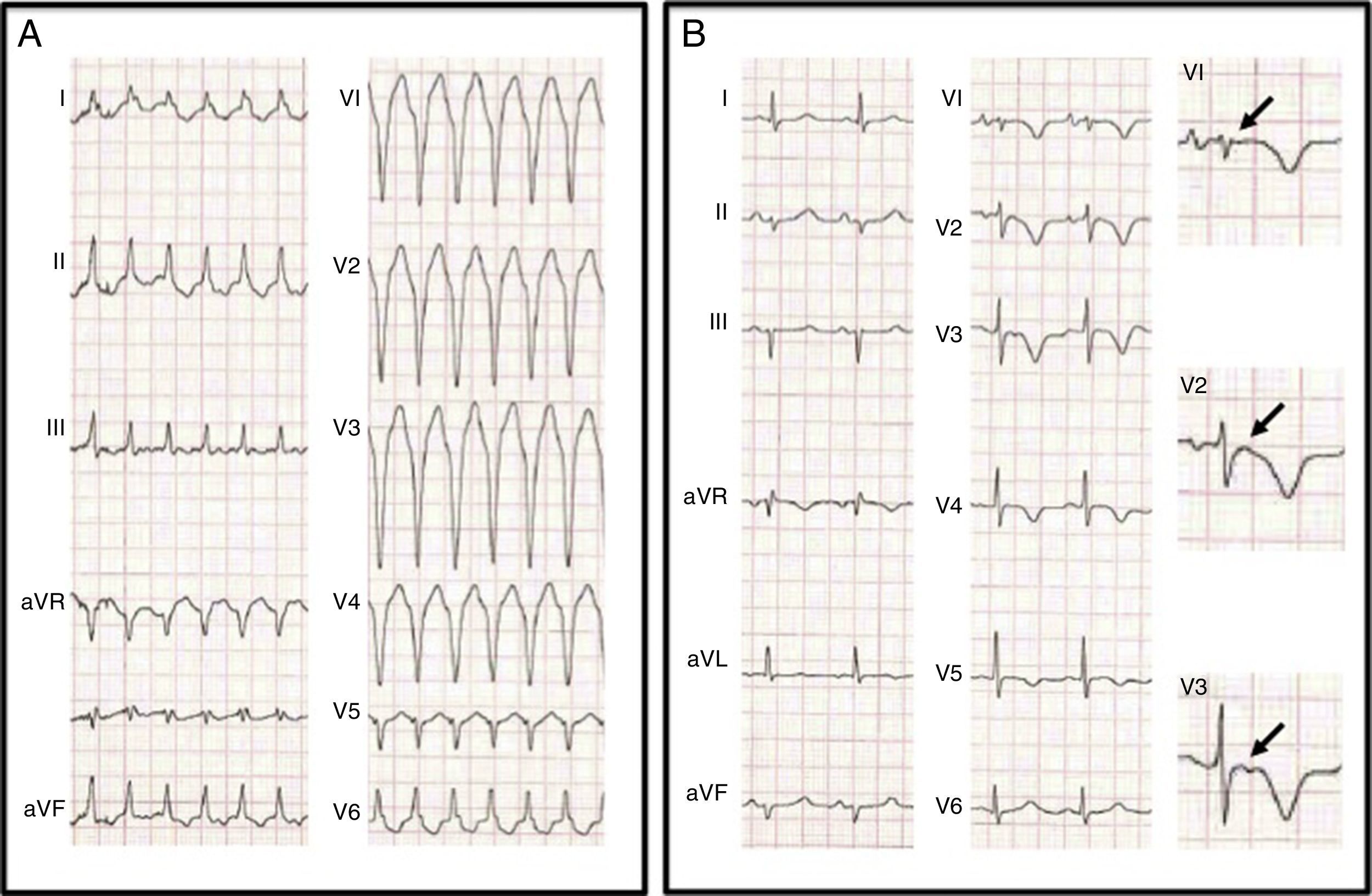
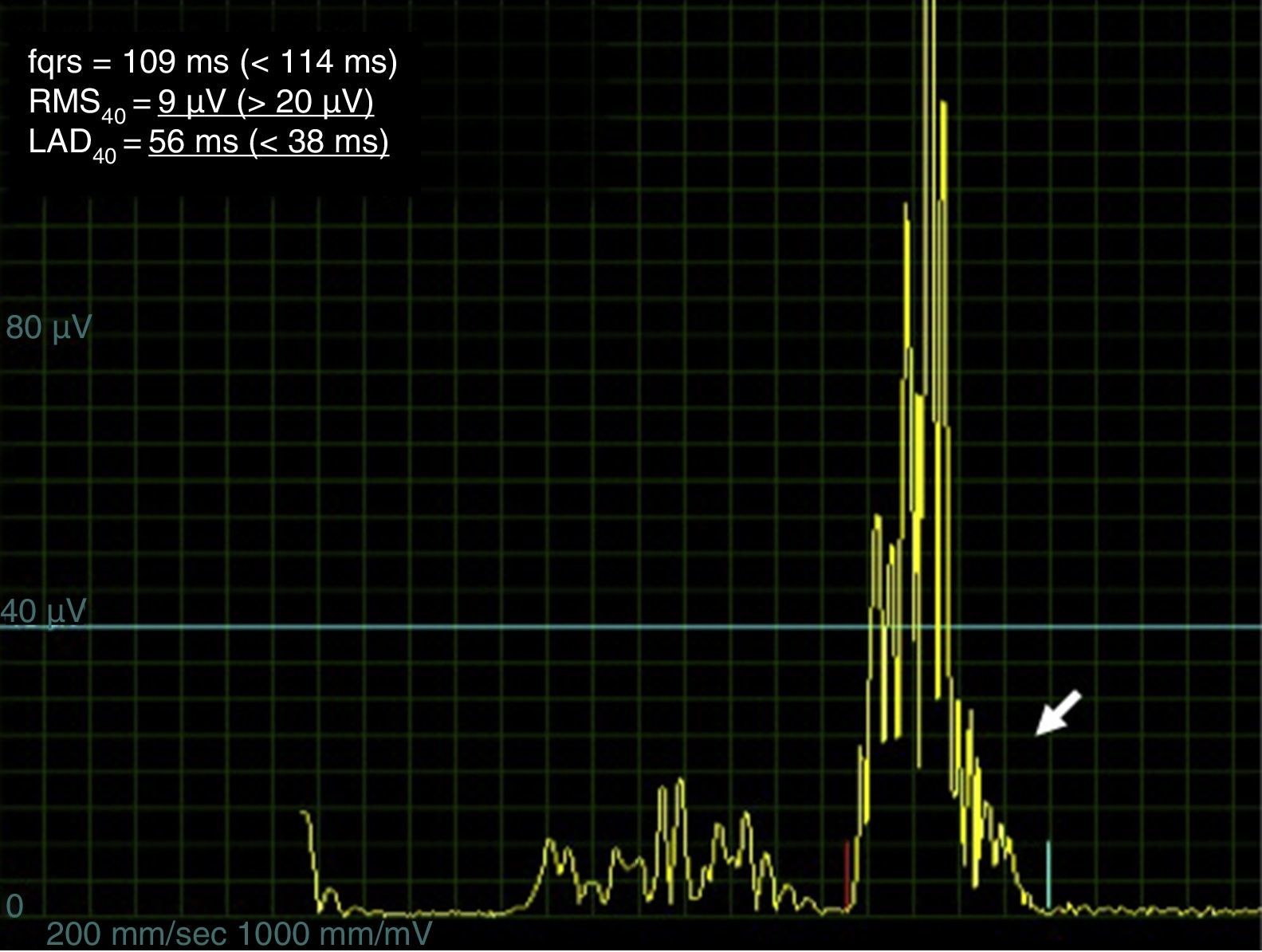
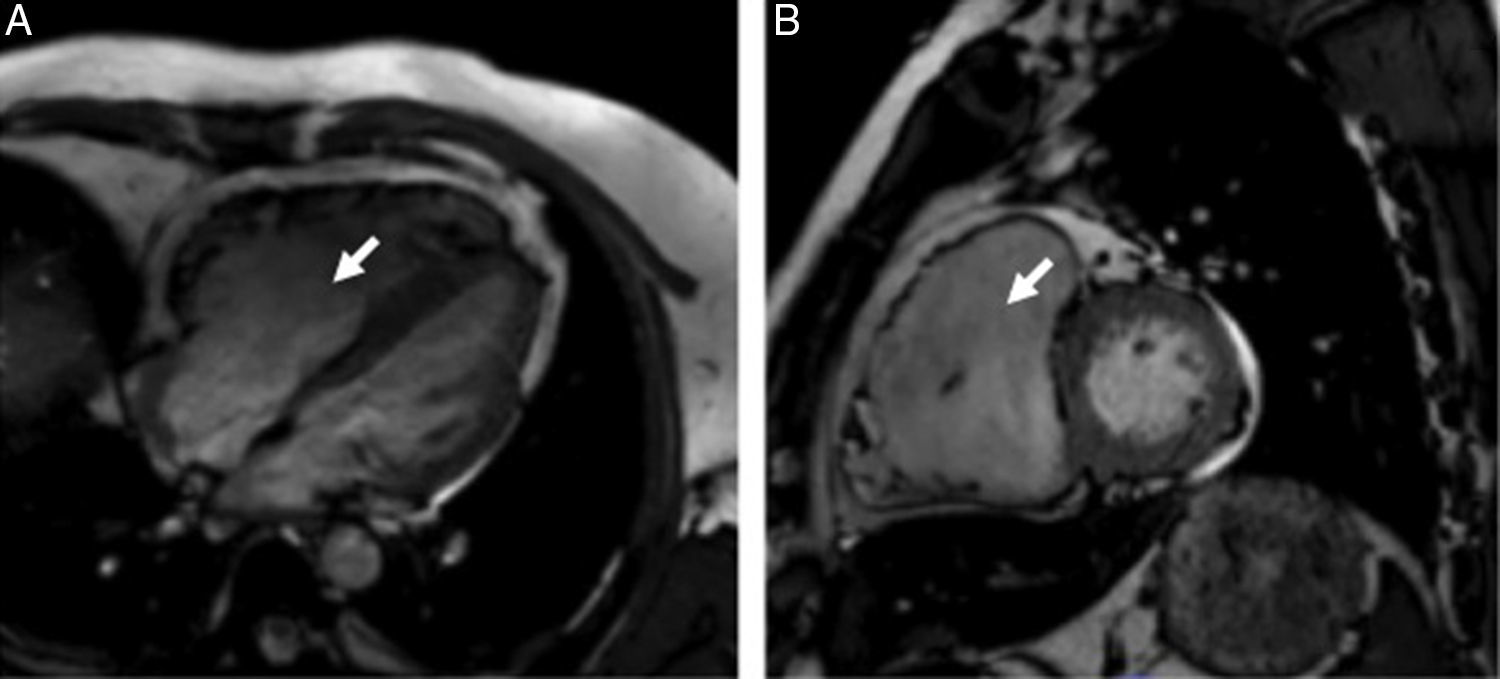
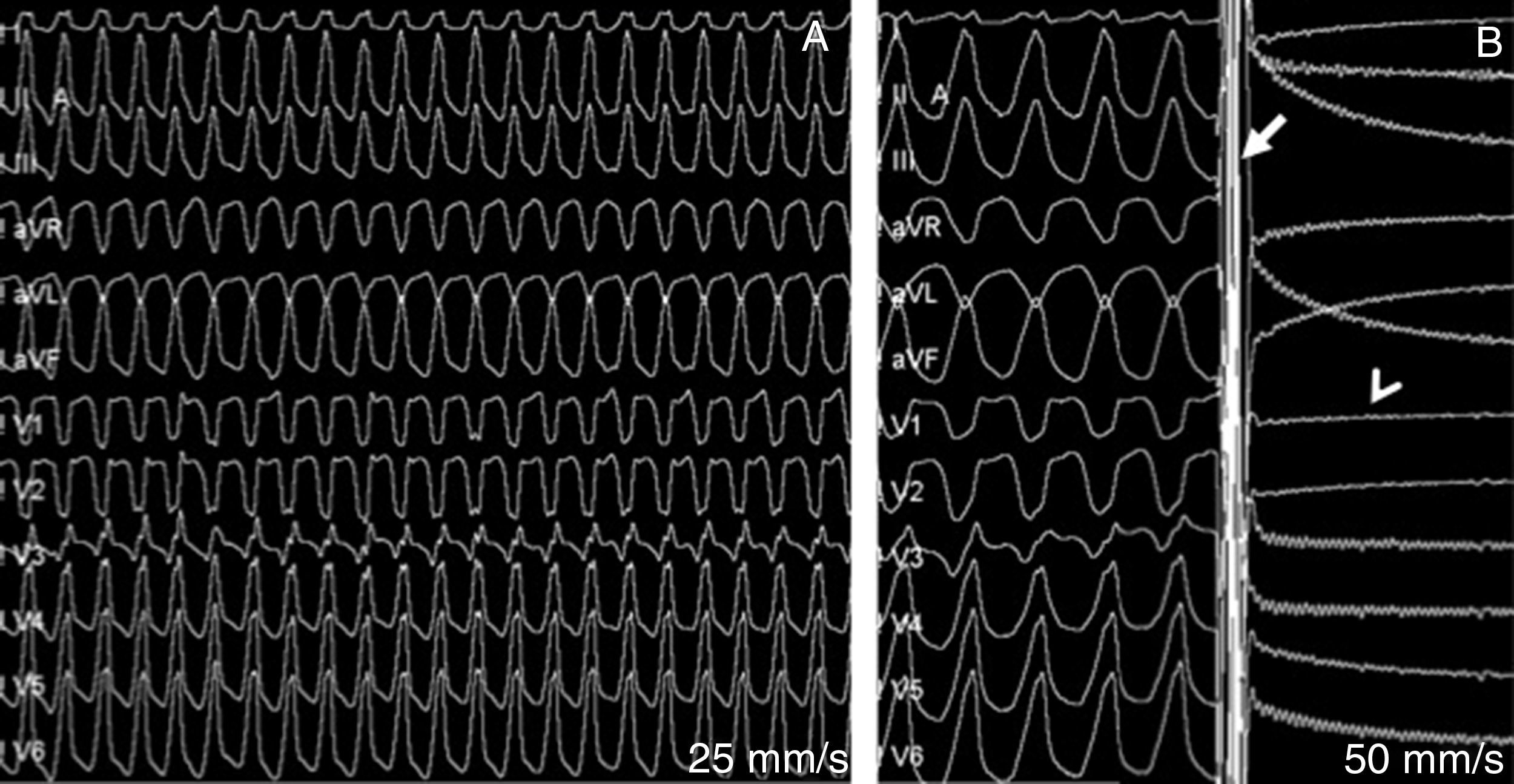
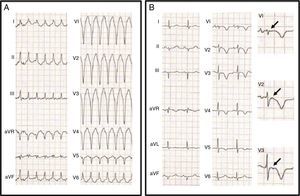
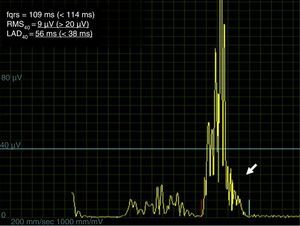
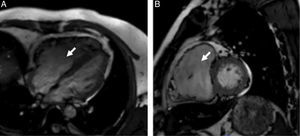
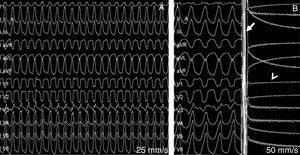
A previously healthy 44-year-old male with unremarkable family history presented to the emergency department with fast palpitations. The electrocardiogram (ECG) revealed a wide QRS tachycardia, 190 bpm, with a left bundle branch block pattern and inferior axis, QS morphology in V1 and RS transition at V6, suggestive of ventricular tachycardia (VT) originating in the right ventricle (RV) (Figure 1A). After synchronized electric cardioversion, the ECG (Figure 1B) showed deep inverted T waves from V1 to V5 and small post-QRS positive inflections suggestive of epsilon waves in the right precordial leads, which raised suspicion of arrhythmogenic right ventricular cardiomyopathy (ARVC). Signal-averaged ECG demonstrated the presence of late potentials (Figure 2). Cardiac magnetic resonance revealed a severely dilated thin-walled right ventricle, with 7% ejection fraction and akinesia of the free wall (Figure 3; Supplementary Videos 1 and 2), confirming the diagnosis of ARVC. The patient underwent electrophysiology study with induction of several VTs of different morphology originating in the RV and hemodynamic collapse, requiring defibrillation (Figure 4). An implantable cardioverter-defibrillator was implanted and the patient was discharged on sotalol. At one year of follow-up he remains asymptomatic and has had no further arrhythmic events.
(A) 12-lead electrocardiogram (ECG) showing a wide QRS tachycardia, 190 bpm, left bundle branch block pattern with inferior axis, QS morphology in V1 and RS transition at V6; (B) 12-lead ECG after synchronized electric cardioversion revealing epsilon waves (arrows) in the right precordial leads and inverted T waves from V1 to V5.
Signal-averaged electrocardiogram revealing the presence of late potentials (arrow), namely RMS40=9 μV and LAD40=56 ms. Normal values are presented in brackets. fQRS: filtered QRS duration; RMS40: root-mean-square voltage of the terminal 40 ms of the QRS; LAD40: low-amplitude (below 40 μV) signal duration.
The classic ECG is a critical diagnostic tool in cardiology. This case demonstrates the importance of the sinus rhythm ECG in the etiological diagnosis of VT.
Conflicts of interestThe authors have no conflicts of interest to declare.
The following are the supplementary material to this article: