A clinical observation is reported in hypertensive patients taking clonidine, which was originally used to reduce blood pressure, but can hinder blood pressure control when its use is combined with a monoamine oxidase inhibitor (MAOI). One typical case was selected and analyzed. The clinical phenomenon of uncontrolled hypertension caused by this drug interaction has not been reported in the literature.
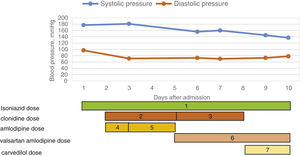
A 64-year-old Chinese male (normal body mass index of 20 kg/m2), with a history of hypertension for more than 10 years and hyperglycemia for more than 30 years, received regular hemodialysis three times per week for three years. On admission, the patient, with a blood pressure of 177/97 mmHg, was taking clonidine 75 μg three times daily and amlodipine 5 mg once daily for hypertension. Two weeks before admission, he was diagnosed with tuberculous pleurisy and treated with isoniazid, rifampicin and ethambutol. On day 3, the patient's blood pressure reached 181/71 mmHg, with chest discomfort experienced after breakfast. Nitroglycerin was given temporarily, and amlodipine was increased to 5 mg twice daily. Although amlodipine was replaced with valsartan/amlodipine and the clonidine dose was increased to 75 μg every 6 h on day 5, the patient's systolic blood pressure still fluctuated between 150 and 160 mmHg. During this period, nifedipine was given temporarily several times as symptomatic treatment, but the patient's blood pressure was still difficult to control. After ruling out risk factors for poorly controlled blood pressure such as secondary hyperthyroidism, sleep apnea syndrome and poor dry weight control on dialysis, we began to consider drug factors. Reviewing the patient's medication, we hypothesized that the interaction between isoniazid and clonidine might be the reason for the difficulty in blood pressure control. Thus clonidine was switched to carvedilol on day 8. The patient's blood pressure then decreased to 145/73 mmHg on day 9 and was 137/78 mmHg at discharge (Figure 1).
Our patient was given clonidine because of high blood pressure after admission. However, instead of his blood pressure falling, it rose even higher, both when the dosage of antihypertensive drugs was increased and when more types of antihypertensive drugs were used. After reviewing his medication, it was hypothesized that the potency of clonidine was influenced by isoniazid, a monoamine oxidase inhibitor (MAOI).1 MAOIs include a variety of commonly used drugs, including antibacterials such as isoniazid, linezolid, and furazolidone; selegiline (an antiparkinsonian agent); and leflunomide (an immunosuppressant), among others. However, an interaction between these MAOIs and clonidine is not noted either in their specification or in the literature.1,2 The mechanism of interaction between clonidine and MAOIs is not fully understood. Clonidine activates presynaptic alpha-2 adrenergic receptors and inhibits the release of norepinephrine (NE) into the synaptic space via a negative feedback mechanism.3 Under normal conditions, the inhibited NE will be metabolized and inactivated by MAO-A and catechol-O-methyltransferase.4 However, the concentration of NE in the presynaptic membrane is increased when combined with MAOIs that selectively inhibit the activity of MAO-A.5 When the accumulation of NE in vesicles reaches a certain level, it is suddenly released and acts on the postsynaptic membrane, resulting in a hypertensive crisis.
When this occurred in our case, after symptomatic treatment nifedipine failed to resolve the patient's hypertension, clonidine was switched to carvedilol. There was subsequently a significant drop in blood pressure. By the time of discharge, the patient's blood pressure had recovered to less than 140/90 mmHg.
We present a case with uncontrolled blood pressure due to drug-related effects. We recommend that cardiologists do not prescribe clonidine and a MAOI at the same time, to avoid a hypertensive crisis, and hope by reporting this case to reduce the occurrence of adverse clinical reactions.
FundingNone declared.
Conflicts of interestThe authors have no conflicts of interest to declare.