete, with a bovine pericardial patch directing right pulmonary venous flow into the left atrium.
Partial APVR is a rare congenital anomaly in which one to three pulmonary veins drain into the RA or one of its tributary veins instead of the LA. In over 95% of cases, anomalous connections occur in one or two pulmonary veins, but rarely involve both lungs at the same time.2,3 It is commonly associated with ASD, but even when the septum is intact, mild clinical symptoms persist in 20–33% of cases, albeit later in life.3,4 The main clinical manifestation is exertional dyspnea. In the absence of ASD, the right chambers are subjected to volume overload and dilate, causing arrhythmias and pulmonary hypertension.4 Pregnancy is known to exacerbate the clinical manifestations of APVR, since it is associated with hypervolemia, hypercoagulability and reduced peripheral arterial resistance, which increase cardiac output and aggravate symptoms.5
Doppler echocardiography can identify the course of the pulmonary veins and their connections with the systemic circulation, and possible obstructions, as well as assessing pulmonary artery systolic pressure and RV dilatation, and thus plays an important role in suspected partial APVR. However, echocardiography is operator-dependent and has certain limitations in assessing complex lesions, particularly those that involve the central pulmonary vasculature and the right chambers, even when a transesophageal approach is used. Confirmation of the diagnosis is usually obtained through hemodynamic study by angiography, which is also essential to assess the degree of pulmonary hypertension.6–8 However, this method is invasive and traumatic, requiring the use of ionizing radiation and contrast agents with possible nephrotoxic effects.6,8
Noninvasive imaging methods are thus useful to confirm or exclude a diagnosis of partial APVR. Cardiac MRI, by combining high spatial resolution angiography and tissue characterization, is of recognized value,6–8 since, without ionizing radiation, it can delineate the anatomy of the great vessels, accurately assess pulmonary venous return and quantify the extent of left-to-right shunting. Furthermore, through analysis of the anatomy and morphology of the right chambers and of ventricular function, cardiac MRI is excellent at measuring RV volume and flow, as well as ventricular mass, thickness and contractility. Thus, MRI affords comprehensive assessment of patients with suspected partial APVR, overcoming most of the limitations of echocardiography, and can be considered a viable noninvasive alternative to cardiac catheterization to guide treatment, which can include different surgical approaches.6–9 Since the patient in the case presented was pregnant, partial APVR could only be assumed on cine MRI (Figure 3); gadolinium contrast angiography was later performed for three-dimensional assessment of the anomalous vasculature (Figure 1).
Cardiac magnetic resonance cine sequences, showing both left pulmonary veins draining into the left atrium (A and B) and both right pulmonary veins draining into the right atrium (C and D). VCI: inferior vena cava; VPID: right inferior pulmonary vein; VPIE: left inferior pulmonary vein; VPSD: right superior pulmonary vein; VPSE: left superior pulmonary vein.
Most studies suggest that MRI is safe in pregnancy since magnetism poses no risk to mother or fetus, with no reports of teratogenesis. Nevertheless, a few studies have suggested that prolonged exposure may be harmful to embryogenesis, chromosomal structure and fetal development, effects that have been minimized by recent advances in MRI systems that include ultrafast image acquisition.9–11 Studies on the use of contrast agents in pregnancy are sparse and little is known concerning their effects on human embryos and fetuses, although it is known that gadolinium crosses the placenta when administered at usual doses.12,13 The chelating agent used in gadolinium contrast can accumulate in the amniotic fluid, but the significance of fetal exposure and the risk of nephrogenic systemic fibrosis are unknown. For this reason, this contrast agent should not be used routinely in pregnant women.13 Although various studies have demonstrated that MRI poses no risk in pregnancy, its safety has not been definitively proven, according to the US Federal Drug Administration. Thus, current thinking is that the decision to use MRI depends on the underlying disease and gestational age, but is generally recommended only from week 24 of gestation, after organogenesis; its use in the first trimester is not advised.9,11
The indications for surgical repair of partial APVR depend on detailed assessment of the anatomy of the pulmonary and systemic veins, presence of ASD and quantification of left-to-right shunting.1,3 Since there was no ASD in the case presented, the indicated surgery was to redirect the right pulmonary veins into the LA.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Souto FM, Andrade SM, Barreto ATF, Souto MJS, Russo MA, de Mendonça JT, et al. Drenagem venosa pulmonar anômala em gestante identificada pela ressonância magnética cardíaca. Rev Port Cardiol. 2014;33:383.