Infective endocarditis affects cardiac valves or devices and has a potentially uncertain prognosis. Little information is available on the epidemiology of this disease in Portugal.
ObjectiveA systematic review of all evidence published in the last 30 years to assess epidemiological data in patients hospitalized with infective endocarditis in Portuguese hospital centers.
MethodsExtensive search of all published evidence using Medline, Scopus, general search databases and in addition Portuguese medical journals was performed. All relevant studies in Portuguese or English that reported short- or long-term mortality were included.
ResultsEighteen retrospective cohort studies (15 medical and three surgical series) were included with a total of 1872 patients assessed. The medical series included 1279 patients. Older males with predominant native left heart valve involvement were identified. Staphylococcus and streptococcus were the most frequent reported pathogens. Surgical intervention was performed on average in 29.8% of cases. The short-term mortality rate ranged from three to 37.2% (average 21.9%). Surgical cases involved older males with affected native left heart valves, emergent/urgent indication was dominant and short-term mortality ranged from 13.6 to 16%.
ConclusionsThe current study provides a descriptive analysis of the published series of infective endocarditis in Portugal over the last 30 years. Therefore, it may serve as a starting point for the development and implementation of a multicentric prospective registry on infective endocarditis patients in Portugal that will allow a better and more accurate characterization of this special patient population.
A endocardite infeciosa afeta válvulas ou dispositivos cardíacos e tem um prognóstico potencialmente incerto. Pouca informação está disponível sobre a sua epidemiologia em Portugal.
ObjetivoRevisão sistemática de todos os estudos publicados nos últimos 30 anos que avaliaram dados epidemiológicos em pacientes hospitalizados com endocardite infeciosa em centros hospitalares portugueses.
MétodosUma pesquisa detalhada de todos os estudos publicados, usando a Medline, Scopus, motores de busca generalistas e também revistas médicas portuguesas, foi realizada. Todos os estudos relevantes em português ou inglês que relataram mortalidade em curto ou longo prazo foram incluídos.
ResultadosDezoito estudos de coorte retrospetivos (15 séries médicas e 3 cirúrgicas) foram incluídos com um total de 1872 pacientes avaliados. As séries médicas incluíram 1279 doentes. Identificaram-se homens mais velhos com envolvimento predominante de válvulas cardíacas esquerdas nativas. Staphylococcus e Streptococcus foram os agentes envolvidos mais frequentemente. A intervenção cirúrgica foi realizada em 29,8% dos casos (valor médio). A taxa de mortalidade em curto prazo variou entre 3 e 37,2% (média 21,9%). Os casos cirúrgicos incluíram homens mais velhos com envolvimento das válvulas esquerdas nativas, a indicação emergente/urgente dominou e a mortalidade em curto prazo variou entre 13,6 e 16%.
ConclusõesO estudo atual fornece uma análise descritiva de todas as séries de endocardite infeciosa publicadas em Portugal nos últimos 30 anos. Pode servir como ponto de partida para o desenvolvimento de um registo prospetivo multicêntrico em pacientes com endocardite infeciosa em Portugal, que permitirá uma caracterização mais rigorosa desta população específica de doentes.
Cardiovascular disease accounts for 45% of all deaths in Europe and 37% of all deaths in the European Union.1 Ischemic cardiopathy and cerebrovascular disease are considered the major causes of cardiovascular mortality in Portugal.2
Among cardiovascular diseases, infective endocarditis (IE) is considered an uncommon cardiovascular condition - its global incidence is estimated at 3-10 episodes per 100 000 person-years.3 Nevertheless, this number is probably underestimated as the diagnosis of endocarditis is difficult and some patients remain undiagnosed. Moreover, IE in valve prosthesis and intracardiac devices4,5 has been increasing in the last decades with a growth in surgical and percutaneous valve interventions and with a more frequent implantation of pacemakers, implantable cardiac defibrillators (ICD) and cardiac resynchronization therapy (CRT) devices.
IE is linked to difficult clinical decisions and is often synonymous of long periods of hospitalization, the need for surgery and impaired quality of life. Classical risk factors such as valvular disease, previous IE and classical points of entry6,7 are now being complemented with newer clinical elements such as HIV, diabetes, cancer, immunosuppressive therapy or chronic venous catheters.4 Children with congenital heart disease that survive through adulthood, elderly patients and a broader exposure to health care interventions also increase the risk of IE.
Meanwhile, the diagnosis of IE is challenging as it requires high clinical suspicion and the need for several diagnostic exams such as blood tests, microbiology, echocardiography and computerized tomography. The epidemiology of IE is now marked by different causative organisms and drug-resistant organisms,8 with an increasing incidence of staphylococcus sp. and enterococcus sp. and a decreasing number of blood culture negative IE.9 Newer imaging modalities such as 18F2-fluoro-2-deoxy-d-glucose positron emission tomography (18F-FDG PET) are developing an important role in the diagnosis of IE, particularly in cardiac valve prosthesis.10,11
In order to reduce the incidence of IE and improve its outcome, epidemiological studies are needed to provide understanding into current, modifiable risks for IE and its morbidity and mortality. IE epidemiological studies are scarce in many countries;12 and unfortunately, Portugal is no exception13 with information mainly based on retrospective studies.
Our aim was to perform a systematic review of all observational series published in the literature or presented at scientific meetings concerning IE patients admitted to Portuguese hospital centers that reported mortality. We conducted a general descriptive analysis of clinical, therapeutic and health outcomes in these studies.
MethodsSearch methods for study identificationWe attempted to identify all relevant studies regardless of publication status (published, unpublished, in press, ongoing) written in English or Portuguese. We identified relevant studies from several databases (Table 1). In particular, we searched the conventional databases Scopus, Medline and Pubmed for articles published in any journal. In addition, we performed specific searches in targeted journals, as described in Table 1.
Search sources for studies identification.
| Included search databases | ||
|---|---|---|
| Health related databases | General databases | Medical journals |
| Medline/PubmedScopus | Google scholarSIGLERepositório Científico Acesso Aberto de Portugal (RCCAP) | Revista Portuguesa de CardiologiaRevista Medicina Interna – Portuguese Society Internal MedicineActa Médica PortuguesaRevista Portuguesa Doenças InfecciosasIndex Médico Revistas PortuguesasOxford Academic Journals |
The search strategy used a combination of subject headings and free-text keyword searching to capture the main search headings of “endocarditis” or “valve infection” and “Portugal” and “Portuguese”. Each database search strategy was adapted to match the appropriate subject headings used by that database.
Citations were screened based on the title/abstract and full texts were manually obtained for all potentially relevant articles. Additionally, we signed up to PubMed to receive automated electronic notification of any new articles containing the above search terms.
Searching other sourcesIn addition to the search methodology described above, we also manually searched papers from the Portuguese Congress of Cardiology editions from 2010 to 2019, as well as several Portuguese medical journals (Table 1). We also conducted a separate citation search on Google Scholar, SIGLE and RCCAP, which are repositories of Master and PhD thesis in Portugal.
Various authors were contacted via telephone and/or email to confirm/complete information from published series and to identify ongoing or unpublished studies relevant to the review.
Study selectionAll abstracts and articles generated were uploaded to Mendeley™. They were screened to exclude items that did not fulfill the inclusion criteria and duplicates. We independently reviewed all texts. All authors were involved in the discussion and all agreed on the final inclusion.
Inclusion and exclusion criteriaAny study that reported an IE outcome was eligible for inclusion. We included studies that fulfilled the following conditions: 1) study included a population of adult patients (>17 years old) diagnosed with IE; 2) patients hospitalized in Portuguese hospitals, regardless of the department; 3) studies should report demographics, study design and setting, clinical, imaging and microbiological aspects. With respect to in-hospital complications, we also analyzed the pooled data for heart failure, embolization, uncontrolled infection, acute kidney failure and cardiac surgery, when available; 4) studies should report outcomes. In-hospital mortality and mortality at 30 days post-discharge were classified as short-term mortality. Long-term mortality refers to the death of patients 30 days and up to two years post-discharge – when several periods were reported, we used the value with the longest duration of time; 5) if more than one publication was identified for the same hospital center, we included the most recent full article.
To improve the quality of our findings only series with ≥25 patients were included. Also, in an effort to homogenize the sample under study, specific settings such as exclusive cardiac device related, prosthetic, tricuspid valve or renal patients IE series were excluded.
Finally, only studies published after 1990 were considered. Details of the inclusion and exclusion criteria are presented in Table 2.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | Hospitalized patients with acute IEIn hospitals located in PortugalPatients ≥18 years old | Patients hospitalized with IE outside PortugalPatients <18 years old |
| Intervention | AntibioticsSurgery | |
| Outcomes | Primary outcome:Short-term mortality orLong-term mortalitySecondary outcome:Intrahospital complications (heart failure, renal complications, embolic complications or sepsis) | Studies not reporting short- or long-term mortality (primary outcome) |
| Research design | Studies that include data regarding any of the outcomes listed aboveStudies published after 1990Studies that included ≥25 patients | Studies not reporting any of the listed outcomes including:Prevalence papersCase reportsLettersEditorialsOpinion papersStudies reporting IE exclusively specific settings (CDRIE, prosthetic IE, renal failure patients) |
| Language | English or Portuguese | Articles not available in English or Portuguese |
Eighteen studies were finally included in the systematic analysis (Table 3). An example of the search conducted in PubMed is displayed in Figure 1. From this search in PubMed, a total of 149 unique articles were identified, of which 13 were selected for full text review and finally three articles were included in this systematic review.
Studies included in the systematic review.
| Study | District | Department | Surgical series | Period | Cases | Mean Age (years) | Male % | Intrahospital complications | Cardiac surgery % | Short term mortality % | Long term mortality % | STROBE % | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HF% | UInf% | Emboliz% | AKF% | ||||||||||||
| Robalo et al., 199822 | Lisbon | Internal Medicine | No | 1992-1995 | 32 | 32.5 | 78 | NA | NA | NA | NA | 16 | 3 | NA | 45 |
| Proença et al., 199923 | Lisbon | Internal Medicine | No | 1988-1998 | 65 | 31.4 | NA | NA | NA | NA | NA | 3.1 | 21.5 | NA | 36 |
| Mimoso et al., 200153 | Faro | Internal Medicine and Cardiology | No | 1990-1997 | 43 | 44.2 | 79 | NA | NA | NA | NA | 14 | 14 | NA | 45 |
| Jerónimo et al., 200654 | Porto | Internal Medicine | No | 2000-2004 | 41 | 50 | 70 | NA | NA | 17 | NA | 34 | 14 | NA | 59 |
| Aranda, 201255 | Coimbra | Cardiology | No | 2005-2010 | 78 | 60.7 | 75.6 | NA | NA | NA | NA | 29.5 | 37.2 | NA | 64 |
| Ferreira et al., 201316 | Porto | Internal Medicine and Cardiology | No | 2000-2011 | 147 | 63 | 71 | NA | 15 | 55.1 | NA | 38.8 | 31 | NA | 82 |
| a Batista et al., 201456 | Vila Real | Cardiology | No | 2000-2013 | 90 | 63.7 | NA | NA | NA | NA | NA | 26 | 12 | NA | 73 |
| a Neves et al., 201425 | Lisbon | Internal Medicine | No | 2008-2013 | 40 | 70 | 69 | NA | NA | NA | NA | 30 | 23.7 | NA | 64 |
| Santos, 201417 | Lisbon | Cardiology | No | 2001-2012 | 91 | 64.4 | 71.4 | 31.9 | NA | 15.4 | 58.2 | 31.9 | 23.1 | 33 | 68 |
| a Faustino et al., 201518 | Lisbon | Cardiology | No | 2002-2013 | 117 | 59 | 67 | 44.2 | NA | 21.1(Stroke) | NA | 31.3 | 22.1 | 29.1 | 82 |
| Lemos, 201519 | Coimbra | Cardiology | No | 2013-2014 | 25 | 59 | 72 | 60 | 28 | 28 | 56 | 52 | 28 | NA | 64 |
| Alves, 201527 | Porto | Cardiac Surgery | Yes | 2004-2014 | 320 | 60 | 69.7 | 11.5 | 6 | 24.6 | 15.1 | 100 | 15.3 | NA | 50 |
| a Santos et al., 201620 | Porto | Cardiology | No | 2005-2015 | 103 | 65.8 | 62.1 | NA | NA | NA | NA | 28.1 | 28.2 | 34 | 73 |
| Madeira et al., 201628 | Lisbon | Cardiac Surgery | Yes | 2007-2014 | 128 | 60 | 75 | 74.2 | 50 | 16.4 | NA | 100 | 16 | NA | 63 |
| Melo et al., 201724 | Lisbon | Internal Medicine | No | 2009-2014 | 40 | 62.3 | 82.1 | 53.5 | NA | 17.5 | NA | 42.5 | 17.5 | NA | 45 |
| Moreira et al., 201826 | Lisbon | Cardiology | No | 2006-2014 | 233 | 63.4 | 69.1 | 37.3 | NA | 26.2 | NA | 36.9 | 22.7 | 33 | 82 |
| Marques et al., 202021 | Setubal | Cardiology | No | 2006-2015 | 134 | 61 | 73 | 41.3 | 8.7 | 32.6 | NA | 32.8 | 31.3 | NA | 91 |
| Guiomar et al., 202029 | Porto | Cardiac surgery | Yes | 2006-2017 | 145 | 72 | 72.4 | 18.6 | 10.3 | 17.2 | 14.5 | 100 | 13.1 | NA | 86 |
AKF: acute kidney failure; Emboliz: embolization; HF: heart failure; UInf: uncontrolled infection.
Data on demographics such as age, gender, hospital setting, and study design were extracted. Medical background, clinical presentation, type of valve affected, microbiology profile, intrahospital complications (embolization, HF, refractory infection, acute renal failure, surgical intervention) and primary outcomes (short- and long-term mortality) were also retrieved.
The quality of studies was analyzed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) scale.14,15
EthicsThe study was approved by the Ethics Committee of the University of Lisbon Academic Center (reference number 349/19).
ResultsCharacteristics of studies reviewedA total of eighteen studies from Portuguese centers were identified, of which fourteen were full texts and four were conference articles, published between 1998 and 2020. Fifteen studies included both medical and surgical interventions for patients and three studies were exclusively surgical series. For the purpose of analysis, medical and surgical series will be discussed separately.
Most studies were from hospitals in the Lisbon area (eight studies), Oporto (five studies) and Coimbra (two studies). More than half of the included centers had an on-site cardiac surgery department available (61%).
Patients were enrolled from the cardiology department (eight studies), from internal medicine department (five studies), internal medicine and cardiology (two studies), cardiology and cardiac surgery (one study) and cardiac surgery (two studies).
All studies were retrospective and cohort-based and only one was multicenter.16 The number of years of analysis varied from two to 14 (mean 8.8 years). The sample size ranged from 25 to 320 patients, and a total of 1872 patients were included. All studies used the Duke's criteria or modified Duke's criteria for case selection.
All 18 studies reported short-term mortality and only five studies addressed long-term mortality (Table 3).
Eleven studies reported partial/complete information on intrahospital complications of IE.
The quality of the studies was variable, ranging from 36 to 91% of items on the checklist and no study met all the criteria from the STROBE list.
We discuss “Medical Series” and “Surgical Series” separately.
Results for medical seriesPatients demographics and characteristics
The 15 medical series studies included 1279 patients (Table 4). The mean age of patients was 55.5±12.1 years. The male gender predominated in all studies, a mean of 72.2% (from 62.1 to 82.1%).
Population characteristics of the total cohort and the medical series of patients with infective endocarditis hospitalized in Portugal.
| Total sample (n=1872)Estimate (CI 95%) | Medical series (n=1279)Estimate (CI 95%) | |
|---|---|---|
| Age (years) | 57.1 (50.9-63.3) | 55.5 (48.2-32.8) |
| Male gender (%) | 72.3 (69.7-74.9) | 72.2 (69.0-75.5) |
| Comorbidities (%) | ||
| Structural heart disease | 44.5 (29.3-59.7) | 44.5 (29.3-59.7) |
| IV drug user | 20.4 (5.5-35.3) | 23.5 (6.2-40.8) |
| Previous IE | 9.6 (4.9-14.3) | 10.6 (5.6-15.6) |
| CKD | 8.9 (5.1-12.9) | 8.2 (2.1-14.,2) |
| Diabetes mellitus | 22.8 (17.0-28.6) | 22.0 (13.5-30.,6) |
| Source of infection (%) | ||
| Community acquired IE | 69.2 (60.1-78.3) | 69.3 (57.2-81.3) |
| Health care acquired IE | 27.4 (17.4-37.4) | 27.1 (13.8-40.3) |
| Type of valve (%) | ||
| Native | 69.2 (63.1-75.2) | 68.6 (61.0-76.2) |
| Prosthetic | 22.6 (17.7-28.4) | 22.6 (15.8-29.4) |
| Device related IE | 6.0 (1.6-10.4) | 6.1 (0.8-11.4) |
| Microbiology (%) | ||
| Positive BC | 74.6 (69.6-79.5) | 73 (68.3-77.8) |
| Staphylococcus | 36.6 (27.3-45.8) | 37.9 (26.3-49.6) |
| Streptococcus | 26.6 (18.5-34.8) | 28.4 (17.7-39.0) |
| Enterococcus | 10.2 (6.7-13.8) | 8.4 (3.0-13.9) |
| Complications (%) | ||
| HF | 41.4 (26.3-56.5) | 44.7 (33.8-55.6) |
| Uinf | 19.7 (2.1-37.3) | 17.2 (-7.2-41.7) |
| Emboliz | 24.6 (16.9-32.4) | 26.6 (15.8-37.4) |
| AKD | 35.9 (-2.9-74.8) | 57.1 (43.1-71.1) |
| Surgery (%) | 41.4 (27.1-55.9) | 29.8 (23.2-36.4) |
| Short term mortality (%) | 20.8 (16.5-25.0) | 21.9 (17.1-26.8) |
| Long term mortality (%) | 32.2 (28.8-35.7) | 32.3 (28.8-35.7) |
AKF: acute kidney failure; BC: blood culture; Emboliz: embolization; HF: heart failure; UInf: uncontrolled infection.
The source of IE was predominantly community-related (56-79%) – this classification was obtained in five studies.17–21
Native valves were more predominantly involved (average 68.6%), followed by prosthetic valves (22.6%) and finally CDRIE (6.1%). Seven studies identified the location of IE, and the left cardiac valves were most commonly affected, except in two studies22,23 from late 1990s, in which tricuspid valve IE was more relevant, as the population presented a high prevalence of IV drug use (68 and 72% respectively). Multivalvular involvement was mentioned in three series, from 1.5% in Proença's series23 to 15% and 25% in more recent series, from Santos et al.17 in 2014 and Melo et al.24 in 2017.
Clinical and microbiology featuresFever and constitutional symptoms were the most frequent presentation symptoms reported.
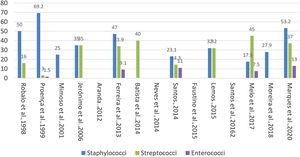
Blood cultures were positive in 73% of the patients, with proportion varying among studies (56-79%). Staphylococcus and streptococcus were the most frequent pathogens in our analysis (Figure 2).
Five studies16,17,21,23,24 reported the presence of enterococcus, in proportions ranging from 1.5 to 13%.
Imaging techniquesIn all 15 series reviewed, echocardiography was the mainstay imaging technique used in patients diagnosed with IE in Portuguese hospitals. Marques et al.21 mentioned the use of 18F-FDG PET/CT to assess one patient who had undergone a prosthetic valve implantation in the previous year.
In-hospital complicationsEight studies (53%) reported partial/complete information about in-hospital complications (Table 3 and Table 4). HF was present at admission or during hospitalization in 44.7%, whereas uncontrolled infection was reported in 17.2%. In addition, 15 to 55% of the patients had an embolic event during hospitalization. Acute kidney failure was very prevalent, affecting more than 50% of patients (from 56 to 58%).
Regarding valve complications, vegetations were the most prevalent major echo finding (48.5 to 93%).
TreatmentIn-hospital, parenteral (IV) antibiotic administration was referred in all series. Neves et al.25 presented the only series with completion of the parenteral antibiotic regimen in an outpatient setting (in 52% of the patients in their series). No specific data was provided in the different series regarding the type of antibiotic and duration of administration. Also, no information regarding the choice of the antibiotics used was given (e.g. national or international guidelines, intrahospital or department protocols).
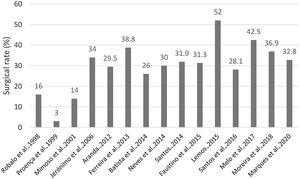
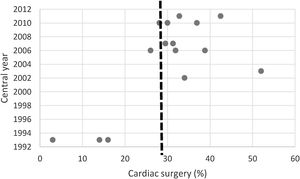
Regarding valve surgery, the presented data was very distinct. The surgical rate in all 15 series varied between 3.1 and 52%, with an average of 29.8% (Figure 3). Nevertheless, the more recent series reveal a tendency toward a higher surgical rate (Figure 4). Analyzing the surgical rate taking into account the presence of a cardiac surgery unit (CCT) in the hospital center, a non-significant a higher rate was observed in the centers that had an on-site CCT[35 (CI 95%: 28.7-41.6)% vs. 23(95% CI: 11.3-26.1)%].
The indication for surgical intervention, was fully specified in two studies,21,26 HF was predominant (50 and 74%), followed by uncontrolled infection (27.3 and 46.8%) and embolization (13.6 and 15.6%). Cardiac surgery was considered a protective factor for patients with a clinical surgical indication.16,21,26
Regarding the reasons for not performing surgery, Marques et al.21 highlighted the presence of significant comorbidities, cognitive impairment and ischemic stroke with significant sequelae as impeding factors.
Timing of surgery was only addressed by Moreira et al.,26 concluding for their series that the timing of surgery (early versus late) was not associated with increased mortality. No information on the culture of surgical material was provided.
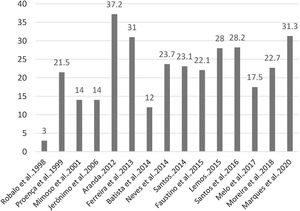
MortalityAll studies reported short-term mortality, with an average of 21.9% (ranging from 3 to 37.2%) (Figure 5 and Table 3).
Only four series evaluated long-term mortality.17,18,20,26 In these four series, more than a third of all patients died within 2 years despite hospitalization, antibiotic and surgical treatment (ranging from 29.1 to 34%) – Table 3.
The cause of death was only specified in two studies,16,21 septic shock being the first cause, followed by HF and embolism with similar rates.
Results for surgical seriesIn this analysis, we review the three surgical series27–29 described in Table 3 and two partial surgical cohorts included in the series validated by Moreira et al.26 and Ferreira et al.16 in their studies (Table 5).
Population characteristics of the surgical cohorts of patients with infective endocarditis hospitalized in Portugal.
| Ferreira et al., 2013 | Alves et al., 2015 | Madeira et al., 2016 | Moreira et al., 2018 | Guiomar et al., 2020 | |
|---|---|---|---|---|---|
| Period | 2000-2011 | 2004-2014 | 2007-2014 | 2006-2014 | 2006-2017 |
| Sample size (n) | 57 | 320 | 128 | 86 | 145 |
| Mean age (years) | NA | 60(49-70) | 60 (47-70) | 59.4±15.3 | 72 (median) |
| Male sex (%) | 69.7 | 75 | 78.2 | 72.4 | |
| Microbiology (%) | |||||
| Positive BC | NA | 81.3 | 67.2 | 67.1 | 95 |
| Staphylococcus | 31.9 | 19 | 32.5 | 45 | |
| Streptococcus | 29.5 | 19 | 15 | 15 | |
| Enterococcus | 13.1 | 11.7 | NA | 15 | |
| Type of IE (%) | |||||
| Native valve | NA | 71.3 | 73.4 | NA | 69.7 |
| Prosthesis | 21.9 | 22.7 | 42.5 | 30.3 | |
| Cardiac device | 6.8 | 3.9 | NA | NA | |
| Valve involvement (%) | |||||
| Aortic valve | 49 | 66.3 | 50 | 64.4 | 54 |
| Mitral Valve | 31.6 | 47.3 | 51.6 | 31 | 45 |
| Aortic and mitral | 17.5 | NA | |||
| Tricuspid | NA | 4.4 | 7.8 | 9.2 | NA |
| Urgency (%) | |||||
| Emergent | 82 | NA | 8.6 | NA | 20 |
| Urgent | NA | 91.4 | NA | 74.5 | |
| Elective | 18 | NA | 0 | NA | 5.6 |
| Reasons for surgery (%) | |||||
| Heart failure | 100 | 36.2 | 74.2 | 50 | 57.9 |
| Uncontrolled infection | NA | 6 | 50 | 46.8 | 31 |
| Embolization | 26.8 | 16.4 | 15.6 | 11 | |
| Post-op complications (%) | |||||
| Acute kidney failure | NA | 19 | NA | NA | 16.6 |
| Atrial fibrillation | NA | 8.3 | |||
| Respiratory infection | NA | 4.8 | |||
| Sepsis | 8 | 6.9 | |||
| Respiratory failure | 10.2 | 5.6 | |||
| Ischemic stroke | 14 | 6 | NA | 20.8 | 2.1 |
| Mortality (%) | |||||
| Short term mortality | 14 | 15.3 | 16 | 15.5 | 13.1 |
| Long term mortality | NA | NA | NA | 33 | NA |
BC: blood culture; IE: infective endocarditis:not available.
A total of 736 patients, mostly men, in their sixth decade of life were identified.
A higher prevalence of native valve endocarditis was included (aortic valve prevailed, except in the Madeira et al.28 cohort with a similar rate in the mitral valve). Right heart valves, namely tricuspid valve, were rarely subject to intervention. Multivalvular involvement and intervention were not disclosed.
Regarding causal agents, staphylococcus spp. ranged from 19 to 45%, followed by streptococcus spp. (15 to 29.5% of patients); most patients had positive blood cultures. Enterococcus was present in 11.7 to 15% of patients. No information on microbiology and molecular testing of operative specimens or post-operative antibiotic regimen and duration was provided.
Surgery was considered emergent/urgent in the majority of cases. Two centers reported having performed elective surgeries (5.6% in Guiomar et al. series29 and 18% in Ferreira et al. cohort16); Madeira et al.28 on the other hand did not perform elective surgeries in their cohort.
All centers followed the scientific guidelines on indication for surgery, the first indication being refractory HF, followed by uncontrolled infection and embolization risk. Length of hospitalization was on average approximately four weeks (disclosed in two series).16,29 Surgical time or aortic cross-clamping times, on the other hand, was not addressed.
As for the major outcomes, post-operative complications were partially disclosed in three series,26,27,29 acute renal and respiratory failure, as well as sepsis, arrhythmias and ischemic stroke were identified. Short term mortality rate ranged from 13.1 and 16% in all five series. Guiomar et al.29 specified septic and cardiogenic shock as the main causes of death. Long-term mortality rate was only addressed by Moreira et al.26 with up to one third of patients dying after one year and up to 43% at five years of follow-up.
An analysis according to subgroups of patients hospitalized before and after 2009 (taking into consideration the different recommendations on surgical intervention in IE3) is only available in the Alves et al. study,27 concluding that the more recent group presented older patients, with less heart failure (HF) and a higher rate of embolization and enterococcus spp. infection.
DiscussionOur main purpose was to review and describe the best evidence available on the epidemiology of patients hospitalized due to IE in Portuguese hospital centers. Despite a paucity of multicenter prospective data, we were able to identify eighteen retrospective case series from different geographical areas, in different hospital settings (community vs. university vs. central tertiary hospital; cardiology vs. surgical vs. internal medicine department) and at different time periods. No data on the incidence of IE in the Portuguese population is known and this analysis could not provide such data. Nevertheless, we believe that this study can reveal important aspects regarding the epidemiology of this complex disease in Portugal.
In our analysis, older males were more frequently affected, which is in accordance with larger prospective international registries.4,6,9,30,31Staphylococcus, followed by streptococcus were the most prevalent pathogens, but enterococcus had a major presence in eight series, which corroborates other series.4,9 In fact, the burden of Enterococcus IE is increasing, which may be related to the diagnosis of IE in older patients,32 as is the case in this population. Nevertheless, staphylococcus and enterococcus IE carry a high mortality rate,33–35 since these are highly locally destructive with a high capacity to embolize, with a significant impact on treatment and prognosis and these results in Portuguese centers should be taken into consideration.
Left heart valves were generally more affected, with the aortic valve being more frequently involved and subject to surgical intervention. The pulmonary valve was rarely mentioned and the only series that had a significant incidence of tricuspid valve involvement were the ones with a high rate of IV drug users. Multivalvular endocarditis rate, normally synonymous of a more severe infectious process,36 was assessed at 18% by Kim et al.37 in a 77 patient non-surgical series; a similar rate was found in the recent EURO-Endo registry.4 Few centers in Portugal have disclosed multivalvular involvement in IE patients which limits our understanding.
The use of modified Duke criteria3 mainly through the presence of positive blood cultures (up to 82% in medical series and 95% in Gaia's surgical center) and echocardiographic imaging compatible with infection (predominantly vegetations) were the mainstay for the diagnosis of IE in Portuguese patients. The use of the imaging techniques such as PET/CT10,38–40 (used in 16.6% of patients in the recent Euro-Endo registry4) was only disclosed in one of the analyzed series, probably as a result of lack of availability and cost, as well as due to the inclusion of patients from before the 2015 ESC guidelines.38 This was when these new imaging tools were included in the diagnostic and prognostic stratification for the first time.
Regarding antibiotic treatment, the general experience consists of full intrahospital IV regimen, as only one national series25 reported the use of outpatient parenteral antibiotic therapy (OPAT) for completion of medical therapy. In stable IE patients, after two weeks of intrahospital antibiotic regimen, OPAT has been shown to be safe38,41 and probably will be used with increasing frequency in our clinical practice in the future, reducing the length of hospitalization and, consequently, cost.
The rate of surgery in nonsurgical series was in general inferior to patterns observed in international series,4,6,30,33 which may be explained by the inclusion of patients from before the 2009 and 2015 ESC Guidelines, probably some resistance to operate when the surgical risk is prohibitive, taking into account the patient's physical and mental status, neurologic sequelae and other comorbidities13 (as was also reflected in the Marques21 series), as well as patient refusal.4 Nevertheless, surgery was in fact identified as a protective factor by three Portuguese series. Also, surgical indication is by itself an important prognosis factor in IE patients,42 and may not always be recognized by the assisting physician,43 highlighting the need for the definition of referral centers with high volume experience and multidisciplinary teams, namely Endocarditis teams44 that can manage complex cases and help define institutional and inter hospital cooperation strategies, with the objective of improving prognosis.
When analyzing Portuguese surgical series, demographics, type of IE and valve involvement in general overlap with the general trends of described Portuguese nonsurgical series and international surgical series.45–48 Clinical indications for surgery agreed with scientific international orientations. Emergent or urgent indication was the pattern in Portuguese centers with surgeries on an elective basis being performed occasionally, with rates well below the recent published Euro-endo registry4 or other surgical series.46,47 The main outcome highlighted in all series was short-term mortality, which was in general slightly higher than in other series reported in the USA,46 Switzerland49 or Greece.47 Nevertheless, international surgical series report intrahospital mortality rates that vary from 6.8 to 28.8%, described in a metanalysis of Barca el al.36 Several clinical and technical aspects were omitted or were superficially approached in the Portuguese surgical studies that could be important to explain the final outcomes of IE patients who undergo surgery
A significant percentage of intrahospital complications and short and long mortality in nonsurgical series was evident in this descriptive analysis. The data do not allow for predictors of outcome analysis or temporal trend analysis, but a dismal prognosis is evident as general short-term mortality was registered as being on average 21% (reported as high as 37%), which is slightly higher than the ones registered by the ICE study,50 EURO-ENDO4 and Euro Heart Survey.6 In spite of less data being available, mortality up to two years was approximately a third of the complete population assessed, confirming that despite all the progress towards a faster diagnosis and improved surgical and intensive care, endocarditis is in fact a lethal disease.51,52
LimitationsThis was a systematic review of mainly single institution series and therefore selection bias may be present as the studies may well not fully represent the entire population. Also, despite exclusion of very small series, the majority of series had a small to moderate number of patients which could lead to reporting bias. Most series were retrospective, purely observational, which led to differences in reporting epidemiological, clinical and technical data and measure outcomes. The significant heterogeneity of the number of patients, hospital settings and the time of the analyzed series also prevented the use of more complex statistical analyses. In particular, most series reported on patients included both before and after the 2009 ESC Guidelines on Infective Endocarditis,3 and for this reason we could not perform a comparative before-after analysis.
Regarding the quality of studies, most had up to 75% on the STROBE checklist which may indicate risk of bias.
ConclusionAs far as we are aware, this is the first systematic review of Portuguese IE case series. Epidemiological data favors a higher incidence of IE in older male patients, with a predominance of staphylococcus and streptococcus species, an apparent high rate of intrahospital complications and lower than expected surgical rate. Access to cardiac surgery for those who had an indication remains an undetermined fact in our country, as only single center individual series addressed this matter. And the prognosis for IE in Portugal remains inadequate even in the more recent hospital series.
The available data supports the need for a multicenter prospective data assessment on the epidemiology and health outcomes of patients with IE in Portugal to address these and other questions, with the purpose of improving the overall prognosis of this complex disease.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors want to thank Dr. Ana Batista (Centro Hospitalar Vila Real), Dr. Anabela Raimundo (Hospital Luz Lisboa), Dr. Ines Cruz (Hospital Garcia Orta) and Dr. Mariana Faustino (Hospital Fernando Fonseca), for their willingness to provide extra information for this analysis and Dr. Susana Oliveira Henriques (Lisbon School of Medicine – Center for Information and Documentation) for her important advice regarding search strategy and referencing.