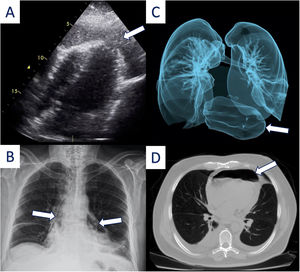
We present the case of a 64-year-old male with a past medical history of diabetes, hypertension and esophageal myotomy for esophageal diverticulum four months ago. He underwent a Nissen fundoplication due to diverticulum recurrence. On his second post-operatory day, he presented chest pain and fever associated with a lower respiratory tract infection treated with levofloxacin. A routine esophagogram, performed four days postoperatively, demonstrated no leakages (video S1). On his seventh postoperative day, he reported an intense stabbing chest pain; a bedside transthoracic echocardiogram demonstrated small air bubbles swirling in the pericardial space suggestive of pneumopericardium (Figure 1A and video S2). On the chest X-ray, a radiolucent space along the left and right borders of the heart confirmed the presence of air in the pericardial sac (Figure 1B). A subsequent chest tomography and three-dimensional reconstruction of the airway revealed the presence of a large bubble of air in the pericardium (Figure 1C and D). The patient quickly deteriorated presenting hypotension and shock nonresponsive to vasoactive agents. He underwent an emergent pericardial window improving his clinical status. As a surgical finding, an esophageal-pericardial fistula was found. This was later confirmed with methylene blue, given orally and then appearing in the drainage tube. A subsequent surgical intervention for fistula repair using a serosal patch took place. Thereafter, the patient's circumstances were complicated by purulent mediastinitis. He was treated with broad spectrum antibiotics and surgical debridement. Unfortunately, the patient died after two months of medical efforts.
(A) Transthoracic echocardiogram showing air bubles swirling in the pericardial space (arrow). (B) Chest X ray demostrating air along the left and right borders of the heart (arrows). (C) Three-dimensional reconstruction of the airway and (D) chest tomography showing a big buble of air in the mediastinum (arrow).
The authors have no conflicts of interest to declare.