We present the case of a woman diagnosed with hypertrophic cardiomyopathy who suffered a myocardial infarction when she was 28 years old, without coronary artery disease on coronary angiography. Two years later, she presented signs of heart failure and left ventricular systolic dysfunction with persistent troponin I elevation, followed by progressive worsening of ventricular dysfunction.
Mulher com miocardiopatia hipertrófica, que sofre enfarte do miocárdio aos 28 anos, sem doença coronária angiográfica. Dois anos mais tarde inicia manifestações de insuficiência cardíaca e instala-se disfunção sistólica ventricular esquerda com elevação persistente da troponina I cardíaca. A partir daí houve deterioração progressiva da função ventricular.
Troponin (Tn) is a laboratory marker of myocardial injury that has prognostic value in chronic heart failure (HF).1,2 Elevated troponin I (TnI) at a first HF consultation is associated with higher mortality, but the prognostic significance of persistent Tn elevation has yet to be fully determined.3,4 Assessment of Tn in advanced HF may be useful in risk stratification.1,5,6
Case reportA 35-year-old woman had been diagnosed with hypertrophic cardiomyopathy (HCM) at the age of six months. Her mother, with the same diagnosis and currently 52 years of age, underwent heart transplantation at age 44, and a maternal aunt suffered sudden death at age nine. There was no other relevant family history.
The patient was hospitalized at age 10 for lipothymia and was followed in adult cardiology consultations from age 16, when she was asymptomatic. Echocardiography revealed marked, asymmetric left ventricular (LV) wall hypertrophy with preserved LV ejection fraction (LVEF), right ventricular (RV) hypertrophy and mitral valve dysplasia.
She remained asymptomatic until the age of 28, when she was hospitalized (in November 2006) for non-ST-elevation myocardial infarction (peak TnI 69 μg/l); coronary angiography excluded coronary artery disease. The pre-discharge echocardiogram showed mild LV dilatation, wall motion abnormalities of atypical distribution and LVEF of 55%. She was prescribed bisoprolol and ramipril and referred to the HF clinic.
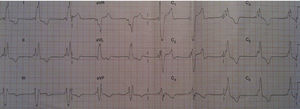
Figure 1 shows the ECG at the first HF consultation. Genetic study identified mutations in the TCAP (c.C410T, p.Thr137lle) and MYH7 (c.C2167T, p.Arg723His) genes. Genetic study of her mother revealed three mutations, one in common with her daughter (MYH7).
A routine consultation in April 2009 for prognostic stratification showed LV systolic dysfunction (LVEF 42%) for the first time and Tn elevation (4.5 μg/l). Table 1 shows changes in levels of Tn and N-terminal pro-brain natriuretic peptide (NT-proBNP), with persistent Tn elevation in follow-up consultations.
Changes in levels of troponin I and N-terminal pro-brain natriuretic peptide.
| Date | TnI (μg/l) | NT-proBNP (pg/ml) |
| March 2009 | 0.71 | 1450 |
| April 2009 | 4.52 | 1370 |
| June 2009 | 5.44 | 1520 |
| November 2009 | 4.47 | 2090 |
| January 2010 | 8.11 | 1930 |
| March 2010 | 9.18 | 1430 |
| June 2010 | 5.47 | 1160 |
| November 2010 | 6.3 | 1130 |
| January 2011 | 5.65 | 1380 |
| May 2011 | 7.27 | 1200 |
| September 2011 | 2.21 | 2170 |
| October 2011 | 5.43 | 2370 |
| December 2011 | 4.77 | 1880 |
| January 2012 | 4.96 | 2040 |
NT-proBNP: N-terminal pro-brain natriuretic peptide; TnI: troponin I.
The patient was asymptomatic until July 2009, when she presented NYHA class II HF. Due to progressively worsening symptoms, furosemide was begun in November 2009 and HF therapy was optimized. Echocardiography in the same month revealed worsening LV systolic function (LVEF <35%) compared to the previous echocardiogram, together with a reduction in dP/dt and increases in mitral regurgitation and in pulmonary artery systolic pressure (48 mmHg). Phenotypic alterations were also observed in the LV posterior and lateral walls, the endocardial border showing small protrusions similar to LV noncompaction. Cardiac magnetic resonance imaging revealed thrombi in the RV apex and left atrial appendage. Irregularities in LV trabeculation were observed, although without criteria for myocardial noncompaction. Oral anticoagulation with warfarin was begun for a target INR of 2.0–3.0.
An implantable cardioverter-defibrillator was implanted in May 2010 for primary prevention of sudden cardiac death, after exclusion of thrombi by transesophageal echocardiography.
The patient was stable until May 2011, when clinical worsening was observed. Echocardiography in August 2011 showed severe biventricular systolic dysfunction (LVEF 26%) and she was hospitalized in September 2011 due to electrical storm. She was subsequently discharged medicated with amiodarone.
In the course of evaluation for heart transplantation, pulmonary artery catheterization (PAC) was performed, which showed marked pulmonary hypertension (mean pulmonary artery pressure 50 mmHg and pulmonary vascular resistance [PVR] 10.4 Wood units, without significant reversibility with high-flow oxygen). Pulmonary ventilation/perfusion scintigraphy excluded pulmonary thromboembolism. Sildenafil was prescribed.
PAC was repeated after six months of sildenafil therapy, which showed PVR had fallen from 15.6 to 3.6 Wood units, with inhaled nitric oxide.
In April 2012, the patient was in NYHA class III, and underwent heart transplantation the following month, which was uneventful and she was discharged clinically stable.
Sildenafil was electively discontinued three months after transplantation. The patient's clinical course has been favorable, with no episodes of acute rejection or infection, and she is currently in NYHA class I.
Discussion and conclusionsThe case presented illustrates a rare clinical course of HCM. The prevalence of end-stage HCM varies between 2.4% and 15% depending on the series7; 5% of HCM patients have two or more mutations8,9 and the presence of multiple mutations is associated with more severe disease.10
This case also highlights the adverse prognostic significance of persistent Tn elevation in chronic HF. Tn elevation mat be due to various factors and is associated with worse prognosis. The case presented suggests that it may have been due to progressive deterioration of LV systolic function, given that the latter began at the same time as persistently elevated Tn was observed. Only 10.4% of HF patients have detectable Tn (>0.01 ng/ml), 2 although more marked elevation is seen in acute HF11–13 but only 6.2% of these patients have elevation of >0.1 ng/ml.14
Finally, the case illustrates the value of pulmonary vasodilatory therapy as a bridge to heart transplantation in selected patients with HF and increased pulmonary vascular resistance.15
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank Dr. Isabel Gaspar, consultant in cardiac genetics at Centro Hospitalar Lisboa Ocidental, for her invaluable contribution to the genetic study in this case.
Please cite this article as: Cardoso G, Aguiar C, Ventosa A, et al. Um caso raro de elevação persistente da troponina em doente com insuficiência cardíaca crónica. Rev Port Cardiol. 2013;32:931–933.