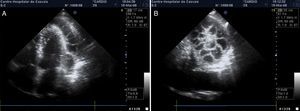
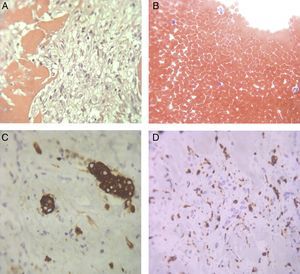
A 58-year-old immunocompetent man with a history of peptic ulcer and orthostatic hypotension was referred for hospital admission by his cardiologist. Pleuritic chest pain, fever (maximum temperature 38.5°C), anorexia and pericardial effusion (12 mm) had begun a month previously. Given the suspicion of pericarditis, he was prescribed aspirin 1 g daily for six days, but without improvement. Initial assessment in the Emergency Department also revealed orthopnea, hypoxemia (pO2 59.5 mmHg; FiO2 0.21), bilateral pleural effusion (a lymphocyte-rich exudate), normocytic normochromic anemia (hemoglobin 115 g/l), C-reactive protein 19.2 mg/dl, and erythrocyte sedimentation rate 120 mm/h. The ECG showed sinus rhythm and nonspecific repolarization changes. He was admitted for further investigation, and oxygen therapy and respiratory physiotherapy were begun, as well as paracetamol for temperatures over 38°C. Two days later repeat echocardiography showed a spiderweb appearance of the pericardium, formed by side-to-side connections of fibrin strands (Figure 1). Pericardiocentesis with biopsy was performed, revealing an inflammatory infiltrate with fibrin (Figure 2). Serological studies revealed a parvovirus B19 infection: IgM 6.04 UA/ml (normal <1.0) and IgG 4.41 UA/ml (normal <1.0). All other serological studies, blood, urine and pleural effusion cultures, and requested autoimmunity markers were negative. The patient was discharged 28 days after admission following remission of clinical symptoms and normalization of imaging and laboratory parameters. Three years later, he has no oncological, autoimmune or infectious disease.
Infection by parvovirus B19 is common. Most adults with parvovirus B19 infection are asymptomatic. Although it is a well-known cause of pericarditis, severe situations like the one presented are rare in patients with no type of immunodeficiency.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank the staff of the Cardiology Department, Dr. José de Almeida Hospital, particularly Élia Baptista, for her assistance with the echocardiographic images. They are also grateful to Ana Paula Martins (Pathology Department, Santa Cruz Hospital) for microscopy analysis of the biopsy samples.
Please cite this article as: Salvado R, Guimarães M, Araújo M, et al. Uma teia de aranha no coração. Rev Port Cardiol. 2014;33:255–257.