Reperfusion and revascularization therapies play an important role in the management of coronary heart disease and have contributed to decreases in case fatality rates. We aimed to describe the use of these therapies for the treatment of acute coronary syndrome (ACS) patients over time in Portugal.
MethodsPubMed was searched in July 2012. The proportion of patients treated with fibrinolysis, primary percutaneous coronary intervention (PCI), any PCI and coronary artery bypass grafting (CABG) was described according to type of ACS: STEMI (≥90% patients with ST-segment elevation or Q-wave myocardial infarction), NSTE-ACS (≥90% patients with non-ST-segment elevation ACS) and mixed ACS (all others).
ResultsWe identified 41 eligible studies, published between 1989 and 2011. Twenty-eight reported on samples considered representative of ACS patients treated in Portugal. The small number of estimates of the use of each treatment in STEMI and NSTE-ACS patients precluded identification of any time trend. In the last 20 years, the proportion of mixed ACS patients treated with fibrinolysis decreased and the use of PCI increased, while the use of CABG did not change.
ConclusionsThe general pattern of the use of reperfusion and revascularization is in accordance with that reported in other developed countries, reflecting a favorable trend in the quality of care of ACS patients. The relatively small number of estimates on the same procedure in comparable patients limits the generalizability of the conclusions, and highlights the need for systematic approaches to monitor the use of treatments over time.
A reperfusão e revascularização desempenham um importante papel no tratamento da doença coronária contribuindo para a diminuição da letalidade. Foi nosso objetivo descrever o uso destes procedimentos no tratamento da síndrome coronária aguda (SCA) ao longo do tempo em Portugal.
MétodosA pesquisa foi efetuada na Pubmed em julho de 2012. A proporção de doentes tratados com fibrinólise, angioplastia primária, qualquer tipo de angioplastia e cirurgia de revascularização coronária (CABG) foi descrita de acordo com o tipo de SCA: SCA supra-ST (quando a proporção de doentes com elevação do segmento ST ou enfarte do miocárdio com ondas Q era ≥90%), SCA sem-ST (quando a proporção de doentes com SCA sem elevação do segmento ST era ≥90%) e SCA misto (restantes casos).
ResultadosForam identificados 41 estudos publicados entre 1989 e 2011. Vinte e oito estudos descreveram amostras representativas dos doentes com SCA tratados em Portugal. O baixo número de estimativas de cada tratamento nos doentes com SCA supra-ST e sem-ST, impossibilitou a observação de tendências temporais. Nos últimos 20 anos, a proporção de doentes com SCA misto tratados com fibrinólise diminuiu, o uso de angioplastia aumentou, enquanto o uso de CABG não se alterou.
ConclusõesO padrão do uso destes tratamentos está de acordo com dados publicados noutros países desenvolvidos, refletindo uma tendência favorável na qualidade dos cuidados prestados. O baixo número de estimativas do mesmo procedimento limitou a generalização de conclusões, reforçando a necessidade de alternativas para monitorizar o uso de tratamentos ao longo do tempo.
Coronary heart disease (CHD) is responsible for 7.3 million deaths yearly worldwide, corresponding to 12.8% of all deaths.1 In Portugal, CHD was responsible for 23% of cardiovascular deaths in 2009,2 though mortality rates have been decreasing since the 1980s, as in most developed countries.3
The increasing use of evidence-based treatments for acute coronary syndrome (ACS), including reperfusion therapy and revascularization procedures, has been reported to explain up to half of the decrease in CHD mortality rates in several developed countries.4,5 Continuous and comprehensive monitoring of the use of reperfusion and revascularization therapies for ACS patients in routine clinical practice is thus essential to evaluate the quality of care.
The Portuguese Registry of Acute Coronary Syndromes provides data on a large number of ACS events in the last decade, but only patients admitted to some cardiology departments in the country are registered and consecutive recruitment is not ensured, possibly limiting its representativeness.6 Other studies, based on samples of episodes, mainly single-center and resulting from the initiative of local physicians or academic researchers, have been published and could complement the registry data with coverage of other institutions and departments and a greater time span.
Therefore, we performed a systematic review of published studies reporting on the use of reperfusion and revascularization procedures in patients with ACS in Portugal.
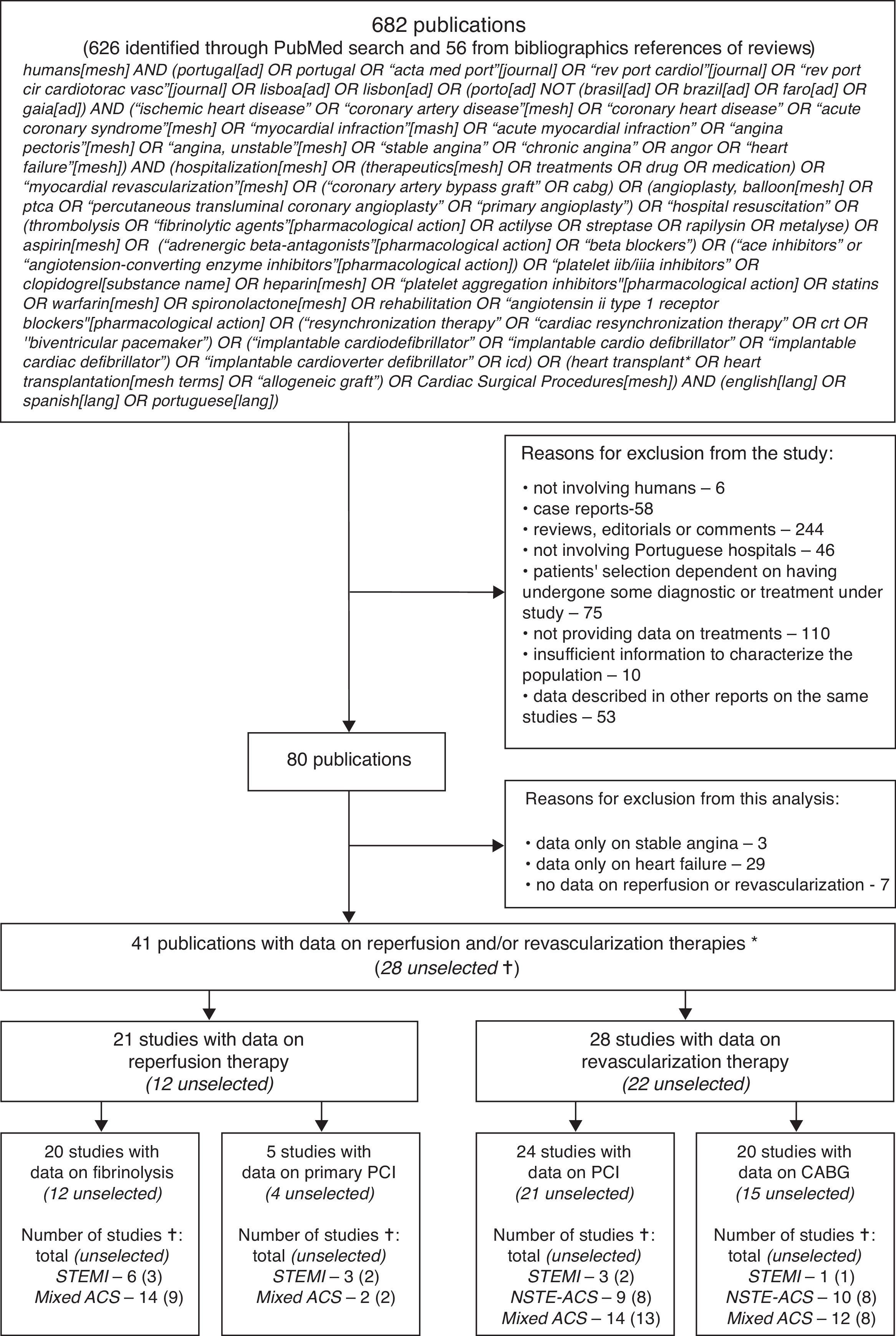
MethodsSearch strategyWe searched PubMed from inception until July 2012 to identify original reports providing data on the proportion of patients with ACS, stable angina and heart failure treated with pharmacological and non-pharmacological therapies in Portugal. The search expression is provided in the systematic review flowchart (Figure 1). This report focuses on reperfusion and revascularization procedures in ACS. The reference lists of review articles on treatment of ACS patients were screened to identify other potentially eligible original studies.
Flowchart of the systematic review. CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention; STEMI: 90% or more patients with diagnosis of ST-segment elevation myocardial infarction or Q-wave myocardial infarction; NSTE-ACS: 90% or more patients with diagnosis of non-ST-segment elevation ACS; mixed ACS: mixture of patients with several types of ACS.
* If a study provided data on treatment with both reperfusion and revascularization, it contributed to both groups. If a study provided data on more than one diagnostic category, it contributed to all groups.
† The sample was considered selected when inclusion of patients was dependent on having undergone some diagnosis or treatment procedure; otherwise, it was considered unselected.
Two reviewers independently assessed the studies in two steps, following the same predefined criteria, to determine the eligibility of each report. In the first step irrelevant studies were excluded on the basis of the title and abstract only; when the abstract of a particular article was not available, the article was selected for further assessment, except when the title unequivocally presented evidence for exclusion (e.g. case report). The full texts of studies selected for the second step were then assessed to decide on their eligibility and availability of relevant data.
The decisions made independently by the two reviewers were compared in the two phases and disagreements were resolved by consensus or after discussion with a third researcher, if necessary.
The criteria for exclusion of studies were the following: not involving humans (e.g. in-vitro studies; animal research); case reports; reviews, editorials or comments; not involving Portuguese hospitals; involving ACS patients whose selection was dependent on having undergone a particular diagnosis or treatment procedure under study and with no information on any other procedure (e.g. samples including only patients who underwent PCI); not providing data on treatments in ACS patients; providing insufficient information to characterize the population (e.g. not providing information on patients’ age or sex, or sample size).
When more than one study provided data on patients with the same diagnosis, selected using the same criteria, from the same institution and in overlapping periods, we included the one that covered the longest time period; if the same time period was considered, the one with the largest sample size was included, or in cases of similar sample size, the one that provided information on more eligible treatments. When there were two studies that included ACS patients admitted to the same hospital with part of the data collection period overlapping, we included only the one with the larger sample size, even though over a shorter time period,7 since the other included a group selected from all patients with ACS.8 When two publications studied the same sample, but reported complementary results on eligible treatments, both articles were included but the information on each eligible treatment for each specific diagnosis was considered only once in the data analyses.
Data extractionPapers were scrutinized using a standardized data extraction sheet, to collect information on: first author, publication year, year or period of data collection, geographical coverage and department where patients were recruited, sample characteristics (study population, diagnosis, type of episode [first vs. recurrent], sex, age and sample size), proportion of patients who received treatments (fibrinolysis, primary and non-specified PCI and coronary artery bypass grafting [CABG]). If only the absolute number of patients treated was available, the proportion was calculated by dividing by the stratum-specific sample size. When an article presented data stratified by a variable with no relevance to our analysis (e.g. diabetic vs. non-diabetic patients), we calculated the weighted average of the proportions over all strata.
All types of PCI (including primary PCI) were considered in the analysis of this procedure as revascularization therapy. The proportions of patients undergoing percutaneous and surgical revascularization procedures were described only when performed during the initial hospitalization for the acute event. We considered two types of study population in terms of their representativeness of ACS patients treated in Portuguese institutions: when patient selection was dependent on having undergone a treatment or a diagnostic procedure (e.g. patients referred for viability tests; patients undergoing coronary angiography), the population was considered selected; otherwise, it was considered unselected.
When possible, year-, sex-, age- and diagnosis-specific estimates were extracted.
Data analysisAll studies are described in the Supplementary Table available online; only those relying on unselected samples of patients are represented in the forest plots. Although sex- and age-specific estimates were extracted and are shown in the detailed Supplementary Table, these were seldom available and for descriptive purposes the results for the total sample are always presented in the forest plots, stratified only by diagnosis.
The proportion of patients who underwent each procedure was described according to type of ACS. However, given that reports did not systematically stratify according to this criterion, patient samples were classified into one of the following three categories, according to the proportion of different ACS patients included: STEMI (90% or more patients with a diagnosis of ST-segment elevation myocardial infarction (STEMI) or Q-wave myocardial infarction [MI]), NSTE-ACS (90% or more patients with a diagnosis of non-ST-segment elevation ACS [NSTE-ACS]), and mixed ACS (if neither of these criteria was satisfied).
ResultsWe identified 41 eligible studies providing data on ACS patients who underwent reperfusion and/or revascularization therapies, 21 presenting data on reperfusion and 28 on revascularization (Figure 1), published between 1989 and 2011 (Supplementary Table 1, available online).
Over three-quarters of the studies reported data from a single institution, mainly from the Lisbon region. Three studies were based on national registries that covered several regions of the country.6,9,10 The vast majority of studies recruited patients in cardiology departments. Two-thirds of the studies included unselected populations. More than half of the studies included both first and recurrent episodes and four studies reported exclusively on first episodes.11–14 The sample size ranged from 21 to 22482 patients, and almost 40% of the studies involved samples between 100 and 500 patients. Seven samples included mostly STEMI patients, 10 mostly NSTE-ACS patients and 27 a mixture of patients with several types of ACS. Five studies presented sex-specific estimates,10,14–17 and only two presented age-specific estimates18,19 (Supplementary Table 1, available online).
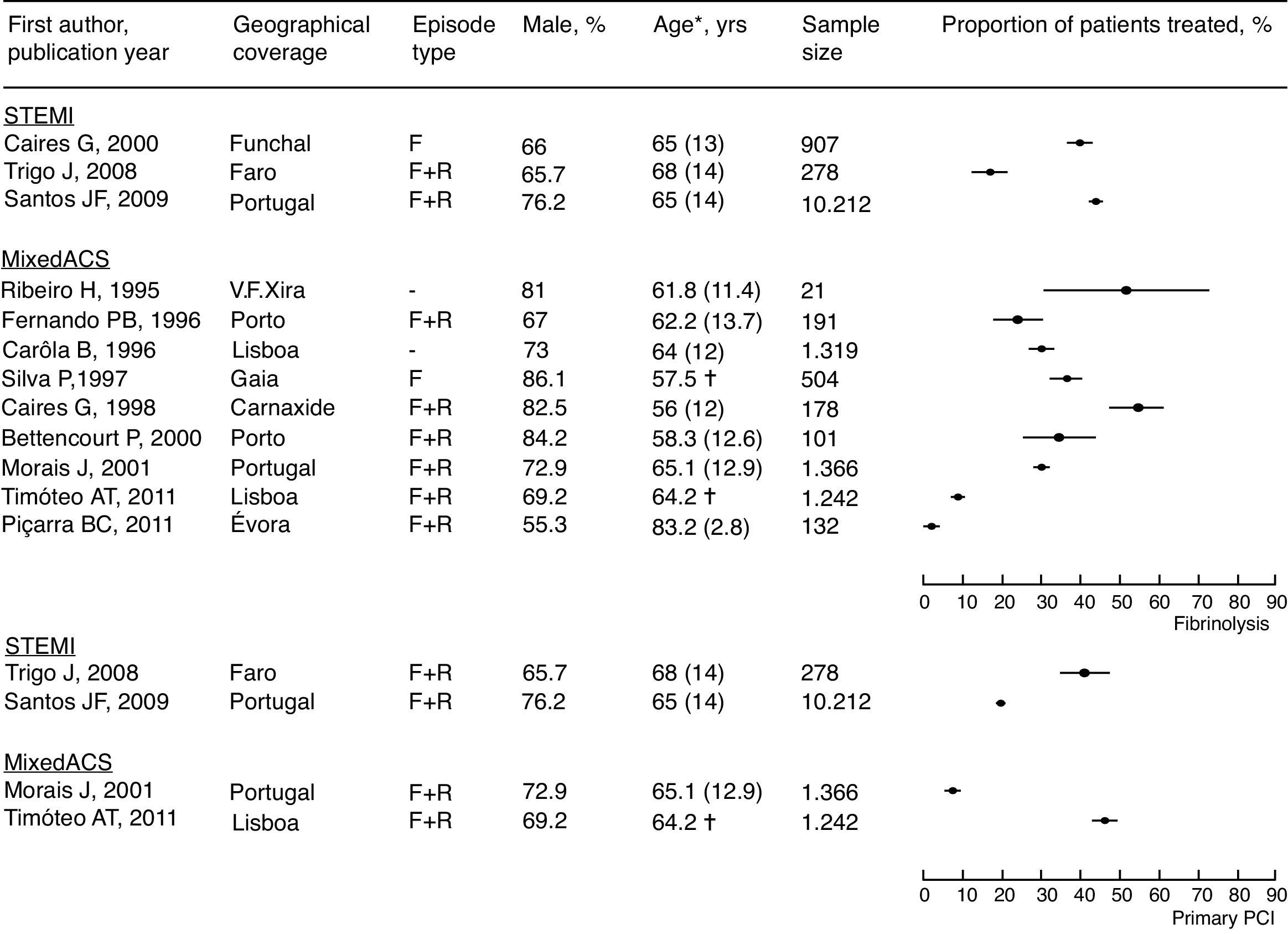
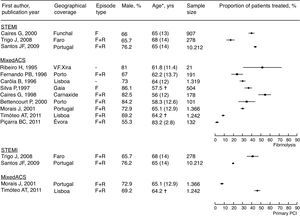
As expected, data on reperfusion were available only for STEMI and mixed ACS patients (Figure 1). Only three studies provided estimates of the use of reperfusion in STEMI patients. In more recent years, one study conducted in Faro reported the use of fibrinolysis in 16.5% of STEMI patients in 2008,20 while a report from the National Registry of Acute Coronary Syndromes showed a mean of 43.7%, representing many cardiology centers across the country over several years.6 The same two studies reported the use of primary PCI in 41.4% and 19.2% of STEMI patients, respectively.6,20 For mixed ACS patients there was a larger number of observations; fibrinolysis was used in a quarter to a half of patients in the late 1990s, decreasing to less than 10% over the next decade. Two reports published 10 years apart, in 2001 and 2011, showed an increase in the use of primary PCI in mixed ACS patients, from less than 10% in a sample of patients from several cardiology centers across the country10 to approximately 50% in a single cardiology center in Lisbon19 (Figure 2).
Proportion of acute coronary syndrome patients treated with reperfusion therapies (fibrinolysis and primary PCI) in Portugal, estimated in unselected samples of patients. F: first episode; mixed ACS: mixture of patients with several types of ACS; NSTE-ACS: 90% or more patients with diagnosis of non-ST-segment elevation ACS; PCI: percutaneous coronary intervention; R: recurrent episode; STEMI: 90% or more patients with diagnosis of ST-segment elevation myocardial infarction or Q-wave myocardial infarction. * Age is presented as mean (SD) unless otherwise specified; † mean age; ‡ median age.
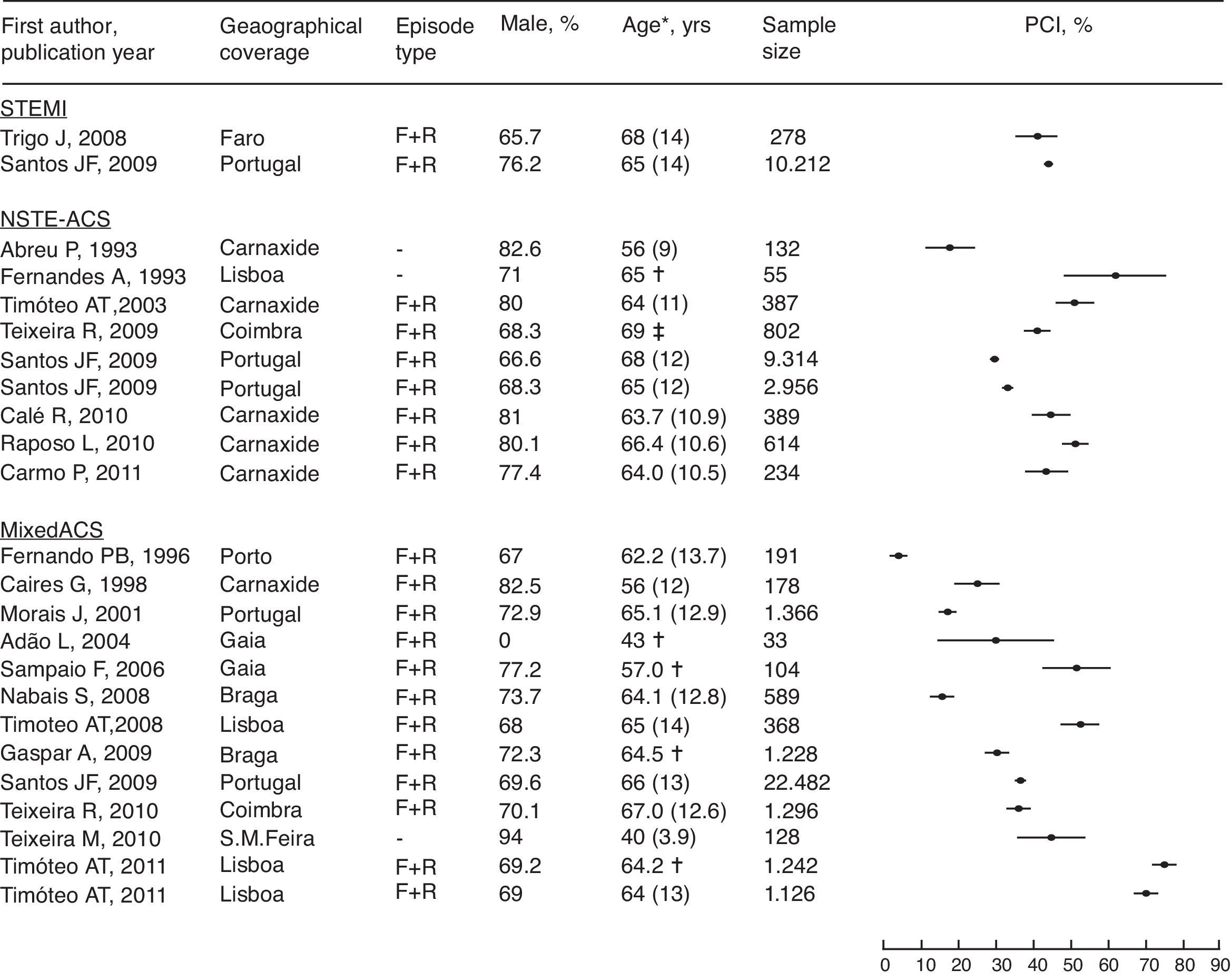
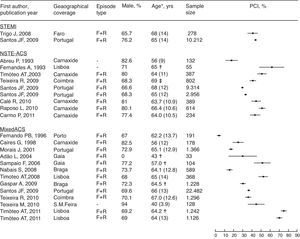
Percutaneous revascularization, including both emergent and elective procedures during hospitalization for an acute event, was performed in approximately half of STEMI patients according to a report from Faro in 200820 and the report of the National Registry of Acute Coronary Syndromes covering several years and centers across the country.6 For NTSE-ACS, two studies published in 1993 report contrasting experiences in small single-center samples, while from 2003 to 2011 several estimates consistently point to one third to one half of patients being revascularized percutaneously during the acute hospitalization, with no clear time trend. With a larger number of reports and more regular publication over 15 years, the proportion of mixed ACS patients revascularized percutaneously increased from under 10% in the mid-1990s to approximately 70% in recent years (Figure 3).
Proportion of acute coronary syndrome patients treated with PCI in Portugal, estimated in unselected samples of patients. F: first episode; mixed ACS: mixture of patients with several types of ACS; NSTE-ACS: 90% or more patients with diagnosis of non-ST-segment elevation ACS; PCI: percutaneous coronary intervention; R: recurrent episode; STEMI: 90% or more patients with diagnosis of ST-segment elevation myocardial infarction or Q-wave myocardial infarction. * Age is presented as mean (SD) unless otherwise specified; † mean age; ‡ median age.
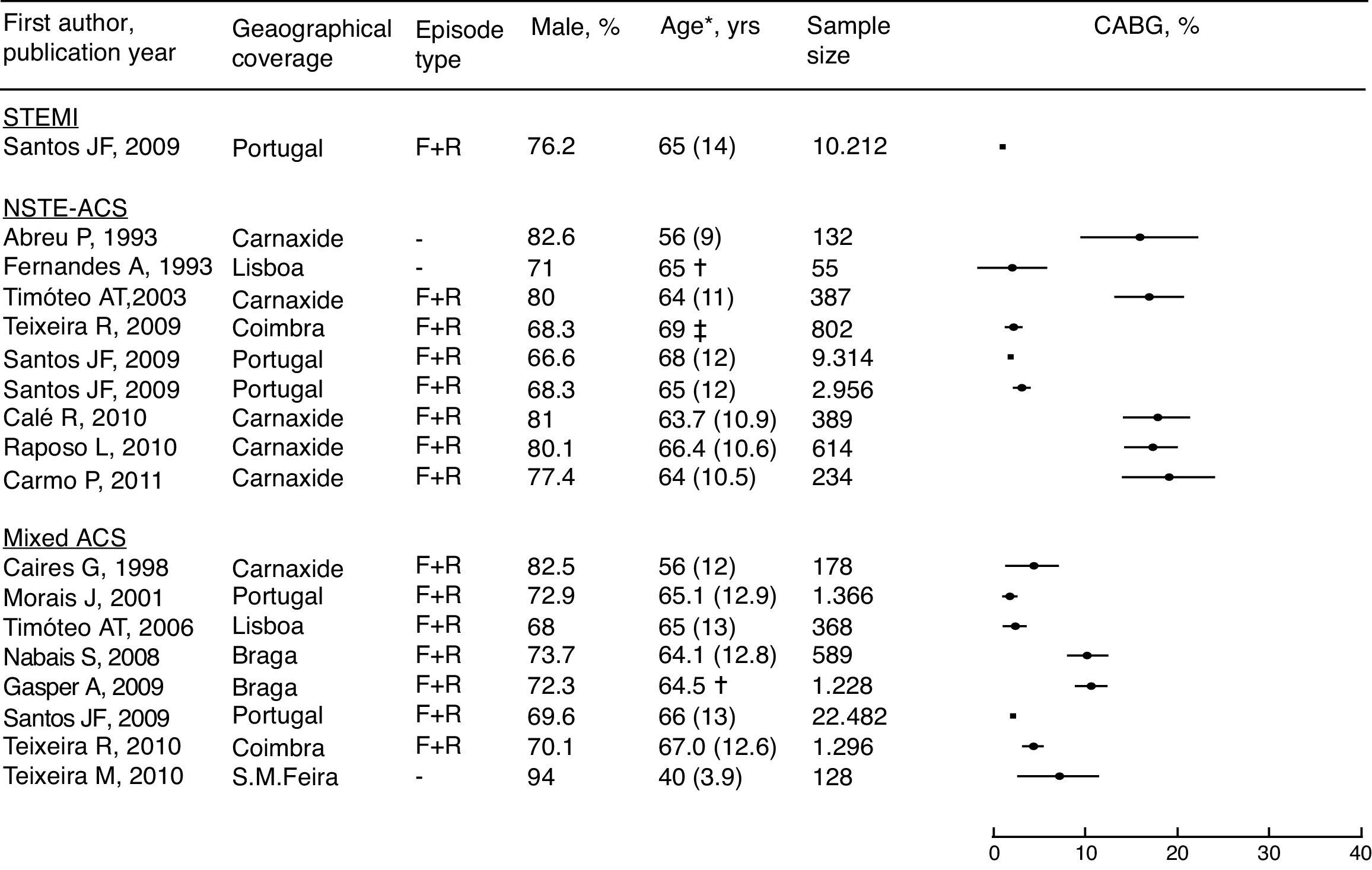
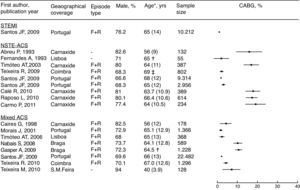
CABG was used in 1.0% of STEMI patients (this figure available only from the National Registry of Acute Coronary Syndromes). In NSTE-ACS and mixed ACS, 1–10% of patients were reported as undergoing CABG, with no clear time trend. An exception for several reports is a single institution (Hospital de Santa Cruz, in Carnaxide) over the years, with a proportion closer to 20% of NTSE-ACS patients having undergone surgical revascularization during hospitalization for the acute event (Figure 4).
Proportion of acute coronary syndrome patients treated with CABG in Portugal, estimated in unselected samples of patients. CABG: coronary artery bypass grafting; F: first episode; mixed ACS: mixture of patients with several types of ACS; NSTE-ACS: 90% or more patients with diagnosis of non-ST-segment elevation ACS; R: recurrent episode; STEMI: 90% or more patients with diagnosis of ST-segment elevation myocardial infarction or Q-wave myocardial infarction. * Age is presented as mean (SD) unless otherwise specified; † mean age; ‡ median age.
Despite considerable heterogeneity in the methodology and presentation of results of available studies, this review shows that the proportion of ACS patients in Portugal treated with fibrinolysis has decreased in the last 20 years and the use of PCI has increased, while the use of CABG has not changed.
Since the late 1970s, more aggressive and effective treatments have been developed and implemented for the treatment of CHD, including fibrinolysis, PCI and CABG.21 Of the primary studies included in the present review, the oldest with data on fibrinolysis was published in 1989,22 while PCI and CABG were first mentioned in an article published in 1993 (data collection in 1982).23 Data from previous years were reported in a few publications which were excluded mainly due to the reporting format, for example lack of data on sample size or patients’ sex and age, or because the use of procedures in the acute hospitalization or over variable follow-up periods could not be distinguished.
During the last decade, mechanical or pharmacological reperfusion therapy has been recommended for all patients with STEMI who present within 12 hours of the onset of symptoms.24–26 A growing body of evidence has also demonstrated beneficial effects of reperfusion therapy in patients presenting more than 12 hours from symptom onset. In this group of patients, recent recommendations consider this treatment a strong indication, preferably by primary PCI (class I) if there is evidence of ongoing ischemia or if pain and electrocardiographic changes have been stuttering. Primary PCI may be also considered even in asymptomatic patients presenting 12–24 hours after symptom onset.25 For years, fibrinolysis was chosen over primary PCI, mainly due to its greater ease of access and use.21 However, mechanical reperfusion has been preferred since several randomized clinical trials and meta-analyses comparing primary PCI with in-hospital fibrinolytic therapy in patients presenting within 6–12 hours of symptom onset showed more effective restoration of vessel patency, less reocclusion, reinfarction and stroke, improved left ventricular function and less short-term mortality with primary PCI.27,28 National6,29 and international registries in Europe30,31 and the USA32,33 suggest an increase in the use of reperfusion therapies accompanied by a significant shift from fibrinolysis therapy to primary PCI. A significant decrease in mortality after STEMI has been observed in countries switching from fibrinolysis to primary PCI.34 In our study, we observed decreased use of fibrinolysis and increased use of primary PCI. In this review, most of the studies providing data on fibrinolysis were published in the 1990s, with data collected in the 1980s and 1990s. By contrast, the studies addressing primary PCI were only published in the current century. Although the trends cannot be quantified, fibrinolysis appears to have been replaced by primary PCI.
Since its introduction in 1977, angioplasty has become the most frequently performed major intervention in medicine,35 as both a reperfusion (primary PCI) and revascularization procedure. Among the included studies addressing the use of revascularization by a percutaneous procedure, one sixth were published in the 1990s and the remainder afterwards. Surgical revascularization with CABG was first introduced in 1969, and become the most thoroughly studied procedure in the history of surgery.36 In our review, a quarter of the studies were published in the 1990s and the remainder after 2000. Although the primary studies provided information on surgeries performed at different times related to the acute event (e.g. during a variable time of follow-up after the acute event), we only included studies with data on CABG performed during the initial hospitalization. Otherwise, the data to be compared would be even more heterogeneous. Particularly for this procedure, it is important to point out that many patients referred for CABG are expected to have undergone surgery after discharge or have been transferred to a different institution while awaiting the procedure,6 thus reducing the proportion of patients treated that were captured by this analysis.
The results on revascularization therapies are consistent with the findings of previous studies showing an increase in PCI use and non-significant changes in use of CABG in recent years.30,37,38 In patients stabilized after an episode of acute coronary syndrome, the choice of revascularization modality can be made as in stable coronary heart disease.25,39,40 In single-vessel disease, which occurs in one-third of patients with ACS, ad-hoc PCI is feasible in most cases, whereas in patients with multivessel disease (approximately half of cases) the decision on the type of revascularization is more complex.41,42 Options for this condition have evolved over time, and currently include culprit lesion PCI, multivessel PCI, CABG or hybrid (combined) revascularization, according to clinical status, lesion characteristics and the severity and distribution of coronary artery disease.25,39,40
Our methodology has some limitations. The use of a single search engine may have limited our results. However, the inclusion of relevant studies identified in the reference lists of the review articles should have helped identify older and non-PubMed-indexed publications. The probability of identifying relevant studies from among those published is also influenced by their results because, despite the descriptive nature of the studies, publication bias can be expected, with higher likelihood of publication from higher-quality or at least higher-volume centers. It is noteworthy that the majority of studies came from cardiology departments, some of which also contributed to the National Registry of Acute Coronary Syndromes. Therefore, the main gain with this review is its coverage of a greater time span, but not the representation of less specialized centers than those included in the National Registry of Acute Coronary Syndromes. The results are affected by the methodological heterogeneity of the studies, particularly inclusion criteria, sample size, and patients’ age and sex, as well as the relatively small number of estimates for each type of treatment under study. Another limitation for more informative conclusions stems from the small number of studies with sex-, age-, and year-specific estimates, as authors mainly reported overall data. Some reported data referring to a period longer than one year; however, it was not possible to obtain year-specific estimates.
Given these limitations, an alternative approach to the study of trends in the use of these treatments in the past could be to rely on administrative databases, using data collected, coded and stored, immediately available for analysis.43 The national register of hospital discharges29 could be used to quantify the number of procedures performed, but the usefulness of these datasets is limited: it is not possible to classify the subtypes of ACS according to current recommendations44 when departing from data coded using the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM). Furthermore, there is no information available in the database to ascertain the timing of PCI or to identify recurrent episodes in the same patient.29
ConclusionsThe general pattern of treatment reflects what is reported in other developed countries and can be viewed as a favorable time trend in the quality of care of ACS patients. Future investigation should focus on the prospective and systematic recording of high-quality information to monitor the use of treatments in this acute condition, while past trends can only be properly clarified by an original retrospective study on a representative sample of ACS patients, involving review of hospital records.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis study was funded by a grant from Fundação para a Ciência e a Tecnologia (PIC/IC/83006/2007).
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors gratefully acknowledge the contribution of authors who provided data different from that presented in their original reports, which were important for decisions of selection and presentation of data in our analysis.