Permanent junctional reciprocating tachycardia (PJRT) is an uncommon form of atrioventricular reentrant tachycardia due to an accessory pathway characterized by slow and decremental retrograde conduction. The majority of accessory pathways in PJRT are located in the posteroseptal zone. Few cases of atypical location have been described. We report a case of PJRT in a 72-year-old woman in whom the accessory pathway was located in the left lateral region and treated by radiofrequency catheter ablation.
A forma permanente de taquicardia juncional reciprocante é uma modalidade incomum de taquicardia auriculoventricular reentrante devida a via de acesso caracterizada por condução retrógada lenta e gradual. A maioria das vias acessórias na forma permanente da taquicardia juncional reciprocante está localizada na zona posterosseptal. Foram apresentados poucos casos de localização atípica1-4. Apresentamos o caso de forma permanente da taquicardia junctional reciprocante numa mulher de 72 anos na qual a via acessória foi colocada na região lateral esquerda sendo a ablação efetuada por cateter de radiofrequência.
Permanent junctional reciprocating tachycardia (PJRT) is an uncommon form of atrioventricular (AV) reentrant tachycardia due to the presence of an accessory pathway (AP) characterized by slow and decremental retrograde conduction, and usually occurs in children and young adults. The hallmark ECG feature is an incessant narrow complex tachycardia with inverted P waves in leads II, III and aVF, as well as the left lateral leads, and an RP interval longer than the PR interval. Although most APs in PJRT are located in the posteroseptal zone, other locations have been described. It should be noted that this tachycardia is generally incessant and slower than common supraventricular tachycardias, hence correct diagnosis is very important due to the inherent risk of left ventricular dysfunction secondary to tachycardiomyopathy.
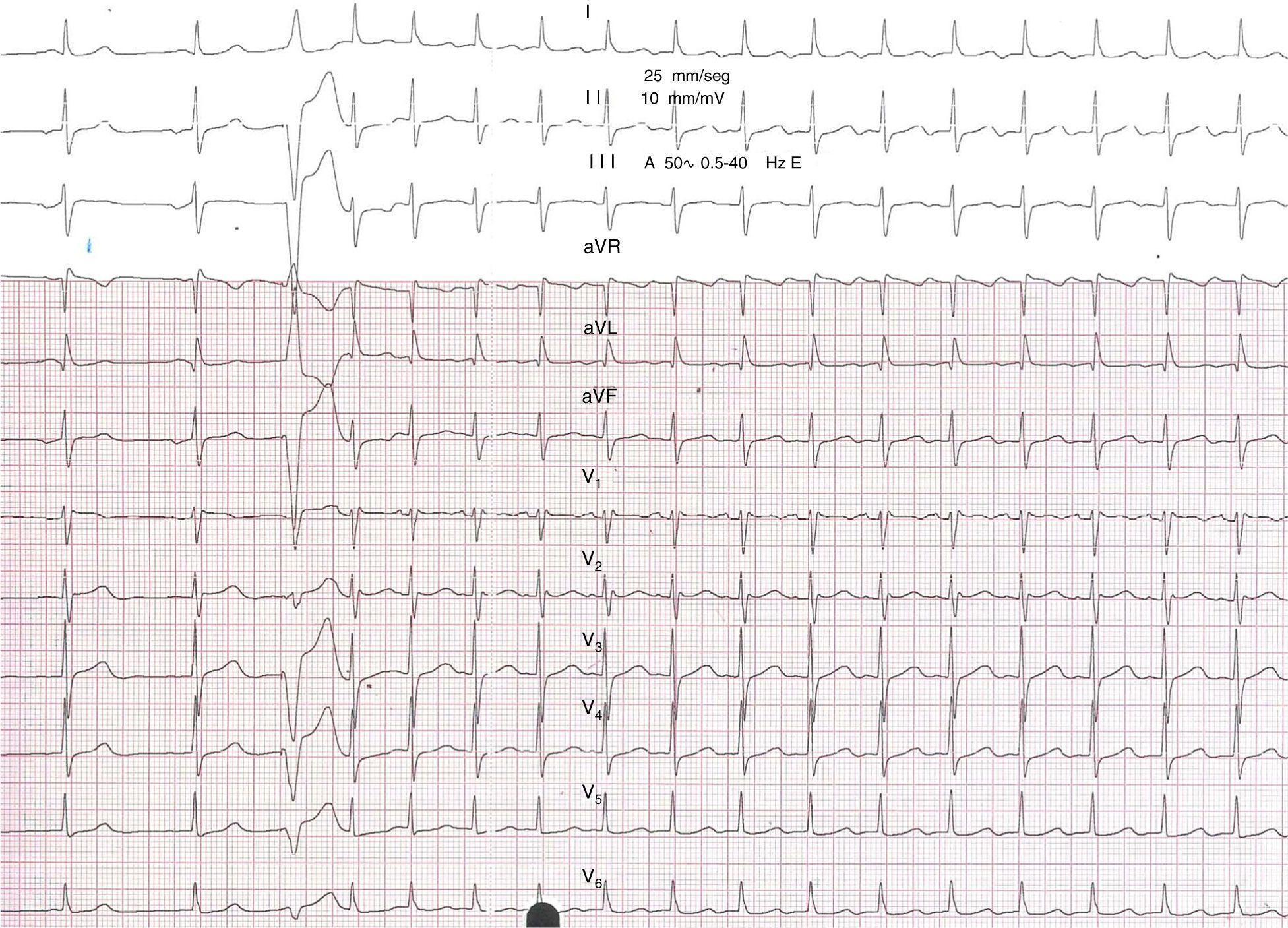
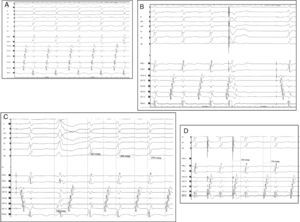
Case reportA 72-year-old woman with a history of frequent episodes of palpitations since childhood had been diagnosed as having ‘bradycardia-tachycardia syndrome’ (sick sinus syndrome) followed by pacemaker implantation five years previously. She complained of dyspnea with minimal exertion and permanent fast heart rate. The patient stated that she had actually felt worse since the pacemaker implantation. During the pacemaker interrogation repetitive induction of a narrow QRS tachycardia was seen during measurement of the ventricular threshold, with a single extra beat (Figure 1). The ECG showed a narrow QRS tachycardia of 125 bpm, negative P waves in the inferior leads, I and aVL, positive in V1, and long RP intervals. Moreover, multiple episodes of incessant narrow QRS tachycardia were also documented by the pacemaker, frequently initiated after a pacing beat. The echocardiogram showed impaired left ventricular ejection fraction. With the suspicion of tachycardiomyopathy (the percentage of ventricular pacing was less than 1%, ruling out right ventricular apical pacing-related heart failure), the patient was referred for electrophysiology study.
12-lead ECG obtained during sinus rhythm, showing a normal PR interval with no delta waves. Tachycardia is then induced with a single extra beat from the right ventricular apex, exhibiting narrow QRS complexes, long RP intervals, and inverted P waves in the inferior leads, I and aVL and positive in V1.
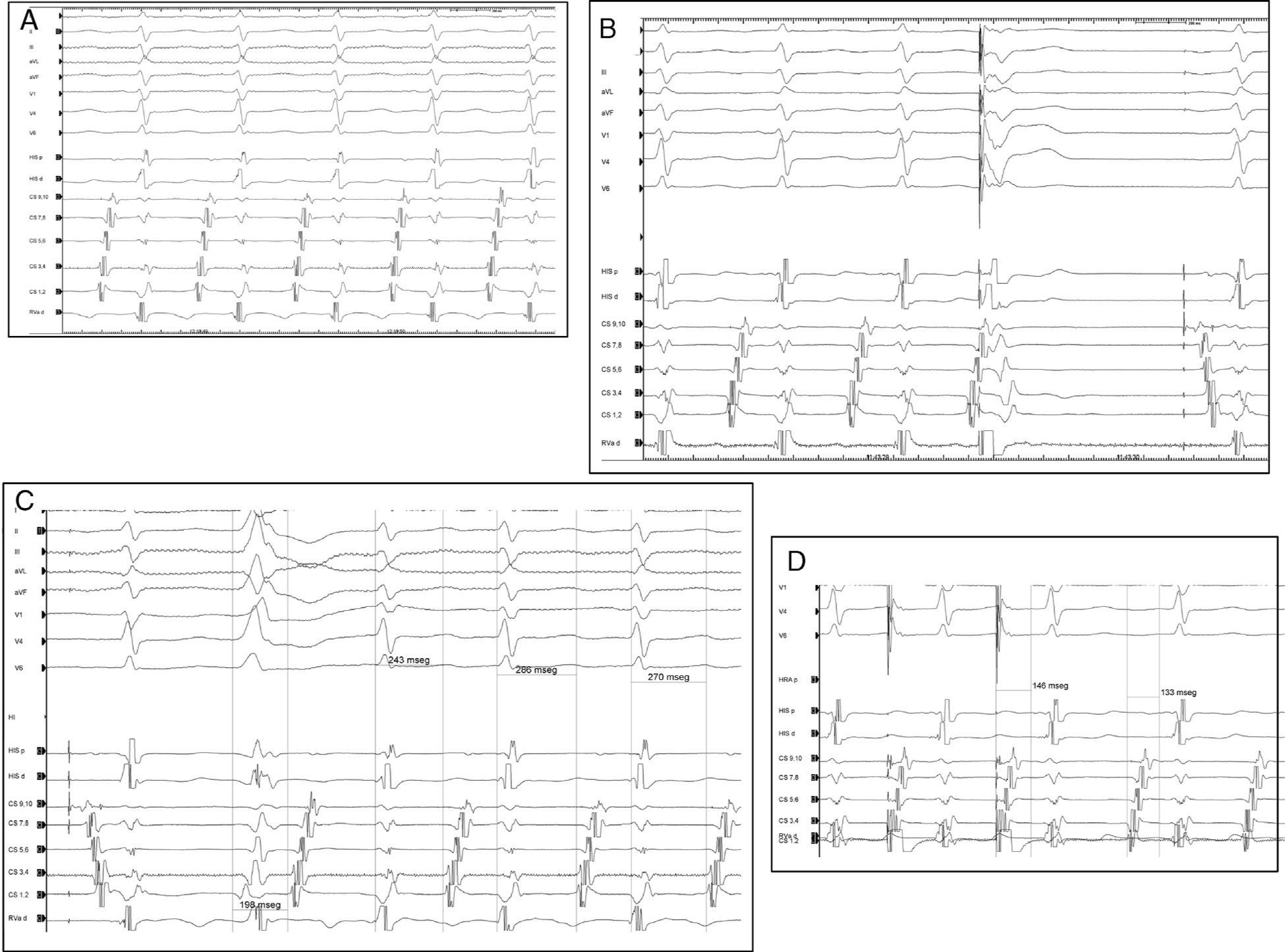
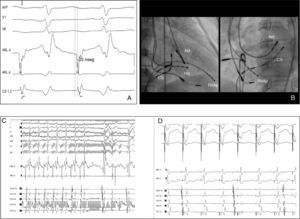
After written informed consent was obtained, the ablation procedure was performed under deep sedation in a fasting and drug-free state. The patient had been in incessant tachycardia since her arrival in the electrophysiology laboratory. Three standard diagnostic catheters were introduced via the femoral veins and placed in the His bundle, right ventricle and coronary sinus. Long RP tachycardia was confirmed (Figure 2A), with a distal to proximal atrial activation sequence in the coronary sinus (CS) (earliest atrial activation being located at the distal electrode pair of the CS catheter), 1:1 AV relationship, AV interval of 270 ms, HH changes preceding and predicting AA changes, and spontaneous termination of the tachycardia ending with ventricular activation. The tachycardia was also inducible by atrial pacing and single ventricular premature beats (VPBs) (Figure 1). Moreover, the tachycardia could not be entrained since it was repeatedly interrupted by continuous ventricular pacing. Tachycardia onset was not preceded by AH prolongation and notably, the ΔAH (difference between atrial pacing AH near tachycardia cycle length and supraventricular tachycardia AH) was 13 ms, ruling out AV nodal reentrant tachycardia with left-sided extension.5 Atrial activation was excluded by showing termination of the tachycardia with a single His-refractory VPB (Figure 2B) without atrial depolarization and fused VPBs, ruling in atrioventricular reciprocating tachycardia mediated by a left lateral AP. Furthermore, the atrial activation sequence during tachycardia was identical to that of right ventricular pacing. The retrograde AP conduction was slow and decremental (Figure 2D). With this information, a diagnosis was made of PJRT due to an AP with retrograde, slow, and decremental conduction properties, located in the left lateral region.
(A) Surface ECG (aVF, V1 and V6) and intracardiac bipolar recordings during tachycardia. A supraventricular tachycardia with a long RP interval and earliest atrial activation along the mitral annulus (CS1–2) is seen; (B) ventricular extrastimuli at shorter coupling intervals from the right ventricle at a time when the His bundle is known to refractorily terminate the tachycardia without reaching the atrium; (C) the tachycardia is induced with a single premature beat from the left ventricle, showing slow and decremental conduction properties. Abl: ablation; CS: coronary sinus (1–2 distal; 9–10 proximal); His p: proximal His; His d: distal His; RVAp: right ventricular apex.
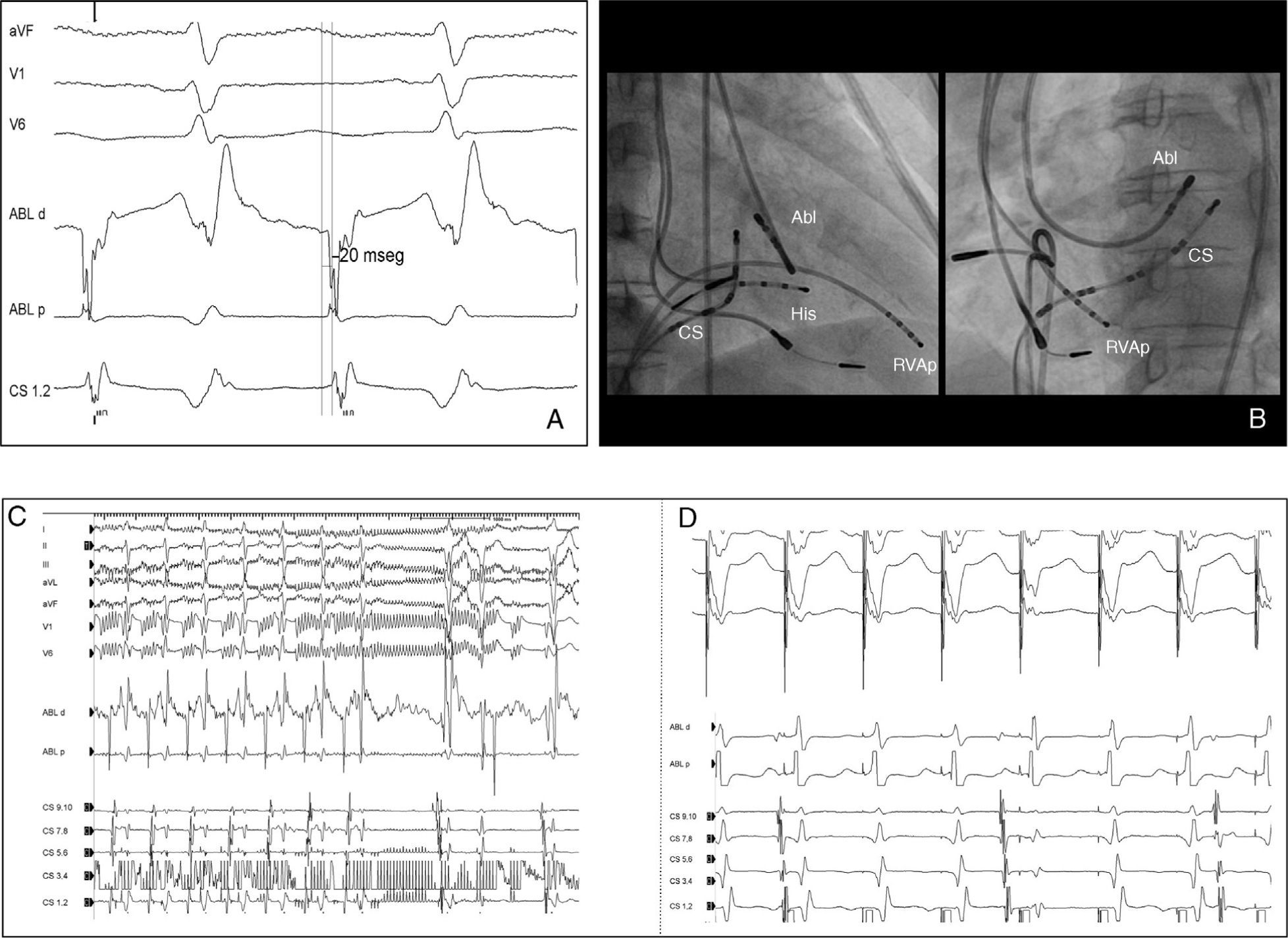
Via a retrograde approach, careful mapping of the mitral annulus showed an early atrial activation site (15 ms before P-wave onset and 20 ms before CS1–2) in the lateral region. The ablation catheter electrogram showed an A/V ratio >2 (Figure 3A). Conventional radiofrequency (RF) application at this site (55°C, 45 W) terminated the tachycardia (within four seconds) with a retrograde block over the AP. After RF ablation the tachycardia was no longer inducible and normal AV node conduction was preserved but without retrograde conduction. No recurrence was observed over six-month follow-up (no events on pacemaker interrogation) and left ventricular ejection fraction increased to normal values.
(A) Successful ablation site. The ablation catheter electrogram during tachycardia showed early atrial activation preceding P-wave onset by 15–20 ms, A/V ratio >2; (B) radiograms obtained in right anterior oblique (30°) and left anterior oblique (45°) projections showing the successful ablation site in the left lateral region at the mitral annulus; (C) the tachycardia was terminated within four seconds of radiofrequency application; (D) absence of ventriculoatrial conduction after ablation. Abbreviations as for Figure 2.
Differential diagnosis of long RP tachycardias includes PJRT, atypical AV nodal reentrant tachycardia and atrial tachycardia. AV nodal reentrant tachycardia usually initiates after a premature beat depending on a critical AH prolongation; also possible, although rare, is a distal to proximal activation sequence, as seen in the present case. Atrial tachycardia was excluded by reproducible tachycardia termination delivering a single VPB without atrial capture and by the fact that the atrial activation sequence during tachycardia was identical to that of right ventricular pacing, confirming retrograde conduction over an AP.
In most cases of PJRT the AP is located in the right posteroseptal region around or just within the coronary sinus ostium, but other atypical locations have been reported.1–4 For instance, various regions of the mitral or tricuspid annuli, except the right posteroseptal region, have been identified in 10% of patients.3 Among these locations, the right anterior septum and left posteroseptal regions are seen more frequently. There is no report in the literature of PJRT in an adult patient due to a left lateral AP. One theory for the decremental properties and long conduction times of the PJRT pathway is that the fibers may have a tortuous course as they cross the AV sulcus.3
PJRT is highly refractory to antiarrhythmic drug therapy, because conduction intervals may be prolonged without creating a conduction block in either the antegrade AV node or the retrograde AP, thus failing to control the tachycardia.4 It may also lead to tachycardia-induced cardiomyopathy in some patients, as in the case presented. For these reasons, RF catheter ablation is considered the treatment of choice in PJRT. Ablation procedures for PJRT must involve careful mapping of both AV grooves, looking for the point of earliest atrial activation and, if possible, an AP potential contiguous with the atrial electrogram.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.