A young male presented with a right parasternal stab wound. The chest radiography was normal and transthoracic echocardiography ruled out pericardial tamponade. He remained hemodynamically stable until three hours later when signs of progressive anemia were observed. Chest computed tomography showed massive right-sided hemothorax. The patient underwent surgery, which revealed an active bleeding atriopleural fistula connecting the right atrium and draining into the right pleura resulting from the negative pressure generated during respiration. This mechanism prevented cardiac tamponade and maintained initial hemodynamically stability.
Um jovem foi transferido para o serviço de emergência da nossa instituição com uma facada paraesternal direita. A radiografia de tórax foi normal. A ecocardiografia transtorácica descartou a presença de derrame pericárdico. Manteve-se hemodinamicamente estável até ao fim de três horas, após o que o paciente começou a apresentar sinais de anemia progressiva. Foi realizada tomografia computadorizada de tórax que mostrou hemotórax maciço. O paciente foi encaminhado urgentemente para cirurgia cardíaca. Observou-se hemorragia ativa através de uma fístula corte pleural ligando o átrio direito/a aurícula direita e drenagem pleural direita, resultado da pressão negativa da pleura durante a respiração. Este mecanismo impediu o tamponamento cardíaco e explica a estabilidade hemodinâmica inicial.
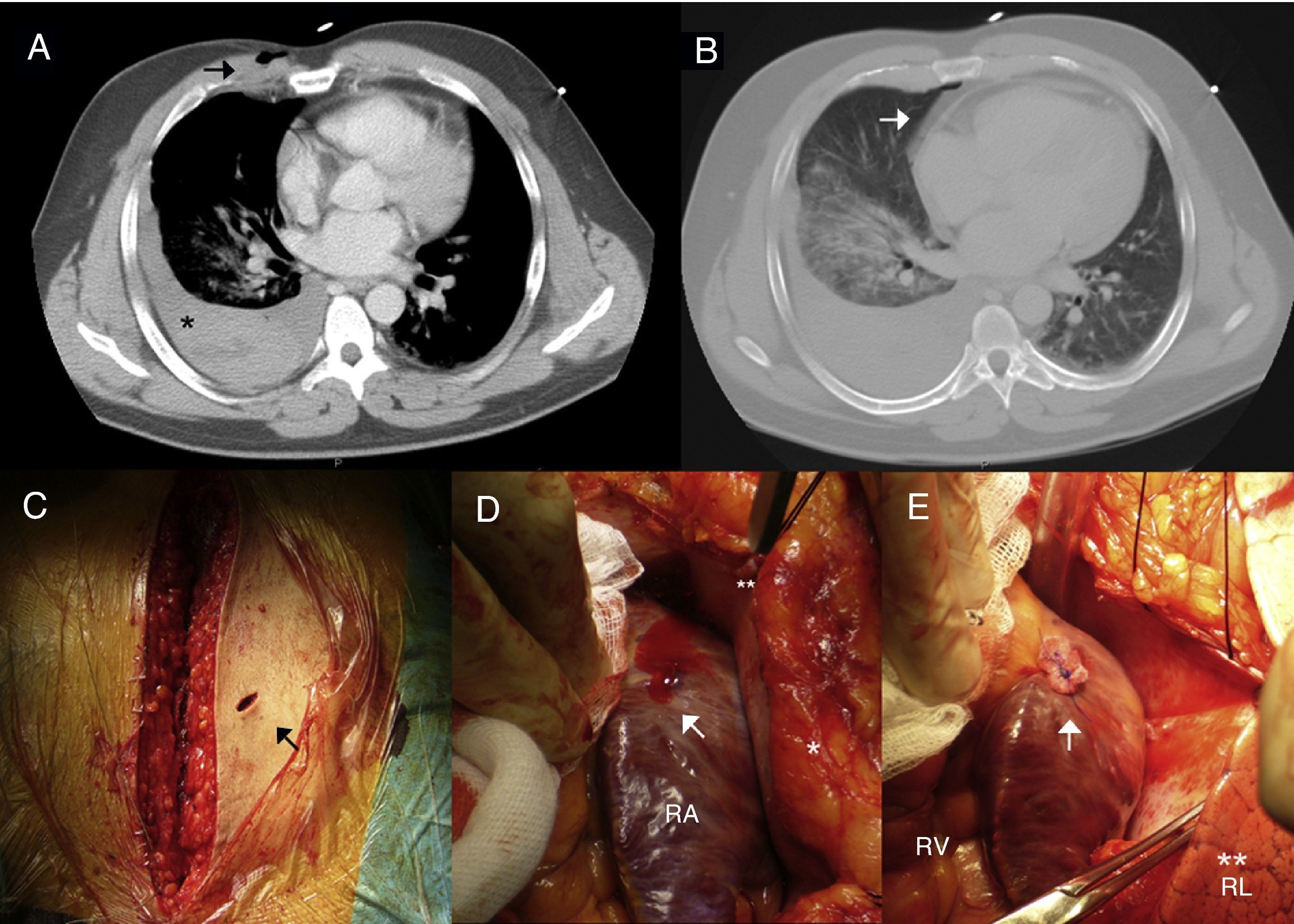
A 36-year-old-male, previously healthy, was admitted to the emergency department presenting a right parasternal knife stab wound in the third intercostal space after a street fight. On physical examination, no other lesions was detected except for ecchymotic lesions around the face and both arms. The patient remained hemodynamically stable. Despite the location and depth of the stab wound, the patient presented no clinical signs of cardiac trauma (no jugular distention, hypotension or tachycardia), normal ECG and no increase in cardiac enzymes. The initial chest radiography showed no abnormalities and transthoracic echocardiography showed no pericardial effusion. Because of the patient's hemodynamic stability and uneventful initial course, conservative management was adopted. However, three hours after admission signs of progressive anemia and low hematocrit in laboratory tests were observed (hematocrit 24%; hemoglobin 8 g/dl), suggesting internal bleeding. Echocardiography was accordingly repeated, which remained normal. A chest computed tomography (CT) scan was then performed to investigate internal bleeding, which showed the trajectory of the chest stab wound and severe right-sided hemothorax. No pericardial tamponade was detected by echocardiography (Figure 1A and B). The patient was immediately taken to the operating room for surgical review, via a median sternotomy because of the stab wound trajectory. A 1-cm parasternal incised wound was located crossing the chest (Figure 1C). No pericardial effusion or cardiac tamponade was seen. However, a concealed active bleeding atriopleural fistula connecting the right atrium (RA) and draining into the right pleural cavity was detected (Figure 1D). The wound path crossed the mediastinum and pleura and reached the RA manifesting as an atriopleural fistula. Massive right-sided hemothorax was confirmed. The wound in the RA had presumably been draining into the right pleural cavity from the time of the street fight until surgery, due to the negative pressure generated by respiratory movements. The size of the pleural cavity enabled a large quantity of blood to accumulate without hemodynamic instability. This mechanism caused a massive pleural effusion and prevented initial cardiac tamponade, and was the reason that the patient remained hemodynamically stable during the first hours after the fight. The injury to the RA was repaired by direct suture with a non-absorbable 4-0 polypropylene suture buttressed with Teflon felt, and the right pleural effusion was drained (Figure 1E). A chest drain was placed and removed two days after surgery. The patient was discharged uneventfully five days after surgery.
Computed tomography images showing (A) chest stab wound (arrow) and severe secondary right hemothorax with different densities inside suggesting different stages of bleeding (*) and (B) no pericardial effusion; (C) median sternotomy showing parasternal stab wound with no active bleeding (arrow); (D) active bleeding stab wound in the right atrium (arrow); the right lung is covered by the pleura (*); **: pericardial membrane; (E) stab wound in the right atrium sutured with a polypropylene suture buttressed with Teflon felt (arrow). The right lung is visible as the pericardium and right pleura are open (**). RA: right atrium; RL: right lung; RV: right ventricle.
The incidence of penetrating traumas, particularly stab wounds, is increasing; they are the major cause of cardiac trauma.1 Potentially deadly, stab wounds need rapid management to reduce complications and alleviate any bleeding.2
When the wound is located in the chest, any life-threatening involvement of the heart or great vessels must be ruled out. Generally, when a patient is unstable, the diagnosis is straightforward, and a severe lesion in the heart or great vessels is easily suspected. Pericardial tamponade is the most frequent mechanism that leads to secondary clinical instability.3,6 However, if the patient remains hemodynamically stable, it is possible to underestimate the severity of the lesions and the associated risk. Internal bleeding can manifest differently from bleeding from the heart to the pleura. Although such bleeding may initially be well tolerated in a young patient, it can lead to a misdiagnosis.2–5
Even if all initial examinations are normal, the lesion must not be underestimated and other mechanisms of injury should be considered, since hemodynamic stability can rapidly reverse and become an emergency.2 Correct diagnosis is thus essential. Chest computed tomography is a useful modality for the evaluation of cardiac injuries in high-risk stable patients.2,6 Our intention with this case report is to highlight the importance of close monitoring of patients during the first hours after the event to detect any signs that could indicate a severe complication and to ensure proper treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Arnáiz-García ME, Arnáiz J, Pontón A, Pulitani I, González-Santos JM, Arévalo-Abascal A, et al. Fístula átrio-pleural/aurículo pleural oculta resultante de uma facada cardíaca penetrante/profunda 2014. Rev Port Cardiol. 2014;33:567.