The authors describe the case of a 59-year-old man, a former smoker, with hypertension, chronic renal failure undergoing hemodialysis, and a history of stent grafting for repair of an abdominal aortic aneurysm and miliary tuberculosis, who was diagnosed with constrictive pericarditis and a thoracic aortic aneurysm. In a patient with such a complex medical history, there were several etiologies to consider. The treatment consisted of pericardiectomy and a hybrid technique of supra-aortic debranching and subsequent endovascular stent-graft repair.
Os autores descrevem o caso de um doente do sexo masculino, de 59 anos, hipertenso, ex-fumador, insuficiente renal crónico em hemodiálise, com antecedentes de endoprótese por aneurisma da aorta abdominal e história de tuberculose miliar no passado, a quem é diagnosticado pericardite constritiva e aneurisma da aorta torácica. Num doente com antecedentes patológicos tão diversos, são várias as etiologias a considerar. O tratamento consistiu numa pericardiectomia e numa técnica híbrida de debranching dos ramos supra-aórticos com posterior implantação de endoprótese aórtica.
Constrictive pericarditis is a rare and disabling consequence of pericardial thickening secondary to chronic inflammation, which may be due to infection (particularly tuberculosis, which has a high prevalence in Portugal), or a late complication of mediastinal irradiation, or following cardiac surgery.
Less common causes are connective tissue disease, end-stage renal failure and cancer, although in the latter, the pathophysiology is different since the thickening results not only from the inflammatory process but also from tumor invasion of the pericardium. Treatment consists of pericardiectomy, except in completely asymptomatic cases or in patients contraindicated for this surgical procedure, in whom diuretic therapy may be an option.1–4
Aortic aneurysms, defined as pathological dilatation of ≥1.5 times normal diameter, are usually asymptomatic and are incidental findings on routine exams performed for other reasons. Various risk factors have been suggested, including hypertension, smoking and chronic obstructive pulmonary disease, and a variety of causes have been identified: cystic medial degeneration, atherosclerosis, trauma, inflammation or infection, post-stenotic or post-surgical dilatation, and familial syndromes such as Marfan and Ehlers-Danlos type IV.
The therapeutic approach is often conservative, with medical therapy and vigilance in cases of asymptomatic aneurysms and/or those considered too small for surgical intervention. In symptomatic aneurysms and those of sufficient size, treatment is invasive, with surgical or percutaneous implantation of an endovascular prosthesis.5–7
Case reportA 59-year-old man, a former smoker, with hypertension, chronic renal failure undergoing hemodialysis and a history of miliary tuberculosis in 2002 (under therapy for 12 months), had an abdominal aortic aneurysm diagnosed and treated by implantation of an aortic endoprosthesis in 2005. He had also had ulcerative colitis, treated by total colectomy and ileostomy. He was under medication with atenolol 50 mg, amlodipine 10 mg, indapamide 20 mg, an intestinal anti-inflammatory drug (mesalazine 500 mg), a phosphorus-binding agent and a multivitamin supplement.
He was referred for cardiology consultation in July 2011, complaining of fatigue (New York Heart Association [NYHA] class III). Physical examination revealed no alterations except mild bilateral pretibial edema. The electrocardiogram showed sinus rhythm, heart rate 92 bpm, with left anterior hemiblock, but no other changes.
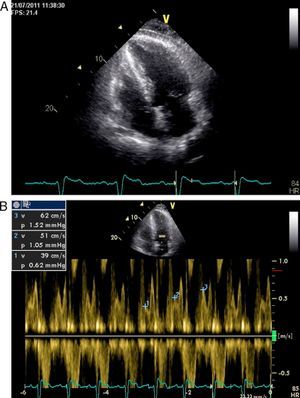
Other diagnostic exams were requested, including transthoracic echocardiography, which showed characteristics compatible with constrictive pericarditis – pericardial thickening with increased echogenicity and significant respiratory variation of the E wave in transmitral flow (Figure 1A and B), together with mildly impaired ejection fraction.
Right and left cardiac catheterization excluded angiographically significant coronary artery lesions; the diagnosis of constrictive pericarditis was confirmed through hemodynamic study, which showed typical dip-and-plateau ventricular pressure curves and equalization of end-diastolic pressures.
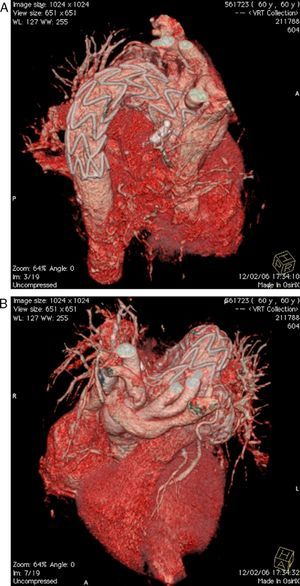
Aortography documented dilatation of the descending thoracic aorta. Chest computed tomography (CT) angiography to better characterize the aorta revealed a large, partially thrombosed, saccular aneurysm originating in the descending thoracic aorta, immediately distal to the emergence of the left subclavian artery, 87 mm × 61 mm in diameter (Figure 2). No pericardial calcification was observed.
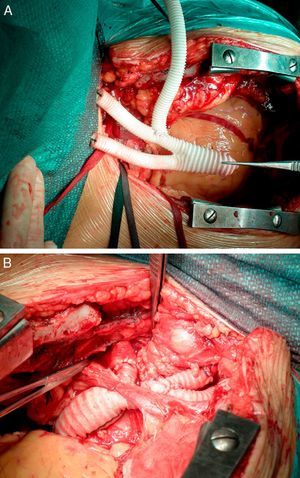
Following joint medical and surgical evaluation, it was decided to adopt a hybrid surgical and percutaneous approach. Surgery consisted of pericardiectomy with total debranching of the supra-aortic branches (left brachiocephalic trunk and carotid and subclavian arteries) with termino-lateral anastomosis of a previously constructed three-branch Dacron graft (Uni-Graft® KUV, B. Braun) (Figure 3A) to the aortic arch, obviating the need for extracorporeal circulation and deep hypothermia (Figure 3B).
Percutaneous implantation of an endoprosthesis in the thoracic aorta (Figure 4) was then performed, taking care not to compromise the emergence of the above vessels.
Anatomopathological study of the pericardium showed non-specific pericarditis. The postoperative period was uneventful and the patient was discharged after nine days.
CT angiography three months after the interventions confirmed a good result (Figure 5).
At six-month follow-up, the patient was in NYHA class II/III, with no complications or rehospitalizations.
DiscussionDescending thoracic aortic aneurysms originating in the aortic arch are not uncommon8 but represent a technical challenge, due to both the involvement of the supra-aortic branches, with their high blood flow, and the curved anatomy and motion of this portion of the aorta during the cardiac cycle.
Conventional surgical treatment requires extracorporeal circulation and deep hypothermia, which, despite advances in knowledge and techniques, still carries significant risk of mortality and morbidity,9 particularly myocardial injury and an appreciable incidence of permanent neurological damage.10
Less invasive strategies, with reduced physiological insult, have therefore become increasingly popular. There is growing evidence that combined percutaneous and surgical treatment of these aneurysms is associated with lower morbidity and mortality in patients who are not ideal candidates for conventional surgery.11–15
Percutaneous implantation of an endoprosthesis is a safe and effective alternative, although it requires a proximal landing zone in the area to be treated that will allow the prosthesis to be anchored without compromising blood supply to the supra-aortic branches. This limitation can be overcome by repositioning these branches proximal to the endoprosthesis implantation site, a technique termed debranching.
Discussion of the etiology of the present case focused on the fact that both the pericardial inflammation and aortic wall degeneration could be cardiovascular manifestations of a single systemic disease.
Although both hypertension and smoking can cause aortic aneurysms, chronic renal failure (by accelerating the atherosclerotic process) and ulcerative colitis (by establishing a systemic inflammatory state) can also be implicated. The latter association has been reported in the literature.16
With regard to pericardial involvement, both chronic renal failure and ulcerative colitis17 are associated, albeit rarely, with chronic pericarditis.
However, tuberculosis, while rarely described in association with aortic aneurysms, is a common cause of constrictive pericarditis (particularly in Portugal), and merits consideration as the cause of both conditions in this case.
Aortic degeneration is a rare sequela of tuberculosis, first described by Weigert in 1882.18 Since then, tuberculous arteritis of the subclavian, carotid, common iliac, hepatic, renal and innominate arteries has been reported.19–21
At least three different mechanisms have been suggested: extension of a contiguous focus of infection (for example, from the pulmonary parenchyma or pericardium to the thoracic aorta or from infected retroperitoneal lymph nodes to the abdominal aorta); hematogenous spread of a pre-existing intimal lesion such as an atherosclerotic plaque; and septic embolism from the arterial wall to vessels or lymph nodes.22,23
Tuberculous aortitis can lead to complete degeneration of the aortic wall or aneurysm formation,24 and diagnosis is a challenge requiring a high level of clinical suspicion.
ConclusionThe case presented is interesting for the variety of cardiovascular diagnoses that could be manifestations of a single disease, for the diagnostic process involved, and for the complex therapeutic solution that combined surgical and percutaneous intervention, a practical illustration of how a heart team works.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carvalho MS, et al. Um caso de pericardite constritiva e aneurisma da aorta torácica: abordagem terapêutica híbrida. Rev Port Cardiol. 2013. http://dx.doi.org/10.1016/j.repc.2012.08.013.