During the Covid-19 pandemic there has been a general belief that hospital admissions for non-infectious causes, especially cardiovascular diseases, have fallen.
ObjectivesTo assess the impact of the pandemic on admissions for ST-elevation myocardial infarction (STEMI) during the first pandemic wave.
MethodsWe performed a multicenter retrospective analysis of consecutive patients presenting with STEMI in two Portuguese hospital centers in two sequential periods – P1 (March 1 to April 30) and P2 (May 1 to June 30). Patient's clinical data and hospital outcomes were compared between the years 2017 to 2019 and 2020 for both periods.
ResultsDuring P1 in 2020, a reduction in the number of STEMI patients was observed in comparison with previous years (26.0±4.2 vs. 16.5±4.9 cases per month; p=0.033), as well as an increase in the number of mechanical complications (0.0% vs. 3.0%; p=0.029). Percutaneous coronary interventions in the setting of failed thrombolysis were more frequent (1.9% vs. 9.1%; p=0.033). An overall trend for longer delays in key timings of STEMI care bundles was noted. Mortality was higher during P1 compared to previous years (1.9% vs. 12.1%; p=0.005).
ConclusionsDuring the first Covid-19 wave fewer patients presented with STEMI at the catheterization laboratory for percutaneous coronary intervention. These patients presented more mechanical complications and higher mortality.
Recentemente durante a pandemia por Covid-19 houve uma perceção global de uma diminuição de admissões hospitalares por causas não infeciosas, em particular por doenças cardiovasculares.
ObjetivosAvaliar o impacto da pandemia nas admissões por enfarte agudo do miocárdio com supradesnivelamento de ST (STEMI), na primeira onda da pandemia.
MétodosAnálise multicêntrica e retrospetiva de doentes consecutivos admitidos em dois hospitais portugueses por STEMI em dois períodos sequenciais - P1 (1 de março a 30 de abril) e P2 (1 de maio a 30 de junho). Foi realizada uma comparação dos dados clínicos e de evolução hospitalar entre 2017 a 2019 e 2020 para os dois períodos.
ResultadosNo P1 de 2020 observou-se, relativamente a anos prévios, uma redução do número de doentes com STEMI (26,0±4,2 versus 16,5±4,9 casos por mês; p=0,033) e um aumento do número de complicações mecânicas (0,0% versus 3,0%; p=0,029). Os casos de angioplastia após trombólise falhada foram mais frequentes (1,9% versus 9,1%; p=0,033). Observou-se uma tendência global para um maior atraso nos tempos-chave de abordagem de doentes com STEMI. A taxa de mortalidade destes doentes no P1 foi superior comparativamente a anos prévios (1,9% versus 12,1%; p=0,005).
ConclusõesDurante a primeira onda da pandemia Covid-19 houve uma redução do número de doentes submetidos a angioplastia coronária por STEMI. Esses apresentaram mais complicações mecânicas e uma maior mortalidade.
In December 2019, a novel pathogenic viral agent named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was discovered in the city of Wuhan, China. The disease was later called Covid-19,1 and subsequent events led the World Health Organization to declare the SARS-CoV-2 outbreak a pandemic. As a precautionary measure, many hospitals postponed elective procedures, and containment measures were adopted by almost every country in the world in an attempt to slow progression of the pandemic. In Portugal, a national state of emergency was declared on March 18 2020 with implementation of strict stay-at-home measures to stop the spread of the disease.2 In early May, these measures were gradually lifted as the rate at which new individuals were being infected by SARS-CoV-2 was slowly decreasing. However, as the number of Covid-19 cases increased worldwide, there has been a general belief that admissions to the emergency room (ER) for non-Covid-related causes, especially cardiovascular diseases, have fallen. A possible explanation for this phenomenon would be fear of seeking medical attention in hospitals and becoming infected with SARS-CoV-2, as well as a medical focus on Covid-related symptoms.
ST-elevation myocardial infarction (STEMI) is frequent in the ER, with an annual incidence ranging from 44 to 142/100 000 population/year in Europe and estimated to be 104/100 000 population/year in Portugal.3,4 The Portuguese national registry reports the incidence of primary percutaneous coronary intervention (PCI) as 316 per million population in 2015.5,6 Several observational studies appear to confirm that the Covid-19 pandemic has been followed by a reduction in the number of STEMI patients admitted to the ER. Italy, one of the first affected European countries, reported a 26.5% reduction in STEMI admissions in a one-week period during the Covid-19 pandemic in comparison with the same week in the previous year.7 Another report, from northern Italy, appears to support these findings.8 In Spain a 40% reduction was observed, with some regions reporting reductions as high as 85%.9 Observational studies in the USA report similar data.10–12 Furthermore, there are reports of increased delays not only in time from symptom onset to first medical contact (FMC), but also in time from door to device and from catheterization laboratory arrival to device.13,14 An increase of 13.7% in STEMI-related mortality was also found in Italy.7
We sought to assess the impact of the Covid-19 pandemic on STEMI admissions in Portugal, specifically in the profile of patients admitted, specific key time components in STEMI care bundles, and associated in-hospital outcomes.
MethodsPatient selectionWe performed a multicenter retrospective analysis of consecutive STEMI patients presenting in the ER of two hospital centers, one with on-site ER (HospA) and another tertiary center without on-site ER (HospB). Both are coordinating hubs within the local STEMI network with cardiac catheterization facilities for PCI. HospA, due to its geographical characteristics, also receives STEMI patients from other spoke centers who undergo fibrinolysis before going to the catheterization laboratory. HospB mainly receives STEMI patients who undergo primary PCI, referred from local emergency medical systems or from non-PCI spoke centers.
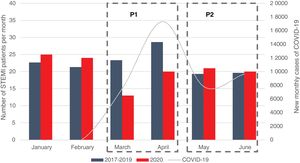
Two sequential time periods were prospectively defined: P1 from March 1 to April 30 and P2 from May 1 to June 30 (Figure 1). The equivalent periods in 2017-2019 were considered the non-Covid-19 period and were compared with the corresponding period in 2020, the Covid-19 period. All patients admitted directly to the catheterization laboratory or who underwent fibrinolysis due to STEMI were included. STEMI was defined according to the Fourth Universal Definition of Myocardial Infarction.15 Non-ST-elevation myocardial infarction patients were excluded. Patients were identified through institutional dedicated database software (CardioBase®), used in both centers.
Data collectionData on the number of patients admitted to each hospital for STEMI were recorded, and the number of people infected with Covid-19 during the study period of 2020 was obtained through national registries available on the national health authority's website.16–19 Data on demographic characteristics, comorbidities and mode of presentation were collected for each STEMI patient. A high cardiovascular risk patient was defined as having at least one of the following: smoking history, previous PCI, previous myocardial infarction or diabetes, plus one cardiovascular risk factor. Key timings for STEMI care, namely pain to FMC, door to needle (DTN), door to wire (DTW) and symptoms to wire (STW), and in-hospital outcomes regarding mortality, length of hospital stay, Killip class, in-hospital heart failure, mechanical complications, mechanical ventilation, major bleeding (defined as Bleeding Academic Research Consortium [BARC]20 grade 3-5) and additional PCI for non-culprit lesions were also retrieved.
Data were obtained from each center's institutional records and from catheterization laboratory records.
Statistical analysisContinuous variables are presented as mean and standard deviation (SD) or median and interquartile range (IQR) as appropriate and compared by the Student's t test if the distribution was normal or the Mann-Whitney test for non-normal distributions. Categorical variables are presented as absolute numbers and percentages and compared using the chi-square test. The p-value for statistical significance was defined as <0.05. All comparisons were made between 2020 and 2017-2019 for both time periods. Analyses were carried using IBM SPSS Statistics version 23.
ResultsA total of 347 consecutive STEMI patients were included in the study. The main results are shown in Figure 1.
During P1 2020 there was a lower absolute number of STEMI cases compared with previous years (monthly STEMI rate of 26.0±4.2 vs. 16.5±4.9 cases, representing a 36.5% reduction; 95% confidence interval 12.1-61.0; p=0.033) (Table 1), a higher incidence of mechanical complications (0.0% vs. 3.0%; p=0.029), and a six-fold higher mortality rate (1.9% vs. 12.1%; p=0.005).
Admissions for ST-elevation myocardial infarction during the two study periods.
| P1 (March-April) | P2 (May-June) | |||||
|---|---|---|---|---|---|---|
| 2017-2019 | 2020 | p | 2017-2019 | 2020 | p | |
| Total number of admissions | 156 | 33 | - | 117 | 41 | - |
| STEMI cases per month (mean ± SD) | 26.0±4.2 | 16.5±4.9 | 0.033 | 19.5±0.7 | 20.5±0.7 | 0.500 |
SD: standard deviation; STEMI: ST-elevation myocardial infarction.
Conversely, during P2, when the number of new monthly reported Covid-19 cases started to decrease, the absolute number of new STEMI cases increased again (monthly STEMI rate of 19.5±0.7 vs. 20.5±0.7), resembling the same behavior in early 2020 (January and February) and previous years.
Patients admitted for STEMI in the Covid-19 year and non-Covid-19 years did not differ in demographic characteristics, except that those in P1 2020 were younger than those presenting in previous years (62.6±12.8 vs. 57.8±12.1 years; p=0.037). Risk factors for cardiovascular disease were similar between 2020 and previous years in both time periods (Table 2).
Patient characteristics.
| P1 (March-April) | P2 (May-June) | |||||
|---|---|---|---|---|---|---|
| 2017-2019 | 2020 | p | 2017-2019 | 2020 | p | |
| Age, years, mean±SD | 59.5±12.7 | 60.6±15.8 | 0.681 | 62.6±12.8 | 57.8±12.1 | 0.037 |
| Male, n (%) | 113 (72.4) | 24 (72.7) | 0.973 | 91 (77.8) | 32 (78.0) | 0.971 |
| High-risk patients, n (%) | 114 (73.1) | 25 (75.8) | 0.696 | 80 (68.4) | 30 (73.2) | 0.566 |
| Diabetes, n (%) | 35 (22.4) | 5 (15.2) | 0.352 | 24 (20.5) | 9 (22.0) | 0.845 |
| Smoking history, n (%) | 90 (57.7) | 20 (60.6) | 0.758 | 65 (55.6) | 26 (63.4) | 0.381 |
| Hypertension, n (%) | 91 (58.3) | 14 (42.4) | 0.095 | 62 (53.0) | 23 (56.1) | 0.731 |
| Dyslipidemia, n (%) | 64 (41.0) | 17 (51.5) | 0.269 | 41 (35.0) | 12 (29.3) | 0.500 |
| Previous MI, n (%) | 16 (10.3) | 5 (15.2) | 0.416 | 7 (6.0) | 2 (4.9) | 0.793 |
| Previous PCI, n (%) | 20 (12.8) | 6 (18.2) | 0.417 | 8 (6.8) | 2 (4.9) | 0.657 |
| CAD family history, n (%) | 13 (8.3) | 2 (6.1) | 0.661 | 9 (7.7) | 2 (4.9) | 0.542 |
CAD: coronary artery disease; MI: myocardial infarction; PCI: percutaneous coronary intervention; SD: standard deviation.
Patients were mainly referred from spoke centers, and this did not change significantly from non-Covid-19 years to the Covid-19 year, regardless of the period considered. More serious forms of STEMI presentation, particularly out-of-hospital cardiac arrest (OHCA) and cardiogenic shock, occurred similarly across periods, with no statistically significant differences (Table 3).
Characteristics of patient presentation.
| P1 (March-April) | P2 (May-June) | |||||
|---|---|---|---|---|---|---|
| 2017-2019 | 2020 | p | 2017-2019 | 2020 | p | |
| Access to the hospital, n (%) | ||||||
| Ambulance | 28 (17.9) | 5 (15.2) | 0.701 | 32 (27.4) | 8 (19.5) | 0.321 |
| Spoke | 105 (67.3) | 24 (72.7) | 0.543 | 67 (57.3) | 27 (65.9) | 0.335 |
| Hub | 23 (14.7) | 4 (12.1) | 0.696 | 18 (15.4) | 6 (14.6) | 0.908 |
| OHCA, n (%) | 6 (3.8) | 2 (6.1) | 0.566 | 12 (10.3) | 4 (9.8) | 0.927 |
| Cardiogenic shock, n (%) | 10 (6.4) | 2 (6.1) | 0.940 | 13 (11.1) | 3 (7.3) | 0.488 |
| Thrombolysis, n (%) | 21 (13.5) | 6 (18.2) | 0.481 | 18 (15.4) | 7 (17.1) | 0.799 |
| Rescue PCI after failed thrombolysis, n (%) | 3 (1.9) | 3 (9.1) | 0.033 | 3 (2.6) | 1 (2.4) | 0.965 |
| Periprocedural P2Y12therapy, n (%) | ||||||
| Clopidogrel | 30 (19.2) | 8 (25.0) | 0.514 | 21 (18.1) | 8 (19.5) | 0.824 |
| Ticagrelor | 126 (80.8) | 23 (71.9) | 0.157 | 95 (81.9) | 33 (80.5) | 0.921 |
| Radial access, n (%) | 139 (89.1) | 28 (84.8) | 0.489 | 105 (89.7) | 38 (92.7) | 0.581 |
| Diseased vessels, mean ± SD | 1.47±0.69 | 1.58±0.71 | 0.443 | 1.39±0.62 | 1.49±0.60 | 0.257 |
Ambulance: patients who accessed the hospital after calling the national emergency system and were diagnosed in an out-of-hospital setting; Hub: patients who accessed a PCI hospital center directly; OHCA: out-of-hospital cardiac arrest; PCI: percutaneous coronary intervention; SD: standard deviation; Spoke: patients who first accessed a non-PCI hospital center.
Rescue PCI after failed thrombolysis occurred more frequently during P1 2020 than in previous years (1.9% vs. 9.1%; p=0.033), although no differences were found in the number of patients who underwent fibrinolysis as reperfusion therapy. Most patients were given ticagrelor as a periprocedural P2Y12 inhibitor, and radial access for PCI was the most common arterial access used.
We observed longer overall delays in all STEMI time components, as shown in Table 4. There was a trend for longer delays in seeking medical assistance in 2020, particularly in P1, as reflected by the interquartile range of the FMC time component (120.0 [50.0-196.0] vs. 120.0 [60.8-270.8] min, p=0.481). DTN time for patients who underwent fibrinolysis followed the same trend, with longer delays for the administration of the fibrinolytic agent during P1 2020 compared with previous years (27.0 [13.8-48.8] vs. 82.5 [27.5-150.0] min, p=0.056). Regarding DTW time, there were longer delays in HospB during P2 2020 than in previous years (28.0 [21.5-34.0] vs. 33.0 [25.0-57.0] min; p=0.03). The change in STW time during P1 was not statistically different for the entire cohort (240.0 [158.3-377.8] min in previous years vs. 244 [165.0-621.5] min in 2020; p=0.342). However, in the HospA cohort, STW time increased during P1 2020 (218.0 [176.8-524.3] vs. 652.0 [432.0-962.0] min; p=0.031). Importantly, and in contrast to what was observed for FMC during the second period, there was also a significant increase in STW time during P2 2020 for the entire cohort (228.0 [152.0-328.5] vs. 250.0 [204.5-441.0] min; p=0.047) (Supplementary Tables 7 and 8).
Key timings of ST-elevation myocardial infarction care.
| P1 (March-April) | P2 (May-June) | |||||
|---|---|---|---|---|---|---|
| 2017-2019 | 2020 | p | 2017-2019 | 2020 | p | |
| STEMI timings, min, median (IQR) | ||||||
| FMC | 120.0 (50.0-196.0) | 120.0 (60.8-270.8) | 0.481 | 106.5 (60.0-210.0) | 120.0 (60.0-215.0) | 0.479 |
| DTN | 27.0 (13.8-48.8) | 82.5 (27.5-150.0) | 0.056 | 32.5 (26.3-46.5) | 30.0 (28.0-105.0) | 0.946 |
| DTW | 34.0 (23.8-86.3) | 37.0 (29.0-50.0) | 0.679 | 33.0 (25.0-57.0) | 41.0 (28.3-68.3) | 0.167 |
| STW | 240.0 (158.3-377.8) | 244.0 (165.0-621.5) | 0.342 | 228.0 (152.0-328.5) | 250.0 (204.5-441.0) | 0.047 |
DTN: door to needle; DTW: door to wire; FMC: pain to first medical contact; IQR: interquartile range; STEMI: ST-elevation myocardial infarction; STW: symptoms to wire.
The difference in the number of diseased vessels detected on coronary angiography was not statistically significant between the previous years and 2020 in either time period (1.47±0.69 vs. 1.58±0.71 in P1 and 1.39±0.62 vs. 1.49±0.60 in P2; p=0.443 and p=0.257, respectively) (Table 3). Despite this, in-hospital outcomes (Table 5) showed six-fold higher mortality during P1 2020 (1.9% vs. 12.1%; p=0.005). This did not occur during P2. As previously stated, the increase in mortality during P1 was associated with more mechanical complications secondary to STEMI (0.0% vs. 3.0%; p=0.029) and a trend toward more BARC grade 3-5 bleeding events (3.2% vs. 9.1%; p=0.132). During P2 2020 there were no significant differences from previous years in in-hospital outcomes. Hospital length of stay was statistically stable in both P1 (7.1±8.7 vs. 6.6±6.9; p=0.152) and P2 (7.4±8.9 vs. 6.4±6.5; p=0.882). None of the patients hospitalized during 2020 had SARS-CoV-2 infection after testing with nasopharyngeal swab.
In-hospital outcomes.
| P1 (March-April) | P2 (May-June) | |||||
|---|---|---|---|---|---|---|
| 2017-2019 | 2020 | p | 2017-2019 | 2020 | p | |
| Killip class, n (%) | ||||||
| III | 5 (3.2) | 1 (3.0) | 0.958 | 1 (0.9) | 3 (7.3) | 0.023 |
| IV | 10 (6.4) | 3 (9.1) | 0.580 | 13 (11.1) | 3 (7.3) | 0.488 |
| BARC 3-5 bleeding, n (%) | 5 (3.2) | 3 (9.1) | 0.132 | 6 (5.1) | 2 (4.9) | 0.950 |
| Heart failure, n (%) | 28 (18.2) | 5 (15.2) | 0.679 | 17 (14.5) | 7 (17.1) | 0.696 |
| Mechanical ventilation, n (%) | 10 (6.5) | 3 (9.1) | 0.594 | 12 (10.3) | 3 (7.3) | 0.581 |
| Mechanical complication, n (%) | 0 (0.0) | 1 (3.0) | 0.029 | 1 (0.9) | 0 (0.0) | 0.553 |
| Additional PCI, n (%) | ||||||
| Intraprocedure | 12 (7.7) | 3 (9.7) | 0.787 | 11 (9.4) | 2 (4.9) | 0.364 |
| Staged | 9 (5.8) | 1 (3.2) | 0.523 | 6 (5.1) | 6 (14.6) | 0.048 |
| Length of stay, days, mean ± SD | 7.1±8.7 | 6.6±6.9 | 0.152 | 7.4±8.9 | 6.4±6.5 | 0.882 |
| Mortality | 3 (1.9) | 4 (12.1) | 0.005 | 5 (4.3) | 0 (0.0) | 0.179 |
BARC: Bleeding Academic Research Consortium grade; PCI: percutaneous coronary intervention; SD: standard deviation.
Our findings are new in that they describe a significant decrease in the absolute number of STEMI cases and increases in the number of STEMI mechanical complications and of failed thrombolysis and, importantly, a mortality impact. The peak incidence of Covid-19 cases in Portugal was accompanied by a reduction in new STEMI patients presenting to hospitals in the acute phase, in line with previous reports from other countries. As new infections began to decrease, the number of new monthly STEMI cases resumed, as compared with previous years. The explanation for this behavior could be related to the strict measures deployed by national authorities and people's fear of becoming infected. Also, after perception of a reduction in all-cause ER episodes during the peak of the pandemic,21 health authorities started public campaigns to encourage patients with symptoms of myocardial infarction and stroke to seek medical attention.22–24 This could explain the increase in STEMI patients during the second period, even during the pandemic.
Patient demographics were roughly similar between the two time periods, the only exception being that patients were younger during P2 2020 than in previous years. This particular finding could be related to greater reluctance of older people to leave their homes or their care centers, as the higher mortality from Covid-19 in this population was soon identified and was extensively covered in the media.25
Most of the patients were referred from spoke centers without catheterization facilities, which was similar to previous years. Although the number of patients undergoing thrombolysis at presentation did not differ from previous years, the number of patients requiring rescue PCI after failed thrombolysis rose significantly. This could be related to the observed trend for longer FMC and DTN times, which are known to reduce the efficacy of this treatment.26 Patient presentation was very similar in both 2020 periods compared to previous years.
The Covid-19 pandemic necessitated a profound and wide-ranging reorganization of emergency departments involving human resources, local protocols and circuits to prevent the spread of the infection and to secure health facilities. Many healthcare workers were assigned different tasks unrelated to their daily practice or specialized training to compensate for the shortage of human resources. These changes, although deemed necessary, may have jeopardized care for non-Covid-19 related situations. In our cohort we observed a trend for longer delays in some key timings of STEMI care.13,27 This raises the concern that, although some degree of delay was related to the patients themselves, the efficiency of the healthcare system was probably also affected. As stated above, most patients were referred from non-PCI centers, and this system delay could be related to the logistics of transfer to a PCI center. Due to the protection measures adopted, all patients were managed as if infected with SARS-CoV-2 until proven otherwise. Healthcare professionals spent additional time putting on personal protective equipment in order to handle these patients in pre-hospital settings and to perform invasive coronary angiography. It is also important to consider the lack of appropriate transportation to PCI centers with dedicated rooms for suspected or positive Covid-19 cases. Also, the catheterization facilities dedicated to Covid-19 patients might not have had all the required devices readily available. Although the operator may anticipate what will be required based on the patient's clinical data, STEMI location and personal experience, if the procedure itself reveals complexity and requires devices other than those available inside the room, this will prolong time until lesion wire crossing and hence total ischemia time.
We found no significant difference in the severity of coronary artery disease in these patients. However, mortality was significant higher during the first 2020 period. This could be related to the above-mentioned findings, as well as to the observation of more frequent mechanical complications. The number of patients included in this study may have been too small to detect other in-hospital outcomes that could explain the rise in mortality in this period.
The present study covers the acute management of the whole spectrum of STEMI patients during the Covid-19 pandemic. The data collected include patients who accessed hub centers directly or after referral from ambulance or spoke centers, as well as patients who, due to transfer logistics, benefited from undergoing thrombolysis before PCI. It is possible that, as the pandemic continued, more patients who refused to seek medical attention during the acute phase of STEMI presented later in the ER in severe ischemic heart failure. With uncertainty surrounding future outbreaks, these findings may help us to prepare ERs and optimize local circuits and protocols in order to improve the prognosis of these patients.
Study limitationsThis is a retrospective study that specifically assessed STEMI patients admitted directly for PCI or fibrinolysis. This form of selection may have introduced selection bias, so the results presented should be interpreted with caution. It would also be interesting to analyze the number of patients in these periods presenting late with STEMI, to have a wider picture of what really happened to these patients during the pandemic. Regarding STEMI time components, information about time from FMC to electrocardiogram was not obtained, which could have provided more answers regarding system delay. Another limitation of this study comes from the fact that many of the included patients referred from spoke centers were transferred back for continuation of care after primary PCI. This resulted in failure to retrieve in-hospital data for every patient regarding pharmacology therapy with prognostic impact on STEMI, such as angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, statins and beta-blockers. However, based on the available data, we found no significant difference for the rate of in-hospital prescription of these drugs. Also, mortality due to STEMI could have been better addressed if we had access to autopsies during these periods to see if there was an increase of initial unexplained deaths that were subsequently found to be due to myocardial infarction. More data are needed to identify factors that are associated with the observed increase in mortality of STEMI patients during the peak of the pandemic.
ConclusionsFindings in this study confirm that fewer STEMI patients were admitted in the acute phase during the first peak of the Covid-19 pandemic in Portugal. Also, these patients had higher mortality during this period, which could be related to delays in key timings for STEMI care and increased mechanical complications. Further research is needed to establish the reasons for this apparent increase in mortality, in order to prepare an appropriate response for these patients in the event of future outbreaks.
Conflicts of interestThe authors have no conflicts of interest to declare.