Infective endocarditis continues to be associated with high mortality, despite the medical and surgical therapeutic options available. Surgical intervention is indicated in cases of heart failure or uncontrolled infection and sometimes for the prevention of embolic phenomena. The authors present the case of a 56-year-old male patient, with fibro-calcific mitral–aortic valve disease, splenectomized and with recently relapsed Hodgkin's lymphoma, who was admitted with infective endocarditis due to Streptococcus dysgalactiae. On the thirtieth day of directed antibiotic therapy, the mitral vegetation showed a significant increase in size and mobility. Surgery was considered at this point. However, given the patient's clinical stability and laboratory results, it was decided to adopt a conservative approach and to extend antibiotic therapy. The vegetation had regressed considerably seven days later. Given this atypical vegetation behavior, with slower than usual regression for the causative agent, the authors suggest that antibiotic therapy should be extended in patients with some degree of immunosuppression.
A endocardite infecciosa é uma doença cuja mortalidade, apesar das opções terapêuticas médicas e cirúrgicas existentes, se mantém elevada. A intervenção cirúrgica está indicada em casos de insuficiência cardíaca directamente relacionada com a disfunção valvular, infecção não controlada e, por vezes, na prevenção de fenómenos embólicos. Os autores descrevem o caso de um doente de 56 anos, com doença degenerativa mitro-aórtica, esplenectomizado e com Linfoma de Hodgkin recentemente recidivado, internado por endocardite infecciosa a Streptococcus dysgalactiae. Ao trigésimo dia de antibioticoterapia dirigida verificou-se um aumento significativo do volume e mobilidade da vegetação mitral, tendo sido equacionada a opção cirúrgica. No entanto, e dada a estabilidade clínica e analítica do doente, optou-se por uma atitude conservadora com prolongamento da antibioticoterapia. Foi constatada regressão franca da vegetação sete dias depois. Dado o comportamento atípico da vegetação com regressão mais lenta que o habitual para o agente em causa, os autores sugerem que em doentes com algum grau de imunocompromisso, a antibioticoterapia deva ser mais prolongada.
Although the epidemiology of infective endocarditis has changed over the last 50 years, with rheumatic heart disease becoming less common and degenerative valve disease more frequent, its incidence and associated mortality have remained constant.1
Annual incidence is 4–10 per 100000 population, and it is slightly more common in men; despite sophisticated diagnostic and therapeutic techniques, mortality remains high, at 1/100000 per year.2,3
The treatment goals for infective endocarditis are eradication of the microorganism responsible and resolution of any intra- and extracardiac infectious complications. The first is usually achieved with prompt intravenous antibiotic therapy directed at the causative agent, while the second often requires surgical intervention.
The antibiotic therapeutic regime chosen depends on the type of valve involved (native or prosthetic), time between prosthetic valve implantation and infection (more or less than a year) and the etiological agent, when identified.4
There is little evidence in the literature on the most appropriate duration of antibiotic therapy in infective endocarditis due to non-opportunistic bacterial pathogens in immunocompromised patients.
Case reportWe report the case of a 56-year-old male patient, with fibro-calcific mitral–aortic valve disease but no significant functional impairment, hypertensive, splenectomized in 1980 in the context of Hodgkin's lymphoma diagnosed in that year, with recent abdominal relapse.
He was admitted to the Portuguese Institute of Oncology in Lisbon on October 13, 2010 in septic shock. Inotropic support was begun, together with antibiotic therapy with piperacillin–tazobactam, to which vancomycin was added following isolation of Streptococcus dysgalactiae in blood cultures. Transesophageal echocardiography (TEE) revealed vegetations on the mitral and aortic valves. Disease staging showed multiple subdiaphragmatic adenopathies, which biopsy revealed as relapsed Hodgkin's lymphoma.
The patient was transferred to our hospital on October 28, 2010, clinically stable, with a diagnosis of infective endocarditis of the mitral and aortic valves due to S. dysgalactiae. Following antibiotic susceptibility testing, therapy was changed to ceftriaxone, together with gentamicin for the first week.
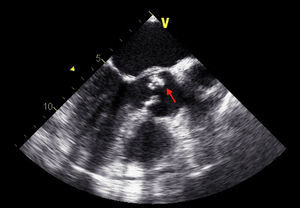
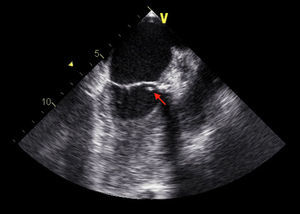
TEE on admission showed a moderately thickened aortic valve with slightly reduced opening, mild regurgitation and a small mobile vegetation approximately 5mm long attached to the arterial side of the aortic valve (Figures 1 and 2). There was also an image suggestive of a vegetation around 5mm long on the mitral valve adjacent to the basal portion of the ventricular side of the anterior leaflet, with moderate annular calcification and mild regurgitation (Figure 3).
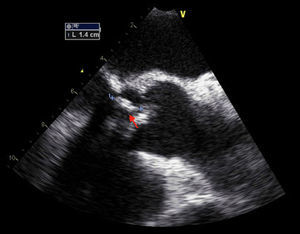
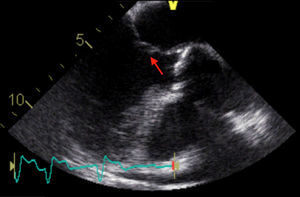
The patient remained clinically stable and asymptomatic during hospital stay on directed antibiotic therapy. On the 31st day of therapy, the aortic vegetation had disappeared on transthoracic and transesophageal echocardiography, but the mitral vegetation showed a significant increase in length (14mm) and mobility, with a longer stalk and clearly rounded extremity (Figure 4); the vegetation was highly mobile in the left ventricular outflow tract, coming into contact with the ventricular side of the aortic cusps during systole, indicating a high embolic risk.
Given the characteristics of the vegetation and the duration of antibiotic therapy, surgical intervention was considered at this point.
However, in view of the patient's comorbidities, particularly immunosuppression, clinical stability (apyretic, with no signs of heart failure or systemic embolism) and laboratory results (C-reactive protein <2mg/dl, with no leukocytosis) and absence of local complications, it was decided to adopt a wait-and-see approach and to extend antibiotic therapy. Transthoracic echocardiography was repeated seven days later, which showed a marked reduction in the size and mobility of the mitral vegetation, a finding confirmed by TEE (Figure 5) on the 46th day of antibiotic therapy. The patient was discharged and remains asymptomatic, with negative blood cultures.
DiscussionAround half of cases of infective endocarditis are treated surgically due to serious complications.5 While this option should be considered in the active phase of the disease to prevent progression of heart failure, irreversible structural damage and systemic embolism, this phase is also associated with higher operative risk.6
Current indications for surgical treatment are: (1) refractory heart failure directly related to valve dysfunction; (2) uncontrolled infection; and (3) prevention of embolic phenomena.7
The risk of embolism is high (20–50%) in patients with infective endocarditis, though it decreases rapidly following institution of directed antibiotic therapy, particularly after two weeks.8
The embolic risk of vegetations is closely linked to their size and mobility, and surgery is recommended for those measuring >10mm in diameter after one or more embolic events, for those associated with predictors of unfavorable evolution such as heart failure or persistent infection, and especially for those measuring >15mm, the latter being a class IIb recommendation, level of evidence C.9
There are few reports of endocarditis in immunocompromised patients, particularly in cases of non-opportunistic infection, and this situation is not specifically addressed in the guidelines.
While infection due to S. dysgalactiae, which belongs to Lancefield serogroups C and G, may be associated with a higher risk of local complications, particularly abscesses, it does not require prolonged antibiotic therapy in the case of native valves, although short-duration treatment (less than two weeks) is contraindicated.10,11
The atypical behavior of the vegetation in the case presented, with slower than usual regression for the causative agent, suggests that antibiotic therapy should be extended in patients with some degree of immunosuppression.
ConclusionsThe present case illustrates an unusual evolution of infective endocarditis and highlights the need for a carefully considered approach, based not only on the guidelines but also on assessment of the risks and benefits of surgical intervention, taking into account the patient's characteristics, clinical course, laboratory results and imaging studies, and duration of antibiotic therapy, in order to decide on the best therapeutic option.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carvalho, M.S. Um caso de endocardite infecciosa de válvula nativa em doente imunocomprometido. doi 10.1016/j.repc.2011.10.009.