A 48-year-old woman with no significant cardiovascular history presented to the hospital with a chief complaint of acute chest pain, without radiation, associated with an episode of blurred vision. The physical examination was remarkable for a systolic blood pressure differential in the upper limbs (left 129/43 mmHg, right 40/20 mmHg), absence of right radial and brachial pulses, and a holodiastolic aortic murmur.
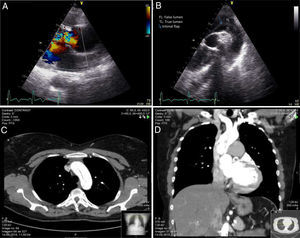
The electrocardiogram revealed left ventricular hypertrophy. Emergent transthoracic echocardiography in left parasternal view showed dilatation of the thoracic ascending aorta (43 mm) and a bicuspid aortic valve, with severe regurgitation due to prolapse of the cusps (Figure 1A). In the suprasternal window, at the level of the aortic arch, an intimal flap with supravalvar origin and extension to the aortic arch, descending thoracic and abdominal aorta was clearly evident (Figure 1B, Videos 1 and 2). Biventricular systolic function was normal and there was no pericardial effusion. Subsequently, cardiac computed tomography confirmed the presence of a Stanford type A aortic dissection (Figure 1C and D). The patient was referred for emergent cardiac surgery. At three months of follow-up, she was asymptomatic, with no signs of target organ damage.
(A) Severe aortic regurgitation due to a prolapse of the cusps; (B) suprasternal view, at the level of the aortic arch, showing an intimal flap (blue arrow) with supravalvar origin and extension to the aortic arch; (C and D) cardiac computed tomography confirming the presence of a Stanford type A aortic dissection. FL: false lumen; TL: true lumen.
Aortic dissection is an uncommon but potentially fatal condition. The accessibility and diagnostic ability of bedside echocardiography enabled the rapid detection and prompt treatment of this condition, contributing to the good end result.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.