This study aimed to evaluate the impact of the COVID-19 pandemic on healthcare provided to patients with arterial hypertension in Portugal.
MethodsThe pre-pandemic and pandemic periods were compared using publicly available data on performance and health outcome indicators from the Portuguese National Health Service (NHS). Pre-pandemic data were modeled to project hypothetical scenarios without a pandemic using an exponential smoothing algorithm, and then compared with data collected during the COVID-19 pandemic. A cohort model was developed to estimate the number of all-cause deaths and years of life lost (YLL) due to the reduction in blood pressure (BP) monitoring and in BP records <150/90 mmHg during the first two years of the pandemic. Microsoft Excel® was used for statistical analyses.
ResultsThere was a 26.4% relative reduction in the number of patients with hypertension under 65 years of age with at least one BP measurement, and a 21.8% relative reduction in the proportion of patients with BP <150/90 mmHg during the first two years of the pandemic. The model projections were 176 additional deaths and 3287 YLL among the Portuguese population of patients with hypertension.
ConclusionsThe disruption in BP testing in Portugal during the pandemic increased hypertension-associated morbidity and mortality, with significant YLL. The long-term implications of impaired monitoring of patients with hypertension should be assessed, and proactive strategies implemented to mitigate the increase in hypertension morbidity and mortality associated with the COVID-19 pandemic.
Este estudo teve como objetivo avaliar o impacto da pandemia de COVID-19 nos cuidados de saúde prestados aos doentes hipertensos em Portugal.
MétodosOs períodos pré-pandémico e pandémico foram comparados utilizando dados disponíveis publicamente sobre indicadores de desempenho e de resultados de saúde do Serviço Nacional de Saúde português. Os dados de pré-pandemia foram modelados para projetar cenários hipotéticos sem pandemia utilizando um algoritmo de suavização exponencial, e foram depois comparados com os dados recolhidos durante a pandemia. Um modelo por coortes permitiu estimar o número de mortes por todas as causas e os anos de vida perdidos devido à redução na monitorização da pressão arterial (PA) e nos registos de PA <150/90 mmHg.
ResultadosVerificou-se uma redução relativa de 26,4% no número de doentes hipertensos com menos de 65 anos com pelo menos uma medição de PA, e uma redução relativa de 21,8% na proporção de doentes com PA <150/90 mmHg durante os primeiros dois anos de pandemia. As projeções são de 176 mortes adicionais e 3.287 anos de vida perdidos na população portuguesa de doentes hipertensos.
ConclusõesA disrupção nos testes de PA em Portugal durante a pandemia fez aumentar a morbilidade e mortalidade associadas à hipertensão arterial, com uma perda significativa de anos de vida. As implicações a longo prazo da monitorização insuficiente de doentes hipertensos devem ser avaliadas, e devem ser implementadas estratégias para mitigar o aumento da morbilidade e mortalidade por hipertensão associadas à pandemia de COVID-19.
The COVID-19 pandemic was declared by the World Health Organization on 11 March 2020.1 The first case of COVID-19 in Portugal was reported on 2 March 2020. By September 2023, 5.6 million cases of COVID-19 had been officially confirmed, resulting in approximately 27.2 thousand deaths.2
The increase in total mortality observed during the COVID-19 pandemic cannot be entirely explained by the direct effects of the disease.3 In the first two months of the pandemic, an excess mortality was estimated of 3.5–5 times higher than that attributable to the official number of COVID-19 deaths in Portugal.4 In England and Wales, 47 243 excess deaths were reported between March and May 2020, of which over a fifth were not directly attributed to COVID-19.3 As such, the pandemic had negative repercussions on the population's health beyond those caused by COVID-19 itself.5,6
The strategies implemented to control the dissemination of the virus posed a challenge to healthcare systems, with cancellations and delays in elective and non-urgent medical procedures.5,6 A systematic review of the literature enabled the identification of a decrease in the use of health resources by about a third during the pandemic.7 Medical appointments were reduced by 42%, hospitalizations by 28%, diagnostic tests by 31%, and therapeutic interventions by 30%.7
Routine consultations for chronic disease management decreased significantly during the COVID-19 pandemic, with patients with hypertension being among the most affected.8,9 In Europe, a study conducted among Excellence Centers of the European Society of Hypertension (ESH) revealed a marked reduction in the number of patients treated per week, as well as a decrease in diagnostic and therapeutic interventions for hypertension management.10 In the United States of America (USA), a study using data from an integrated healthcare system revealed that more than one-fourth of patients with hypertension who had their blood pressure (BP) measured before the pandemic did not have any measurements taken during the pandemic. These patients were found to have an increased probability of dying during the year.11 A different study indicated that patients with hypertension were 50% less likely to have a BP measurement in April 2020 when compared to February of the same year.12
There was a drop in the healthcare provision services of the Portuguese National Health Service (NHS), with a reduction in the number of consultations, both in primary and in hospital healthcare, a decrease in the number of elective surgeries and a slowdown in disease screening programs.13 Therefore, it is thought that the provision of arterial hypertension care has been negatively affected by the pandemic in Portugal.
ObjectivesThis study aimed to evaluate the impact of the COVID-19 pandemic on the healthcare provided to patients with hypertension by the Portuguese NHS, and to estimate the respective consequences on arterial hypertension-associated morbidity and mortality.
MethodsThis study utilizes publicly available data on performance and health outcome indicators of the Portuguese NHS to compare the pre-pandemic period (January 2015–February 2020) with the pandemic period (March 2020–February 2022). Pre-pandemic data were modeled to project hypothetical scenarios in which the pandemic would have not occurred. The data resulting from these projections were then compared with data collected during the pandemic. Differences between hypothetical scenarios and real-life outcomes were used to evaluate the potential impact of alterations in healthcare provision in the monitoring of arterial hypertension within the Portuguese NHS on morbidity and mortality in the country.
Data sourceData were obtained from the Transparency Portal of the Portuguese NHS.14 This website aggregates health data from diverse entities in Portugal and provides public access to these datasets. The “Hypertension Program Activ”y” database was used in this analysis to assess the variation in morbidity associated with arterial hypertension during the COVID-19 pandemic. Data collected during the pre-pandemic and pandemic periods include the following:
- •
Number of registered users aged <65 years with a diagnosis of arterial hypertension and at least one record of BP measurement in the previous 6 months; and
- •
Proportion of patients with hypertension aged <65 years with the last BP record of less than 150/90 mmHg.
Data collected during the pre-pandemic period we modeled to project hypothetical scenarios in which the pandemic would not have occurred. This estimate assumed that, without a pandemic, the evolutionary pattern observed during the pre-pandemic period would continue thereafter.
To perform the forecast, an exponential smoothing algorithm ETS (Error, Trend, and Season) was used, which allowed to estimate hypothetical values on specified target dates, as a continuation of previous historical values, taking seasonality into account. In this case, the “FORECAST.ETS” function was used in the Microsoft 365® ExcelTM. The function syntax is FORECAST.ETS (target_date, values, timeline, [seasonality], [data_completion], [aggregation]), using an annual ‘seasonal’ty’ (i.e., reflects the monthly variations throughout each year), missing values treated as zero for ‘data complet’on’ and sum or average for the variable ‘aggregat’on’ (depending on the type of variable being analyzed, i.e., absolute counts or proportions).
The estim’ted hypothetical values (forecasts without a pandemic) were compared with the values observed during the pandemic period to identify the impact of the pandemic on health care provision (i.e., on the different NHS performance indicators under analysis). Absolute and relative differences between predicted values and observed values were calculated using Microsoft 365® ExcelTM.
Mortality due to inadequate arterial hypertension monitoringThis analysis aimed to estimate the potential impact of the pandemic on all-cause mortality among patients with hypertension, as a consequence of the decrease in NHS care provided to those patients, including in diagnosing and monitoring arterial hypertension.
The results obtained by the NHS during the pandemic were used for arterial hypertension morbidity indicators (number of registered users with a diagnosis of arterial hypertension and at least one BP measurement in the last 6 months; and proportion of patients with hypertension with the last BP record of less than 150/90 mmHg) and an ETS exponential smoothing algorithm was applied to project estimated results for these same indicators in a hypothetical scenario without a pandemic. Based on these data, the following was calculated for the hypothetical scenario without a pandemic (A) and for the real scenario with a pandemic (B):
- i.
the number of patients with hypertension who were no longer treated (i.e., were no longer followed up in consultation);
- ii.
the number of patients with hypertension who continued to be treated and maintained BP <150/90 mmHg; and
- iii.
the number of patients with hypertension who continued to be treated but no longer maintained BP <150/90 mmHg.
A cohort model was then developed to estimate the number of deaths from all causes associated with each of these disease states in the hypothetical scenario without a pandemic (A) and in the real scenario with a pandemic (B). This model is based on applying a specific hazard ratio (HR) value to each disease state (treated and BP <150/90 mmHg; treated and BP ≥150/90 mmHg; or untreated) to estimate the increase in mortality associated with arterial hypertension. The HR values for the risk of death (from any cause) used in the model were obtained from an observational study of around 14000 adults.15 In that study, the HRs compared to a normotensive reference population were as follows: HR=1.40 (95% CI=1.21–1.62) for the population of untreated patients with hypertension; HR=1.16 (95% CI=0.95–1.42) for the population of treated patients with hypertension with BP <140/90 mmHg; and HR=1.62 (95% CI=1.35–1.95) for the population of treated patients with hypertension with BP ≥140/90 mmHg.15 These HRs were applied in our model, despite the systolic BP threshold defined in the Zhou et al. study being lower than the boundary used in the Portuguese database. This may result in an underestimation by the model of deaths in the Portuguese population.
In the following step, the two-year forecasts for the hypothetical scenario without a pandemic (A) were compared with the results obtained for the real scenario with a pandemic (B) to estimate the differences in mortality and total years of life lost (YLL).
To estimate the total number of YLL, the model incorporated the average age at diagnosis of arterial hypertension in Portugal (54.3 years),16 as well as the average life expectancy of patients with hypertension in Portugal (73.0 years – estimated by applying a HR [=1.4] to the average life expectancy of the general population in Portugal). The projections of YLL considered, for each patient who dies early due to insufficient monitoring, the difference between the average life expectancy of a patient with hypertension and the average age of the patient. The adjustment to a pati’nt's average life expectancy was calculated using the HRs obtained and considering that the number of years until death as the expected value for a probability variable (annual mortality rate) follows a negative binomial distribution.
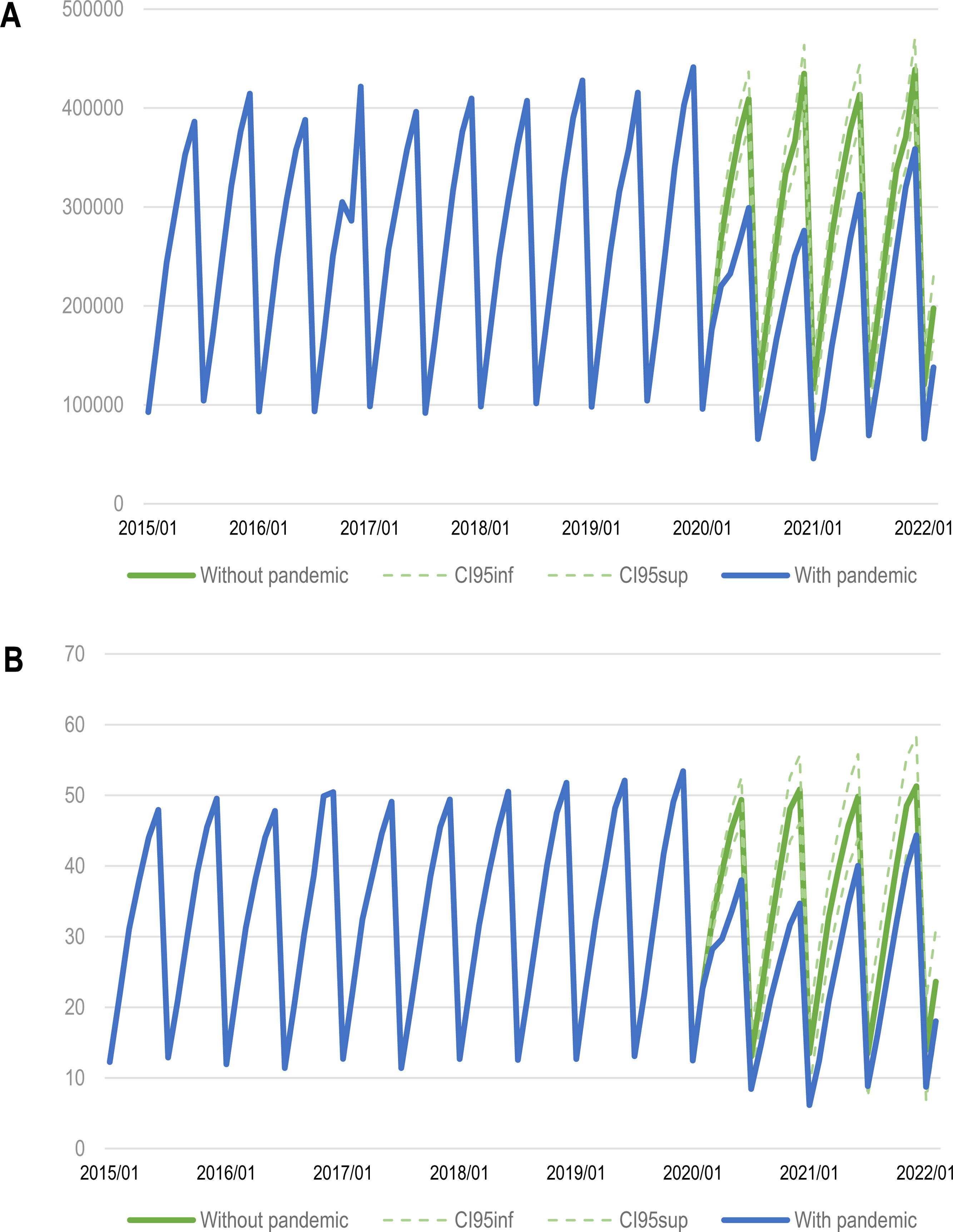
ResultsImpact of the pandemic on arterial hypertension-associated morbidityThe total number of patients with hypertension <65 years of age with at least one BP measurement in the previous six months decreased from the first month of the pandemic and remained below the expected value throughout the pandemic period (between March 2020 and February 2022) (Figure 1A). The same trend was observed for the proportion of patients with hypertension <65 years of age with at least one BP measurement in the previous six months and a last record <150/90 mmHg (Figure 1B).
Impact of the pandemic on arterial hypertension morbidity: number of patients with hypertension under 65 years of age with at least one blood pressure measurement in the previous six months in Portugal (A) and proportion of these patients with a last record <150/90 mmHg (B). CI: confidence interval; inf: inferior; sup: superior.
Source: NHS Transparency Portal (data extracted on April 27, 2022).
There was a 26.4% relative reduction in the number of patients with hypertension <65 years of age with at least one BP measurement in the previous six months (312000 observed versus 424000 expected) (Figure 1A). Regarding the proportion of patients with hypertension whose BP was <150/90 mmHg, a relative reduction of 21.8% was witnessed (39.3% observed versus 50.3% expected) (Figure 1B).
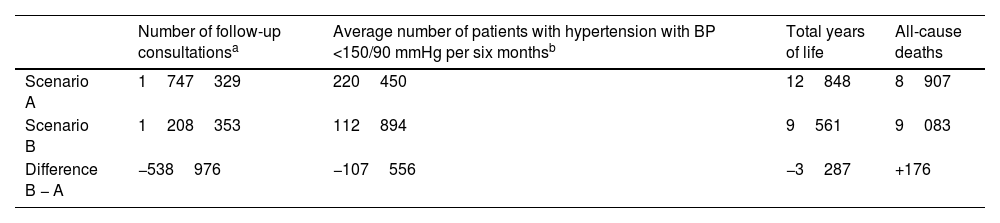
Impact of insufficient arterial hypertension monitoring on mortality during the pandemicTable 1 presents the results obtained for the total years of patients with hypertension and the number of all-cause deaths during the pandemic period in scenario A (without pandemic) and scenario B (with pandemic).
Impact of the pandemic on the mortality of patients with hypertension.
| Number of follow-up consultationsa | Average number of patients with hypertension with BP <150/90 mmHg per six monthsb | Total years of life | All-cause deaths | |
|---|---|---|---|---|
| Scenario A | 1747329 | 220450 | 12848 | 8907 |
| Scenario B | 1208353 | 112894 | 9561 | 9083 |
| Difference B − A | −538976 | −107556 | −3287 | +176 |
Scenario A: without pandemic; scenario B: with pandemic.
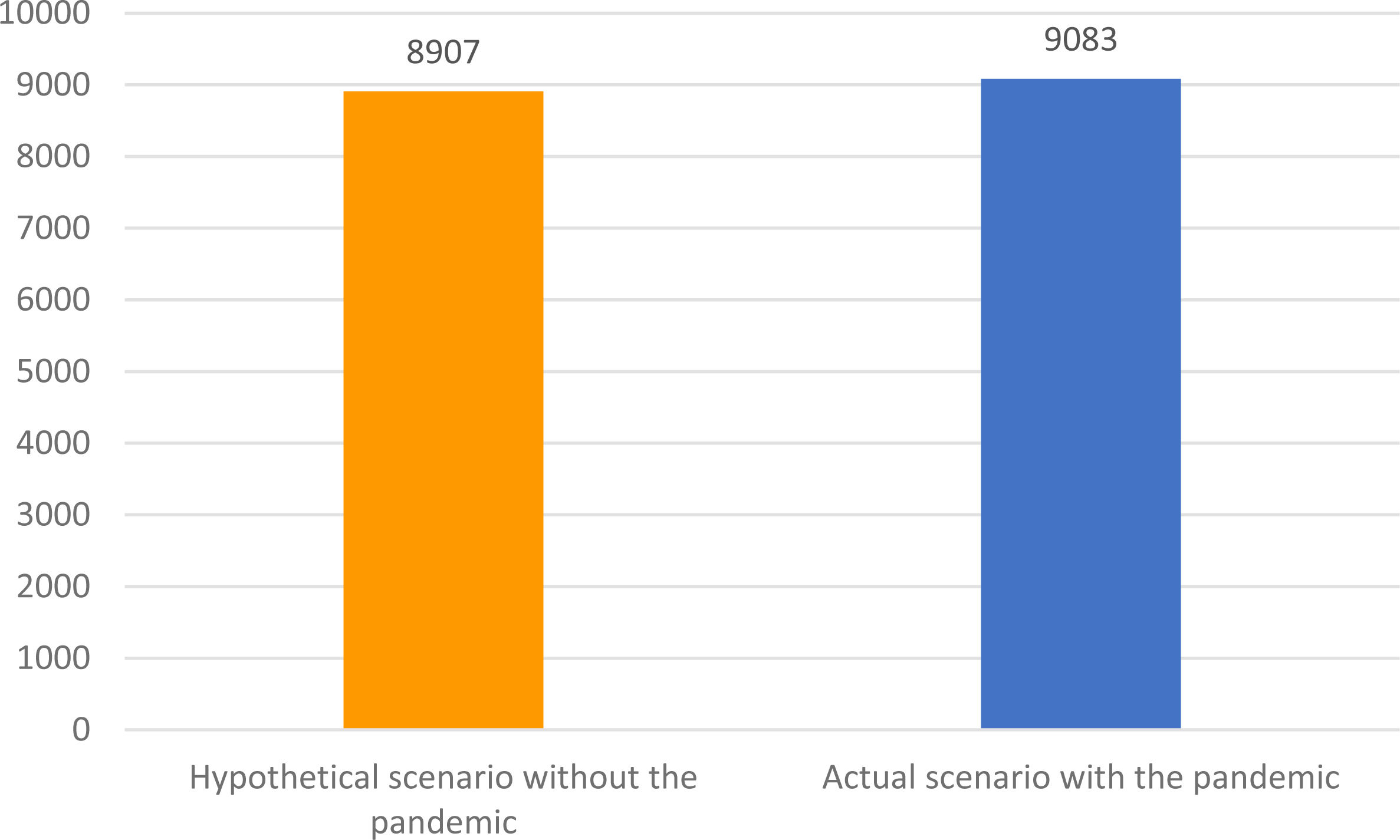
During the first two years of the pandemic, there were 176 additional all-cause deaths in the Portuguese population of patients with hypertension as a consequence of the impact of the pandemic on the monitoring of these patients, which corresponds to a 2.0% increase in mortality (Figure 2).
Approximately 3287 years of life were lost due to insufficient monitoring of patients with hypertension during the first two years of the pandemic.
DiscussionThis study enabled us to quantify the impact of the COVID-19 pandemic on the health of patients with hypertension living in Portugal, by analyzing indicators of arterial hypertension morbidity and mortality, and indicators of performance of the NHS in pre-pandemic and pandemic periods.
There was a 26.4% relative reduction in the number of patients with hypertension <65 years of age who had a BP measurement during the first two years of the pandemic compared to what would have been expected in a hypothetical pandemic-free scenario. In addition to the decrease in the number of patients attending monitoring consultations, a reduction in the number of arterial hypertension diagnosis was also anticipated, although the data do not allow for this distinction to be made.
Similar trends were observed in different regions of the world. In Europe, a study conducted among Excellence Centers of the European Society of Hypertension (ESH) reported a reduction in hypertension diagnostic tests by 1/3 in 2020 when compared to 2019, with reductions ½1/2 happening during the lockdown periods. Ambulatory BP monitoring decreased 30.8% in 2020.10 In the USA, a study using data from an integrated healthcare system reported that 27.4% of patients with hypertension with BP measurement records in the pre-pandemic period (March 2019–February 2020) had no BP measurements during the pandemic (March 2020–February 2021). In addition, the patients without BP measurements had an increased probability of dying during the year when compared to patients with BP measurements (3.1% versus 1.7%).11 Similarly, an analysis of ambulatory care electronic health record data from patients with BP >140/90 mmHg in Massachusetts reported a sharp decline in the percentage of patients with a valid BP measurement, from 40.0% in January 2020 to 4.5% in April 2020. This percentage remained significantly below pre-pandemic records throughout the pandemic, reaching only 16.5% in March 2021.17 A different study indicated that patients with hypertension were 50% less likely to have a BP measurement in April 2020 when compared to February of the same year.12
Our results also demonstrated a downward trend for the proportion of patients with hypertension whose BP was <150/90 mmHg, with a relative reduction of 21.8% when compared to a hypothetical scenario without the pandemic. These observations seem to be plausible, given that a decrease in the proportion of patients with normal BP values was also verified in the USA18–20 and Argentina21 during the pandemic. Furthermore, an interrupted time series analysis conducted in the USA reported an increase in BP (by 1.79 mmHg in systolic and 1.30 mmHg in diastolic BP) during the pandemic period (April 2020–November 2020) when compared to the pre-pandemic period (August 2018–January 2020).18 Similar results were documented by other studies, using both in office-measured BP data22 and home BP data.19
Studies conducted in Spain,23 the United Kingdom (UK),24 and USA11 have also revealed an adverse effect of the COVID-19 pandemic on the adherence to hypertension treatment. An analysis using data from England, Scotland and Wales between April 2018 and July 2021 reported a decrease in the dispensing of antihypertensive medication during the pandemic period (March 2020–July 2021), with 491306 fewer individuals starting treatment compared to what would have been expected. This decline was estimated to lead to 13662 additional cardiovascular disease incidents if these individuals remain untreated throughout their life course.24
Conversely, other studies reported no major adverse effects of the COVID-19 pandemic on hypertension monitoring. Studies conducted in France,25 Italy,26,27 and Brazil28 reported similar or even lower BP values during the pandemic period when compared to the pre-pandemic period. In addition, no differences in adherence to hypertension treatment were observed before and during the pandemic.27,28
Considering the rise of the proportion of patients with higher BP values during the pandemic, an increased risk of mortality among patients with hypertension was expected. Probabilistic modeling allowed us to estimate the impact of the decrease in care provided to patients with hypertension on arterial hypertension-associated mortality in Portugal during the first two years of the pandemic. The lack of information concerning the period during which each patient had BP >150/90 mmHg represents a limitation in our model. The risk of death is anticipated to rise with increasing duration of BP >150/90 mmHg. On the other hand, in order to estimate the number of YLL by the population, it was necessary to use average ages at the time of diagnosis of the disease, as well as the average life expectancy of patients with hypertension, given that it was not possible to identify data on the distribution of these and other characteristics, such as gender, in the population of patients with arterial hypertension. The HR values used in the model to estimate the increase in mortality were obtained from an observational study of around 14000 adults.15
According to the results obtained in the simulation model, there were 176 additional deaths among the Portuguese population of patients with hypertension during the first two years of the pandemic (i.e., a 2.0% increase in arterial hypertension-associated mortality). Moreover, 3287 years of life were lost during the same period. As arterial hypertension represents a major health concern, these results demonstrate how important it is to increase the awareness and the proportion of patients achieving recommended BP targets.29
In addition to using a validated method to estimate arterial hypertension-associated mortality and life expectancy, one of the strengths of the present study lies in the fact that official and publicly available data from the Portuguese NHS were used in the analyses, including data recorded for more than seven years. Conversely, the lack of granularity of the data is a limitation that prevents the possibility of adjusting for possible confounders and risk factors for arterial hypertension, or sub-analysis for age, sex, and other characteristics. The results obtained in our study should be interpreted bearing in mind that the model evaluates the impact of only one hypertension-related routine analysis (i.e., BP measurement) on mortality and life expectancy. However, other diagnostic tests and interventional procedures are important in hypertension care and were also negatively affected during the COVID-19 pandemic.10
The following limitations should be noted. The “Hypertension Program Activity” database from the Portuguese NHS reports data on patients with hypertension aged <65 years with the last BP record of less than 150/90 mmHg. Data were not available for patients aged ≥65 years. The prevalence of hypertension increases with age, where 60% and 75% of patients aged >60 years and aged >75 years have hypertension, respectively.30 Older patients are more likely to have comorbidities and lower adherence rates to antihypertensive medications, increasing the risk of morbidity and mortality.30 Moreover, the aforementioned arterial hypertension indicator uses a BP threshold <150/90 mmHg resulting in a set of patients with systolic BP between 140 and 150 mmHg registered in this database and considered as having a “controlled” BP. The most recent clinical guidelines recommend that the first objective of treatment should be to lower BP to <140/90 mmHg in all patients. Lower values for systolic BP can be targeted if treatment is well tolerated and diastolic BP <80 mmHg should be considered for all patients.30 Scientific evidence suggests that the benefits from treatment are greater for patients at higher absolute levels of cardiovascular disease risk.31 However, one cannot neglect the fact that the gap between the systolic BP target of 140 mmHg stated in the clinical guidelines and threshold of 150 mmHg in the Portuguese NHS indicator corresponds to a group of patients with arterial hypertension at a slightly higher risk of mortality. In addition, this indicator considers patients with at least one BP measurement in a previous six-month span, which may represent extended periods of time where blood pressure fluctuations cannot be registered, or proper monitoring and treatment be ensured. Thus, not only the results from this study should be interpreted with caution, but further studies are also necessary to assess the long-term implications of impaired monitoring of patients with hypertension during the pandemic. As new waves of the pandemic or other public health emergencies may occur in the future, it is essential for the Portuguese NHS to develop effective strategies to mitigate the adverse impact on the population with arterial hypertension.
ConclusionsThe COVID-19 pandemic led to a reduction in BP measurements in the Portuguese population with arterial hypertension compared to what would be expected in a hypothetical pandemic-free scenario, as well as a decrease in the proportion of patients with BP <150/90 mmHg. This contributed to a rise in hypertension-associated mortality, resulting in thousands of YLL among the population.
FundingAPIFARMA – Associação Portuguesa da Indústria Farmacêutica provided financial support for the conduct of the research, but was not involved in study design, in the collection, analysis and interpretation of data, in the writing of the report, nor in the decision to submit the article for publication.
Conflicts of interestThe authors declare that they have no known competing financial interests or personal relationships that could have appear to have influenced the research reported in this paper.