Coronary pseudoaneurysms are an unusual finding during coronary angiography and there are very little data on their prognosis in the literature. We report the case of a 62-year-old man admitted with an anterior myocardial infarction who developed a pseudoaneurysm in the mid left anterior descending artery some days after a type I coronary perforation during coronary angioplasty. Spontaneous closure of the pseudoaneurysm was observed during hospital follow-up. Spontaneous closure of coronary pseudoaneurysms may be more common in clinical practice than previously thought, but few cases have been reported. As the natural history of post-intervention coronary pseudoaneurysms has been little investigated, reports of their occurrence may help to clarify their evolution.
Pseudoaneurimas coronários são raramente encontrados durante procedimentos hemodinâmicos e os dados na literatura sobre sua evolução são escassos. Relatamos o caso de um homem de 62 anos, admitido em nosso serviço com enfarte agudo do miocárdio de parede anterior, que desenvolveu um pseudoaneurisma da artéria descendente anterior após perfuração coronária durante a angioplastia primária. Durante o planeamento terapêutico para o tratamento invasivo do pseudoaneurisma, verificamos que ocluiu espontaneamente. Existem poucos relatos de oclusões espontâneas de pseudoaneurismas coronários na literatura, podendo ser um evento mais comum do que previamente pensado. Como a história natural dos pseudoaneurismas coronários é pouco conhecida, o relato de sua ocorrência e evolução pode ser útil no manejo de futuros casos.
Coronary pseudoaneurysms are a rare finding during coronary angiography. Cases have been reported after chest trauma,1 systemic inflammatory vascular disease,2 cardiac tumors,3 and most commonly after catheter-based coronary interventions.4 Post-intervention coronary pseudoaneurysms generally originate from traumatic dissection or perforation of a coronary artery.5,6 They are more frequently found during subsequent angiography in patients with recurrent post-intervention angina or in those who have a new intervention scheduled. In this report, we describe the case of a post-intervention pseudoaneurysm in a patient with acute myocardial infarction that resolved spontaneously during hospital follow-up.
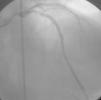
Case reportA 62-year-old man was admitted to the emergency room with chest pain that began 60 minutes before admission. A 12-lead electrocardiogram in the emergency room revealed ST-segment elevation in leads V1–V6 and DI and AVL, confirming the diagnosis of anterior myocardial infarction with ST-segment elevation. His medical history included hypertension and hypercholesterolemia. The patient was taken to the catheterization laboratory, where urgent coronary angiography showed severe obstruction and thrombus in the mid portion of the left anterior descending (LAD) coronary artery and moderate to severe stenosis in the proximal portion. An anomalous right coronary artery (RCA) that was difficult to catheterize was also observed during angiography. Balloon predilatation of the mid LAD lesion was performed and, after implantation of a 3.5×32 mm Liberté stent (Boston Scientific) deployed at 14 atm, a type I perforation was noted (Figure 1), which was successfully treated with prolonged balloon inflation and protamine. The mid LAD angioplasty ended successfully, with TIMI grade 3 flow and no residual perforation, and the proximal LAD lesion was staged. A two-dimensional echocardiogram performed one hour after the coronary angiogram in the intensive care unit showed mid-apical akinesia of the left ventricular anterior wall and no pericardial effusion.
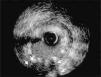
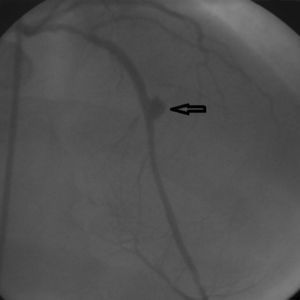
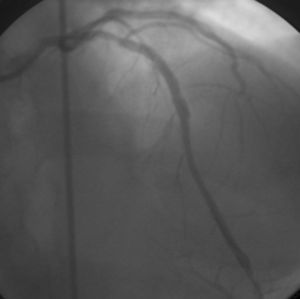
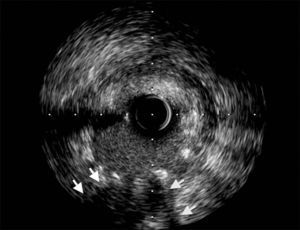
The patient presented signs of heart failure with pulmonary congestion that was successfully treated with vasodilators and intravenous diuretics during the following days. On the eighth day after admission, a second coronary angiography was performed to better assess the lesion in the proximal LAD and the RCA anatomy, which revealed an anomalous origin RCA without obstructive stenosis, severe stenosis in the proximal LAD and a moderate size saccular formation in the mid LAD at the same site as the previous coronary perforation, suggestive of a coronary pseudoaneurysm (Figure 2). After discussion with the hospital's heart team, a third coronary intervention was scheduled for the next day to seal the pseudoaneurysm with a mesh-covered stent (MGuard) and to treat the proximal LAD stenosis with an everolimus-eluting stent. During the third coronary angiography, in the same projection of the left coronary artery, it was noted that the pseudoaneurysm had spontaneously closed (Figure 3). Intravascular ultrasound of the LAD during the third coronary intervention showed loss of vessel wall integrity, damage to the adventitia and hyperechogenicity, suggesting a thrombosed pseudoaneurysm (Figure 4). The intervention was accordingly limited to stent implantation in the proximal LAD. The patient was discharged from the hospital two days after the third intervention, medicated with aspirin, ticagrelor, enalapril, carvedilol and atorvastatin. At one-month follow-up, he was in good clinical condition.
The natural history of coronary pseudoaneurysms is not well defined, but concern exists about the risk of rupture leading to cardiac tamponade or distal embolization.7 Although there is little consensus in the literature, the treatment of moderate and large coronary pseudoaneurysms generally involves interventional procedures such as surgical resection of the pseudoaneurysm8 and use of covered stents9 or spring coils.10
We report a case of spontaneous closure of a perforation-related coronary pseudoaneurysm. Excessive distention during balloon angioplasty, implantation of a stent with greater caliber than the coronary luminal diameter, and calcified coronary lesions are possible factors associated with coronary perforation. There are few reported cases of spontaneous closure of coronary pseudoaneurysms in the literature.11,12 This is probably related to the difficulty in diagnosing pseudoaneurysms before spontaneous closure. Chen et al. described a case of a pseudoaneurysm after an intervention with a paclitaxel-eluting stent in the proximal LAD that was managed conservatively, spontaneous closure occurring two years after the initial diagnosis.12 In another report, a coronary pseudoaneurysm of the circumflex artery closed spontaneously after a few days of follow-up.11 Spontaneous closure of coronary pseudoaneurysms may be more common in clinical practice than previously thought, but few cases have been reported. As the natural history of post-intervention coronary pseudoaneurysms has been little investigated, reports of their occurrence may help to clarify their evolution. However, the lack of knowledge of the natural history and the risks associated with coronary pseudoaneurysms mean that more data are needed to determine the best approach to these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.