Sex differences among patients with acute myocardial infarctions remain a matter of debate. Inequalities in presentation, diagnosis, treatment, and prognosis are frequently observed, contributing to a worse prognosis in women. The aim of this study was to investigate sex-related differences in Portuguese ST-segment elevation myocardial infarction (STEMI) patients.
MethodsThe authors conducted a retrospective analysis of STEMI patients included in the Portuguese Registry on Acute Coronary Syndromes, between October 2010 and 2022. The two co-primary endpoints were in-hospital and one-year mortality.
ResultsA total of 14470 STEMI patients were studied. Women were underrepresented with 3721 individuals (25.7%). They were significantly older (70 vs. 62 years, p<0.001), with higher prevalence of cardiovascular risk factors, and underwent less frequently coronary angiography (84.4% vs. 88.5%, p<0.001) and guideline-directed medical therapy (e.g., aspirin 92.5% vs. 95.4%, beta blockers 79.2% vs. 83%, p<0.001). Furthermore, they experienced more complications, such as congestive heart failure (23.4% vs. 14.6%), ischemic stroke (47% vs. 40%), and in-hospital mortality (8.5% vs. 4.1%) (p<0.001 for all comparisons). Similarly, they presented higher one-year mortality (11.5% vs. 6.3%, p<0.001). However, after a multivariate analysis testing significant clinical variables, female sex remained an independent predictor for in-hospital (odds ratio=1.633; 95% CI [1.065–2.504]; p=0.025), but not for one-year mortality.
ConclusionsThis analysis reveals sex-related disparities in Portuguese STEMI patients. Despite limitations inherent to registry-based analysis, women were significantly older, with increased cardiovascular risk, less treated, and with higher in-hospital mortality. These disparities should be a concern for clinicians to further improve outcomes and move toward equitable medical care.
As diferenças entre sexos nos doentes com enfarte agudo do miocárdio (EAM) são um tópico controverso. São frequentemente descritas disparidades na apresentação, no diagnóstico e no tratamento, as quais contribuem para um pior prognóstico nas mulheres. O objeto desta análise foi determinar estas diferenças no EAM com supradesnivelamento do segmento ST (STEMI).
MétodosOs autores realizaram uma análise retrospetiva de doentes com STEMI incluídos no Registo Português de Síndromes Coronárias Agudas, entre outubro de 2010 e 2022. Foram definidos dois endopoints primários: mortalidade intra-hospitalar e mortalidade a um ano.
ResultadosForam incluídos 14 470 STEMI. O sexo feminino estava sub-representado (3.721 doentes, 25,7%). As mulheres tinham uma idade superior (70 versus 62 anos, p < 0,001), com maior prevalência de fatores de risco cardiovascular, sendo menos submetidas a angiografia coronária (84,4% versus 88,5%, p < 0,001) e a terapêutica médica (aspirina 92,5% versus 95,4%, beta bloqueantes 79,2% versus 83%, p < 0,001). O sexo feminino apresentou mais complicações: insuficiência cardíaca congestiva (23,4% versus 14,6%), acidente vascular cerebral isquémico (47 versus 40%), e mortalidade intra-hospitalar (8,5% versus 4,1%) (p < 0,001 para todas as comparações). A mortalidade a um ano foi superior nas mulheres (11,5% versus 6,3, p < 0,001). Após análise multivariada, o sexo feminino manteve-se preditor independente de mortalidade intra-hospitalar (OR = 1,633; CI 95% [1,065-2,504]; p = 0,.025), mas não a um ano.
ConclusãoO presente estudo, em Portugal, revela múltiplas diferenças entre sexos no STEMI. Apesar das limitações inerentes às análises baseadas em registos nacionais, as mulheres têm idade e risco cardiovascular superior, sendo menos tratadas, com mortalidade superior. Estas desigualdades devem ser uma preocupação para a comunidade médica de modo a melhorar outcomes e a proporcionar cuidados médicos equitativos.
Although there has been significant improvement in healthcare1,2 and a decrease in mortality,1,3–5 cardiovascular diseases, with the significant weight of myocardial infarction, continue to be the most common cause of death in Europe1,6–8; and their burden is increasing in women.5,9 Improved healthcare is mainly based on three factors: the implementation and dissemination of coronary reperfusion,3 better myocardial revascularization techniques10 and the widespread application of guideline-directed medical therapy.3
Around 30–40% of acute myocardial infarctions (AMI) occur in women; ST-segment myocardial infarction (STEMI) is less likely than non-ST-segment myocardial infarction (NSTEMI).4 STEMI is described as increasing exponentially with age in women compared to a linear rate in men.3
Sex differences in AMI are an issue that is continually under debate,11,12 with conflicting results in the literature,1,7,8,10 partly due to the heterogeneity of studied populations, including both STEMI and NSTEMI.1,13 Although comorbidities, complications, and mortality remain higher in women,1 long-term differences appear to attenuate after adjusted analysis.1,6 These differences may be related to worse baseline characteristics,8,14 pathophysiology and treatment disparities4 in women, but they are not fully understood.1,15,16
This matter has raised awareness not only inside the cardiology community with several publications and campaign advertisements,17 but also among the general population.7 Nevertheless, differences still persist.4,17,18
In Portugal, cardiovascular diseases are the most common cause of death. They are the most common etiology in women, in contrast to oncologic diseases in men.19 A previous Portuguese study on acute coronary syndromes (ACS) identified differences in treatment and prognosis between sexes.5 Nevertheless, as of the present date and to the best of the authors’ knowledge, the specific situation in Portugal, particularly regarding STEMI, is not known. The authors consider that including only STEMI could help reduce the heterogeneity of the population and eliminate potential confounding factors associated with the spectrum of ACS, particularly in diagnosis and treatment.
ObjectivesThe purpose of the current analysis is to investigate sex-related differences among patients who have experienced STEMI in Portugal focusing on baseline characteristics, clinical findings, treatment modalities, prognosis and mortality. Based on the literature, the authors expected to find sex-related differences in these patients.
MethodsThe Portuguese Registry on Acute Coronary Syndromes (ProACS) was established in 2002, founded by the Portuguese Society of Cardiology and is coordinated by the National Center for Data Collection in Cardiology. This multicenter, continuous, prospective observational national registry is registered at ClinicalTrials.gov (NCT01642329).20 All Portuguese cardiology departments were invited to participate and consecutively include adult patients who were hospitalized. The inclusion and exclusion criteria were established and published elsewhere.20
By 2016, a total of 49 Portuguese centers had been included (11 university hospitals, 12 hospitals with cardiac surgery and 25 with catheterization laboratories), distributed across Portugal: North (11 centers), Central region (12 centers), South (22 centers) and in the Autonomous Regions of Madeira and the Azores (four centers).20
The authors conducted a retrospective analysis of STEMI patients included in the ProACS between October 2010 and 2022.
Statistical analysisContinuous variables were presented as mean value±standard deviation or median and interquartile range (IQR). These were compared between groups using independent samples t-test or the Mann–Whitney U test, based on their distribution. Categorical variables were presented as frequencies and percentages and were compared using the chi-square or Fisher's exact tests, as appropriate. Separate analyses were made for in-hospital and one-year endpoints.
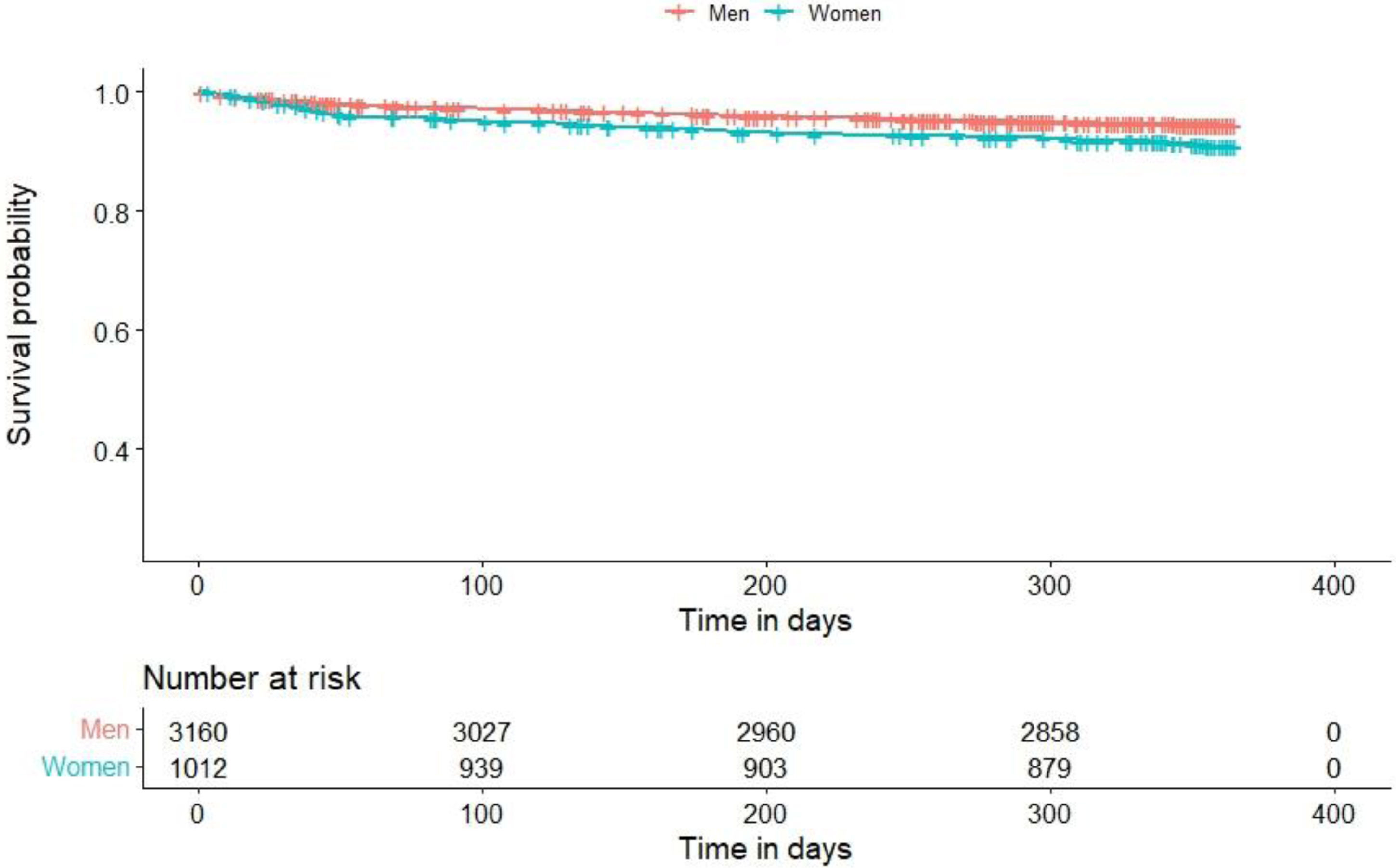
The independent predictors of the primary outcome (in-hospital mortality) were assessed by multivariable logistic regression analyses using the stepwise forward method. The Hosmer–Lemeshow test was used for the calibration of the regression model. The effect of the variables was assessed by estimating the odds ratio (OR) and 95% confidence interval (CI). Survival analysis was assessed using Cox proportional hazard regression, cumulative incidences of events were estimated by the Kaplan–Meier method, and the difference was assessed by the log rank test.
All analyses were performed using SPSS software for Windows, version 29.0®. All p-values were two-sided and were considered significant when <0.05.
Study endpointsTwo cohorts were defined based on sex. Baseline clinical characteristics, in-hospital clinical findings, treatment and outcomes were compared.
The two co-primary endpoints were in-hospital and one-year mortality. Secondary endpoints consisted of in-hospital complications (congestive heart failure, cardiogenic shock, atrial fibrillation, cardiac arrest, atrioventricular block, sustained ventricular tachycardia (SVT), mechanical complications, stroke, reinfarction, and major bleeding), and one-year cardiovascular and non-cardiovascular hospital readmission.
ResultsBetween October 2010 and 2022 a total of 14470 STEMI patients were registered on ProACS.
Baseline characteristicsOut of 14470 STEMI patients, 3721 (25.7%) were female with a mean age of 64±13.5 years – reported in almost the entire population (14465 patients).
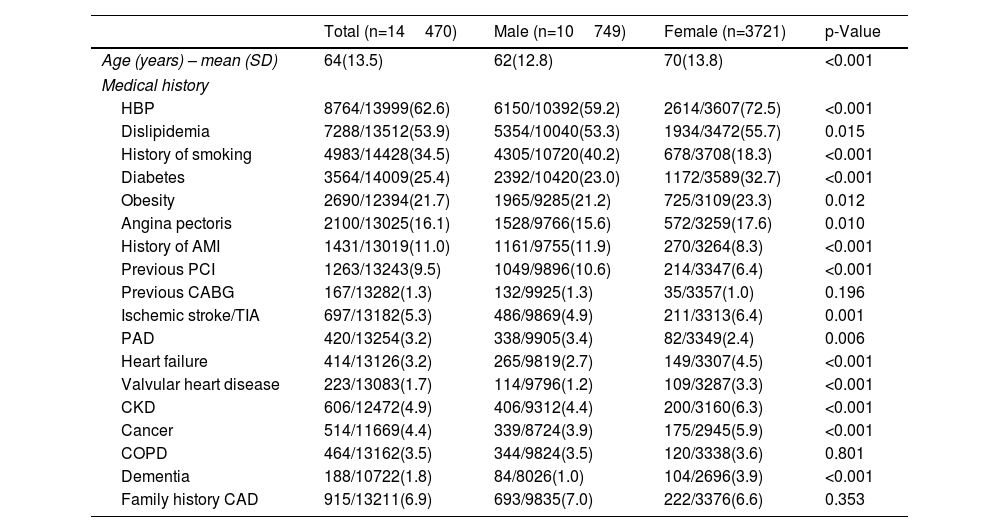
Patient baseline characteristics are shown in Table 1. Women were older with a worse cardiovascular risk profile, taking into consideration higher rate of high blood pressure (HBP), dyslipidemia, diabetes, obesity, chronic kidney disease (CKD), cerebrovascular disease, and heart failure (HF). Smoking, peripheral arterial disease (PAD), previous AMI and previous percutaneous coronary intervention (PCI) were more common among men.
Patient baseline characteristics.
| Total (n=14470) | Male (n=10749) | Female (n=3721) | p-Value | |
|---|---|---|---|---|
| Age (years) – mean (SD) | 64(13.5) | 62(12.8) | 70(13.8) | <0.001 |
| Medical history | ||||
| HBP | 8764/13999(62.6) | 6150/10392(59.2) | 2614/3607(72.5) | <0.001 |
| Dislipidemia | 7288/13512(53.9) | 5354/10040(53.3) | 1934/3472(55.7) | 0.015 |
| History of smoking | 4983/14428(34.5) | 4305/10720(40.2) | 678/3708(18.3) | <0.001 |
| Diabetes | 3564/14009(25.4) | 2392/10420(23.0) | 1172/3589(32.7) | <0.001 |
| Obesity | 2690/12394(21.7) | 1965/9285(21.2) | 725/3109(23.3) | 0.012 |
| Angina pectoris | 2100/13025(16.1) | 1528/9766(15.6) | 572/3259(17.6) | 0.010 |
| History of AMI | 1431/13019(11.0) | 1161/9755(11.9) | 270/3264(8.3) | <0.001 |
| Previous PCI | 1263/13243(9.5) | 1049/9896(10.6) | 214/3347(6.4) | <0.001 |
| Previous CABG | 167/13282(1.3) | 132/9925(1.3) | 35/3357(1.0) | 0.196 |
| Ischemic stroke/TIA | 697/13182(5.3) | 486/9869(4.9) | 211/3313(6.4) | 0.001 |
| PAD | 420/13254(3.2) | 338/9905(3.4) | 82/3349(2.4) | 0.006 |
| Heart failure | 414/13126(3.2) | 265/9819(2.7) | 149/3307(4.5) | <0.001 |
| Valvular heart disease | 223/13083(1.7) | 114/9796(1.2) | 109/3287(3.3) | <0.001 |
| CKD | 606/12472(4.9) | 406/9312(4.4) | 200/3160(6.3) | <0.001 |
| Cancer | 514/11669(4.4) | 339/8724(3.9) | 175/2945(5.9) | <0.001 |
| COPD | 464/13162(3.5) | 344/9824(3.5) | 120/3338(3.6) | 0.801 |
| Dementia | 188/10722(1.8) | 84/8026(1.0) | 104/2696(3.9) | <0.001 |
| Family history CAD | 915/13211(6.9) | 693/9835(7.0) | 222/3376(6.6) | 0.353 |
AMI: acute myocardial infarction; CABG: coronary artery bypass graft; CAD: coronary artery disease; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; HBP: high blood pressure; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention; SD: standard deviation; TIA: transient ischemic attack.
Conversely, women were more previously medicated with clopidogrel, beta blockers, angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), calcium channel blockers, mineralocorticoid receptor antagonists (MRA), and statins.
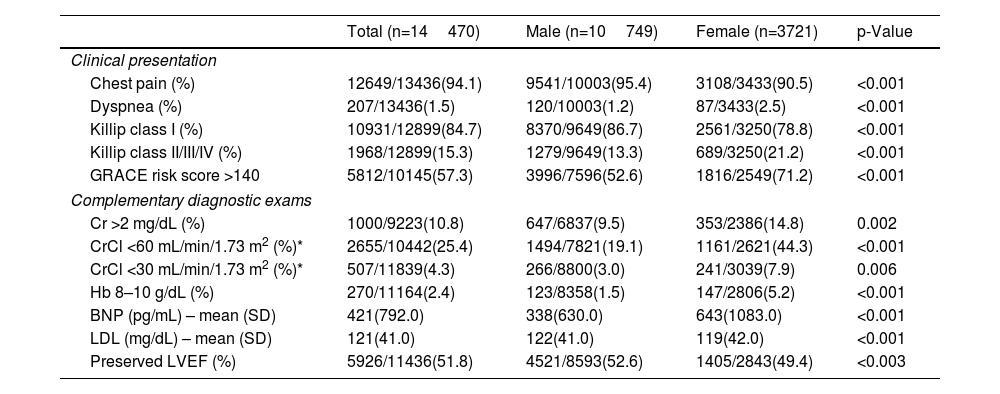
Clinical findings and treatmentClinical presentation characteristics and inpatient treatment strategies are shown in Tables 2 and 3 and discharge features are shown in Table 4. Chest pain was the most common symptom in both sexes. However, female patients had more atypical presentations, especially dyspnea, a worse clinical profile with a higher Killip class, and worse serum biomarkers, such as elevated creatinine and B-type natriuretic peptide (BNP), and lower hemoglobin. In fact, women had a higher median calculated global registry of acute coronary events (GRACE) risk score (161 vs. 146, p-value <0.001). Severely depressed left ventricular ejection fraction (LVEF) was more frequent in women (8.2% vs. 6.4%, p-value <0.001).
Patient clinical findings.
| Total (n=14470) | Male (n=10749) | Female (n=3721) | p-Value | |
|---|---|---|---|---|
| Clinical presentation | ||||
| Chest pain (%) | 12649/13436(94.1) | 9541/10003(95.4) | 3108/3433(90.5) | <0.001 |
| Dyspnea (%) | 207/13436(1.5) | 120/10003(1.2) | 87/3433(2.5) | <0.001 |
| Killip class I (%) | 10931/12899(84.7) | 8370/9649(86.7) | 2561/3250(78.8) | <0.001 |
| Killip class II/III/IV (%) | 1968/12899(15.3) | 1279/9649(13.3) | 689/3250(21.2) | <0.001 |
| GRACE risk score >140 | 5812/10145(57.3) | 3996/7596(52.6) | 1816/2549(71.2) | <0.001 |
| Complementary diagnostic exams | ||||
| Cr >2 mg/dL (%) | 1000/9223(10.8) | 647/6837(9.5) | 353/2386(14.8) | 0.002 |
| CrCl <60 mL/min/1.73 m2 (%)* | 2655/10442(25.4) | 1494/7821(19.1) | 1161/2621(44.3) | <0.001 |
| CrCl <30 mL/min/1.73 m2 (%)* | 507/11839(4.3) | 266/8800(3.0) | 241/3039(7.9) | 0.006 |
| Hb 8–10 g/dL (%) | 270/11164(2.4) | 123/8358(1.5) | 147/2806(5.2) | <0.001 |
| BNP (pg/mL) – mean (SD) | 421(792.0) | 338(630.0) | 643(1083.0) | <0.001 |
| LDL (mg/dL) – mean (SD) | 121(41.0) | 122(41.0) | 119(42.0) | <0.001 |
| Preserved LVEF (%) | 5926/11436(51.8) | 4521/8593(52.6) | 1405/2843(49.4) | <0.003 |
BNP: B-type natriuretic peptide; CrCl: creatinine clearance; GRACE: global registry of acute coronary events; Hb: hemoglobin; LDL: low-density lipoprotein; LVEF: left ventricular ejection fraction.
Patient treatment.
| Total (n=14470) | Male (n=10749) | Female (n=3721) | p-Value | |
|---|---|---|---|---|
| Reperfusion therapy | 9238/14434(64.0) | 7052/10723(65.8) | 2186/3711(58.9) | <0.001 |
| PCI | 11582/14399(80.4) | 8818/10701(82.4) | 2764/3698(74.7) | <0.001 |
| Culprit artery (PCI) | ||||
| LAD | 5284/10714(49.3) | 4018/8157(49.3) | 1266/2557(49.5) | 0.823 |
| RCA | 4147/10304(40.2) | 3159/7865(40.2) | 988/2439(40.5) | 0.763 |
| LCx | 1954/9843(19.9) | 1574/7547(20.9) | 380/2296(16.6) | <0.001 |
| LMA | 140/8954(1.6) | 104/6845(1.5) | 36/2109(1.7) | 0.544 |
| Graft | 50/147(34.0) | 43/118(36.4) | 7/29(24.1) | 0.210 |
| Multivessel disease (%) | 4640/10639(43.6) | 3567/8034(44.4) | 1073/2605(41.2) | 0.004 |
| CAG characterization | ||||
| Radial access | 7164/10469(68.4) | 5578/7934(70.3) | 1586/2535(62.6) | <0.001 |
| Femoral access | 3305/10469(31.6) | 2356/7934(29.7) | 949/2535(37.4) | <0.001 |
| Single-vessel PCI | 5995/8898(67.4) | 4576/6801(67.3) | 1419/2097(67.7) | 0.743 |
| Multivessel PCI | 1226/8898(13.8) | 968/6801(14.2) | 258/2097(12.3) | <0.025 |
| DES | 5329/8845(60.2) | 4151/6754(61.5) | 1178/2091(56.3) | <0.001 |
| BMS | 1586/8845(17.9) | 1187/6754(17.6) | 399/2091(19.1) | 0.116 |
| Thrombectomy | 2431/10598(22.9) | 1869/8102(23.1) | 562/2496(22.5) | 0.566 |
| Medical treatment (inpatient) | ||||
| Statins | 11386/12179(93.5) | 8529/9091(93.8) | 2857/3088(92.5) | <0.012 |
| Aspirin | 10718/11534(92.9) | 8005/8578(93.3) | 2713/2956(91.8) | 0.005 |
| Clopidogrel | 8252/12192(67.7) | 6115/9099(67.2) | 2137/3093(69.1) | 0.053 |
| Ticagrelor | 3573/10066(35.5) | 2751/7542(36.5) | 822/2525(32.6) | <0.001 |
| ACEi/ARB | 10104/12167(83.0) | 7648/9080(84.2) | 2456/3987(79.6) | <0.001 |
| Beta blocker | 9491/12161(78.0) | 7199/9081(79.3) | 2292/3080(74.4) | <0.001 |
| MRA | 1466/12107(12.1) | 1052/9032(11.6) | 414/3075(13.5) | 0.008 |
| Diuretics | 3219/12111(26.6) | 2122/9035(23.5) | 1097/3076(35.7) | <0.001 |
| Inotropes | 936/12094(7.7) | 595/9020(6.6) | 341/3074(11.1) | <0.001 |
ACEi: angiotensin-converting enzyme inhibitors; ARB: angiotensin receptor blockers; BMS: bare-metal stent; BNP: B-type natriuretic peptide; CAG: coronary angiography; CCB: calcium channel blockers; DES: drug-eluting stent; LAD: left anterior descending; LCx: left circumflex; LMA: left main artery; MRA: mineralocorticoid receptor antagonists; PCI: percutaneous coronary intervention; RCA: right coronary artery.
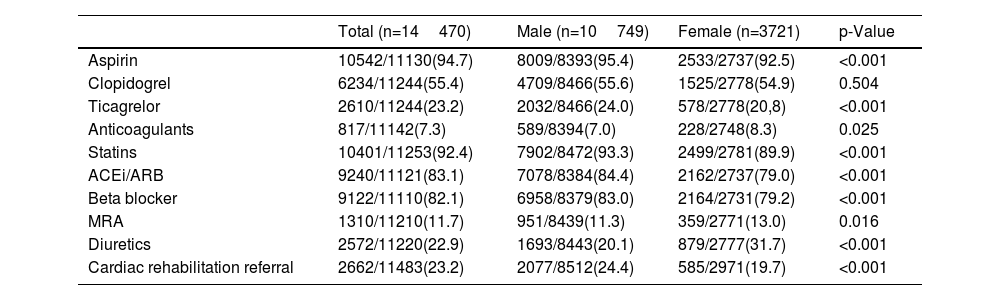
Discharge medication and referral.
| Total (n=14470) | Male (n=10749) | Female (n=3721) | p-Value | |
|---|---|---|---|---|
| Aspirin | 10542/11130(94.7) | 8009/8393(95.4) | 2533/2737(92.5) | <0.001 |
| Clopidogrel | 6234/11244(55.4) | 4709/8466(55.6) | 1525/2778(54.9) | 0.504 |
| Ticagrelor | 2610/11244(23.2) | 2032/8466(24.0) | 578/2778(20,8) | <0.001 |
| Anticoagulants | 817/11142(7.3) | 589/8394(7.0) | 228/2748(8.3) | 0.025 |
| Statins | 10401/11253(92.4) | 7902/8472(93.3) | 2499/2781(89.9) | <0.001 |
| ACEi/ARB | 9240/11121(83.1) | 7078/8384(84.4) | 2162/2737(79.0) | <0.001 |
| Beta blocker | 9122/11110(82.1) | 6958/8379(83.0) | 2164/2731(79.2) | <0.001 |
| MRA | 1310/11210(11.7) | 951/8439(11.3) | 359/2771(13.0) | 0.016 |
| Diuretics | 2572/11220(22.9) | 1693/8443(20.1) | 879/2777(31.7) | <0.001 |
| Cardiac rehabilitation referral | 2662/11483(23.2) | 2077/8512(24.4) | 585/2971(19.7) | <0.001 |
The time from first symptoms to first medical contact (patient delay) was higher among women, approximately 2.6 hours and 2.2 hours in men (median values with p-value <0.001), as well as system delay (2.9 hours vs. 2.5 hours, p-value <0.001). Similar trends were observed in the time from first symptoms to revascularization (median values: four hours for male vs. 4.8 hours for female, p-value <0.001).
The occurrence of inferior and anterior STEMI, 50.6% and 47.9% respectively, was similar between sexes. The localization of the STEMI was reported in 13174 patients.
Regarding treatment, coronary angiography (CAG) was performed in 12599 patients (87.5%), significantly less frequently in women (84.4% vs. 88.5%, p-value <0.001), and also reperfusion therapy (58.9% vs. 65.8%, p-value<0.001), including both fibrinolysis and primary angioplasty. Nevertheless, CAG without significant epicardial lesions was more common among women (16.5% vs. 13.3%, p-value <0.001). The distribution of the most common culprit artery was identical, with left anterior descending (LAD) artery accounting for 44% and the right coronary artery (RCA) for 36% of the total population. The success of revascularization was higher than 90%, and with no differences between sexes in the most common culprit arteries.
As for medical treatment, statins, aspirin, ticagrelor, ACEi/ARB, and beta blockers were less prescribed in women, with an opposite tendency for the prescription of anticoagulants, nitrates, MRA, diuretics, and inotropes. Although low referral rates for cardiac rehabilitation were observed in the total population, women were referred even less.
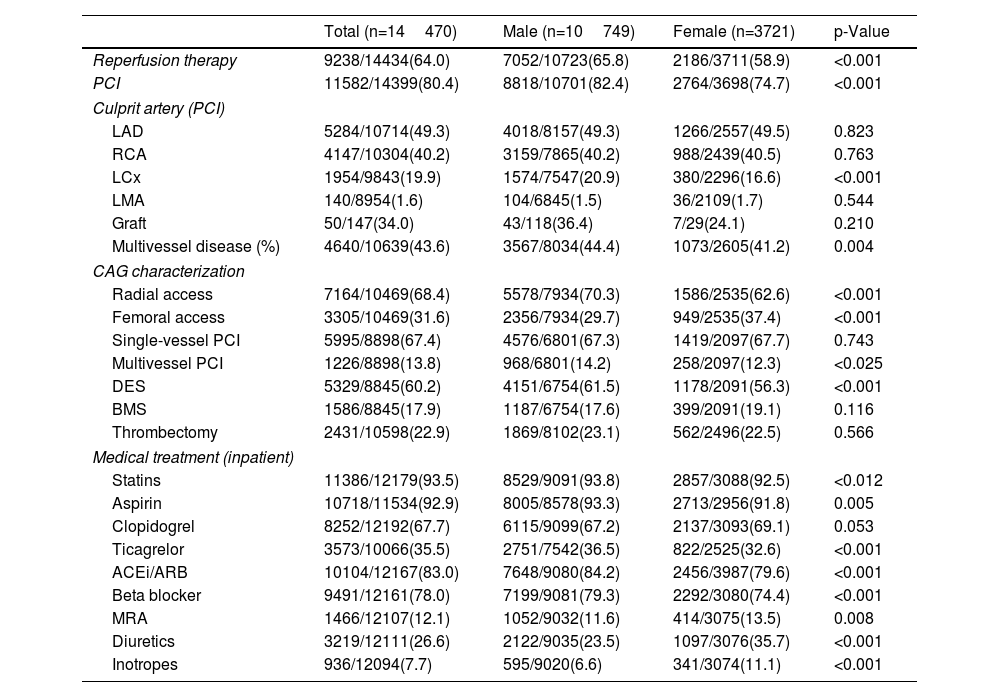
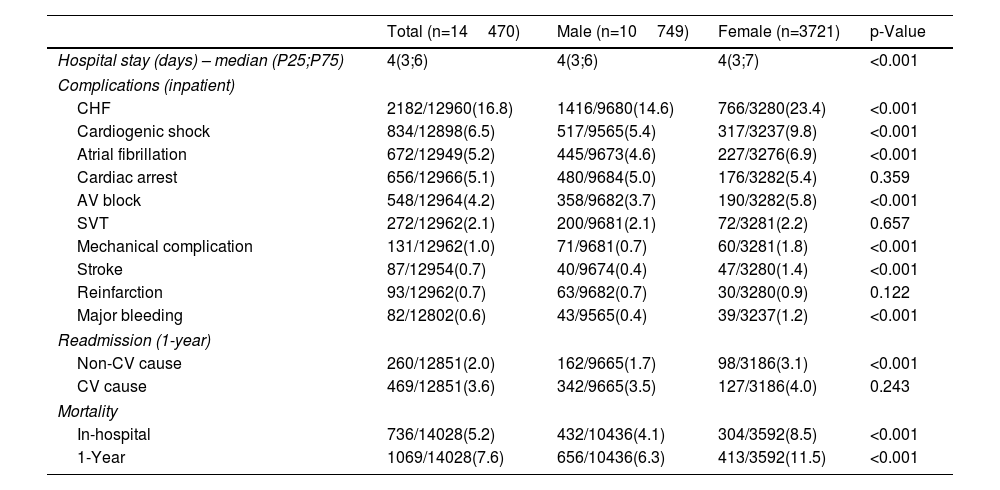
Study endpointsIn-hospital mortality was reported in 736 patients (5.2%) (304 females, i.e. 8.5%, vs. 432 males, i.e. 4.1%, p-value<0.001), and one-year mortality in 1069 patients (7.6%) (413 females, i.e. 11.5%, vs. 656 males, i.e. 6.3%, p-value<0.001) (Table 5).
Inpatient complications, readmission and mortality.
| Total (n=14470) | Male (n=10749) | Female (n=3721) | p-Value | |
|---|---|---|---|---|
| Hospital stay (days) – median (P25;P75) | 4(3;6) | 4(3;6) | 4(3;7) | <0.001 |
| Complications (inpatient) | ||||
| CHF | 2182/12960(16.8) | 1416/9680(14.6) | 766/3280(23.4) | <0.001 |
| Cardiogenic shock | 834/12898(6.5) | 517/9565(5.4) | 317/3237(9.8) | <0.001 |
| Atrial fibrillation | 672/12949(5.2) | 445/9673(4.6) | 227/3276(6.9) | <0.001 |
| Cardiac arrest | 656/12966(5.1) | 480/9684(5.0) | 176/3282(5.4) | 0.359 |
| AV block | 548/12964(4.2) | 358/9682(3.7) | 190/3282(5.8) | <0.001 |
| SVT | 272/12962(2.1) | 200/9681(2.1) | 72/3281(2.2) | 0.657 |
| Mechanical complication | 131/12962(1.0) | 71/9681(0.7) | 60/3281(1.8) | <0.001 |
| Stroke | 87/12954(0.7) | 40/9674(0.4) | 47/3280(1.4) | <0.001 |
| Reinfarction | 93/12962(0.7) | 63/9682(0.7) | 30/3280(0.9) | 0.122 |
| Major bleeding | 82/12802(0.6) | 43/9565(0.4) | 39/3237(1.2) | <0.001 |
| Readmission (1-year) | ||||
| Non-CV cause | 260/12851(2.0) | 162/9665(1.7) | 98/3186(3.1) | <0.001 |
| CV cause | 469/12851(3.6) | 342/9665(3.5) | 127/3186(4.0) | 0.243 |
| Mortality | ||||
| In-hospital | 736/14028(5.2) | 432/10436(4.1) | 304/3592(8.5) | <0.001 |
| 1-Year | 1069/14028(7.6) | 656/10436(6.3) | 413/3592(11.5) | <0.001 |
AV: atrioventricular; CHF: congestive heart failure; CV: cardiovascular; IH: in-hospital; SVT: sustained ventricular tachycardia.
Women had more one-year non-cardiovascular readmission and in-hospital complications, including congestive HF, shock, mortality, atrial fibrillation, atrioventricular block, mechanical complications, stroke and major bleeding. However, reinfarction, SVT, cardiac arrest, and cardiovascular readmission, did not achieve statistical significance, despite higher rates among women (Table 5).
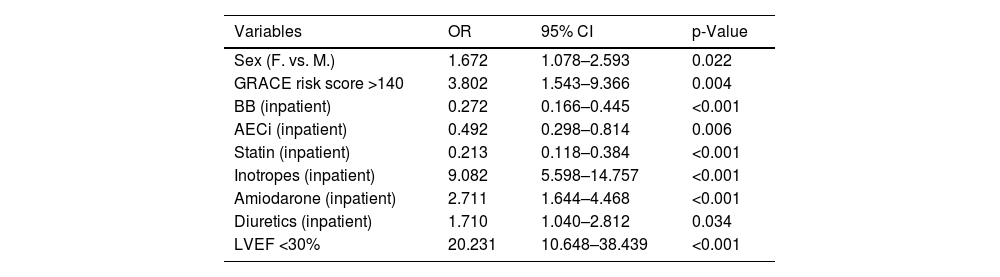
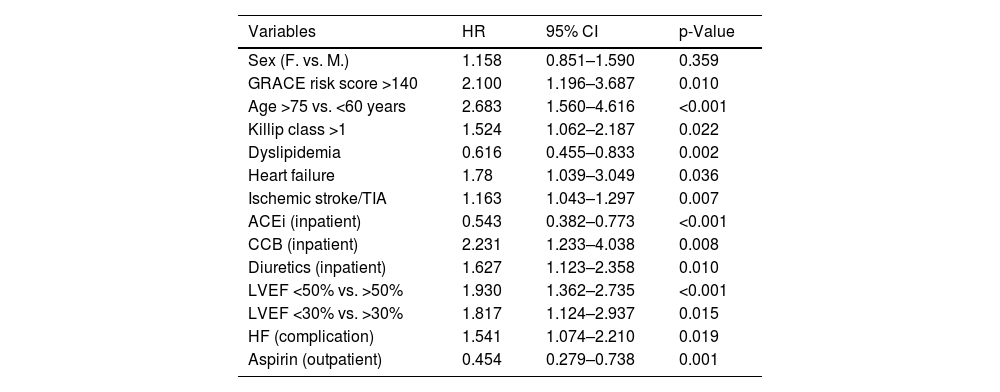
Survival analysis and adjusted analysisSurvival analysis is shown in Figure 1. Multivariate logistic regression for in-hospital mortality and Cox proportional hazard regression for one-year mortality are shown in Tables 6 and 7, respectively.
Multivariate analysis for in-hospital mortality (other variables included not shown).
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Sex (F. vs. M.) | 1.672 | 1.078–2.593 | 0.022 |
| GRACE risk score >140 | 3.802 | 1.543–9.366 | 0.004 |
| BB (inpatient) | 0.272 | 0.166–0.445 | <0.001 |
| AECi (inpatient) | 0.492 | 0.298–0.814 | 0.006 |
| Statin (inpatient) | 0.213 | 0.118–0.384 | <0.001 |
| Inotropes (inpatient) | 9.082 | 5.598–14.757 | <0.001 |
| Amiodarone (inpatient) | 2.711 | 1.644–4.468 | <0.001 |
| Diuretics (inpatient) | 1.710 | 1.040–2.812 | 0.034 |
| LVEF <30% | 20.231 | 10.648–38.439 | <0.001 |
CI: confidence interval; OR: odds ratio.
Cox's hazard regression (one-year mortality) (other variables included not shown).
| Variables | HR | 95% CI | p-Value |
|---|---|---|---|
| Sex (F. vs. M.) | 1.158 | 0.851–1.590 | 0.359 |
| GRACE risk score >140 | 2.100 | 1.196–3.687 | 0.010 |
| Age >75 vs. <60 years | 2.683 | 1.560–4.616 | <0.001 |
| Killip class >1 | 1.524 | 1.062–2.187 | 0.022 |
| Dyslipidemia | 0.616 | 0.455–0.833 | 0.002 |
| Heart failure | 1.78 | 1.039–3.049 | 0.036 |
| Ischemic stroke/TIA | 1.163 | 1.043–1.297 | 0.007 |
| ACEi (inpatient) | 0.543 | 0.382–0.773 | <0.001 |
| CCB (inpatient) | 2.231 | 1.233–4.038 | 0.008 |
| Diuretics (inpatient) | 1.627 | 1.123–2.358 | 0.010 |
| LVEF <50% vs. >50% | 1.930 | 1.362–2.735 | <0.001 |
| LVEF <30% vs. >30% | 1.817 | 1.124–2.937 | 0.015 |
| HF (complication) | 1.541 | 1.074–2.210 | 0.019 |
| Aspirin (outpatient) | 0.454 | 0.279–0.738 | 0.001 |
CI: confidence interval; HR: hazard ratio.
After adjusted analysis, female sex remained as an independent factor for in-hospital mortality (OR=1.672; 95% CI [1.078–2.593]; p=0.022) but not for one-year mortality.
Regarding in-hospital mortality, several statistically significant variables in univariate analysis – including baseline characteristics such as HBP, diabetes, angina, VHD, HF, history of smoking, cerebrovascular disease, PAD, CKD, cancer, chronic obstructive pulmonary disease, clinical findings with GRACE risk score and STEMI localization, as well as medication use both prior to and during hospitalization and angiographic characteristics like multivessel disease, culprit artery, and time to reperfusion – were incorporated into the regression model. Likewise, the regression model for one-year mortality included HBP, VHD, PAD, CKD, cancer, prior, inpatient and outpatient medications, the use of PCI, angiographic characteristics (multivessel disease), and in-hospital complications.
GRACE risk score, inotropes and LVEF lower than 30% were the most important independent predictors for in-hospital mortality. Guideline-directed medical therapy was associated with a reduced risk of in-hospital mortality. Moreover, older age, in-hospital complications, worse clinical profiles at admission, including GRACE risk score, and lower LVEF were independent predictors for one-year mortality.
DiscussionApproximately one-quarter of our population was female, consistent with the underrepresentation of women in clinical studies regarding ACS.6,9,15,21
Similar to other European registries – such as in Estonia, Hungary, Norway, Sweden and Vienna – and to other studies,1,3,6–8,10,16 women were older and had a higher frequency of several cardiovascular risk factors. Coronary artery disease appears to be age-dependent in women, especially occurring after menopause6 and typically five to 10 years after men,6,21 due to the protective effects of estrogen.21 Moreover, these risk factors appear to have a more unfavorable role in women – for example, the OR of AMI in diabetic women is higher compared to men (4.26 vs. 2.67).19 Unassessed comorbidities, such as depression,13,21 anxiety and stress21 may be related to worse outcomes. The prevalence of depression after an AMI is estimated to be 20% and doubles in women compared to men.12 A study found higher early complication rates in patients with anxiety or depression and proposes the use of screening tools to manage this comorbidity better.12 These data probably justify the inclusion of these new variables in future registries.
Chest pain is the most common symptom of acute ACS.11 Nevertheless, atypical symptoms appear to be more common among women,1,7,21 in accordance with the present study, which is an alarming feature that can lead to misdiagnosis and undertreatment.1 Furthermore, women appear to wait longer before seeking healthcare3,7,11,13,16,17; this was also observed in the present study. Reducing this delay may have potential benefits on mortality and morbidity.3 In our analysis, despite a higher prevalence of obesity, BNP levels in women were twice as high as those in men, probably corroborating a delayed and worse clinical presentation, as well as the presence of other comorbidities known to increase BNP levels (anemia, CKD). Awareness around clinicians should be raised, and effective educational campaigns targeting the general population should address this issue.
The management of STEMI differed based on sex1,6,7,16; women underwent CAG, PCI, and guideline-directed medical therapy less frequently. Accordingly, a study found lower prescription of ticagrelor and prasugrel in women.22 Lower prescription of dual antiplatelet (DAPT) therapy could be explained by low adherence to guideline recommendations in conservative cases and also due to higher prescription of oral anticoagulants1; this was presumed in the current study due to the higher frequency of atrial fibrillation and anticoagulation at discharge. While the rate of major bleeding in our population was low, concerns about higher bleeding risk in women may also contribute to lower adherence to DAPT.1,22 Thus, these differences may be attributed to older age and frailty,1 which is consistent with our population of frailer women. This characteristic was, however, inferred through other features.
In another recent study among patients with ACS, similar tendencies were observed with less guideline-directed therapy during both prehospital and hospital care in women.11 It is suggested that this difference is greater in prehospital care,11 which is a parameter that was not evaluated in our study. Ours reveals differences in discharge medications that could be partly explained by increased comorbidities in women. Nevertheless, clinicians should be aware of these differences in order to prescribe optimized medical therapy and individualize treatment regardless of the patient's sex.
On the other hand, the lower rates of PCI in our study may be partially explained by the higher number of normal CAG findings in women, while the success of PCI for the most common culprit artery was similar, suggesting that equivalent treatment was offered in cases that underwent PCI. Myocardial infarction with non-obstructive coronary arteries (MINOCA) is a heterogeneous entity more frequently found in women and associated with a higher risk of cardiovascular events19 that should be properly addressed. However, as ProACS does not collect information regarding MINOCA, this analysis could not be performed in the present study.
Our analysis revealed a more significant role of sex in in-hospital mortality. There is consistent evidence that women have higher short-term mortality, while there are conflicting results for long-term mortality.6,7 In a recent metanalysis, the effect of difference in sex on short-term mortality was significant, in contrast to long-term mortality, even after attenuation with adjusted analysis.7 In contrast, women had higher short and long-term mortality rates in several registries, although both these differences seem to attenuate after adjusted analysis in European countries,1,16 but not in India.9 The justification for these differences is not known, although frailty1 and worse cardiovascular profiles7 may play a role.
An international study regarding thirty-day mortality found statistically higher mortality in women after adjusted analysis but that these differences were stronger in younger patients, and not related to treatment variations.13 Other studies in younger women had similar results.21 Conversely, a study focusing on differences in STEMI patients who underwent PCI, did not find differences in thirty-day and one-year mortality.10
Most of these studies are based on registries and observational data and one-year follow-up.6 A subanalysis from the EXAMINATION-EXTENDED trial, with a 10-year follow-up, encountered a higher incidence of all-cause and cardiac death in women. After adjusted analysis of its primary endpoint, a composite of all-cause death, myocardial infarction and revascularization, sex was not a predictor of events, while age was the most important one.6 The authors suggest that HF and cardiogenic shock may lead to worse outcomes in women, as they are related to higher in-hospital and thirty-day mortality,6 similar to our findings. Other complications, including bleeding and mechanical complications were also reported as more common among women.7
In our analysis, lower LVEF was associated with mortality, which is similar to previous studies in which LVEF was an independent predictor of in-hospital complications.12 On the other hand, with regard to noncardiac comorbidities and death,6 the delay in seeking medical observation and in diagnosis,13 may play a role in all-cause death. In this context, one study focused on in-hospital STEMI and found there were fewer disparities in baseline characteristics between sexes, although longer times, less guideline-medical therapy in women, and no significant differences in mortality.2
There are several recommendations to improve outcomes in women, including education campaigns for the general population, particularly women, education campaigns for healthcare providers and the implementation of protocols for STEMI management.17 In fact, STEMI management protocols may reduce sex differences,10,14,17 and one study observed a reduction in thirty-day mortality in women.17 Further research is of utmost importance, and the use of artificial intelligence may help reduce existing bias.17
There are sex-based differences in the pathophysiology of acute myocardial infarction (AMI)1,5,8,13,14 which may play a role in mortality.13 While plaque rupture and thrombus formation are established mechanisms in men, plaque erosion,4 inflammation, endothelial dysfunction, coronary vasospasm, spontaneous coronary dissection and connective tissue disorders may have a role in women.1 Furthermore, women have smaller vessels, fewer collaterals and increased vascular stiffness.13 Estrogen may act as a plaque stabilizer, and the small vessel size and higher blood flow may lead to increased endothelial shear stress, thus contributing to plaque erosion.4
Differences in thrombogenicity between sexes may also be a plausible cause related to sex hormones; a study found that women with high thrombus burden in an acute setting had higher cardiovascular mortality compared to men. Moreover, another prospective study found higher clopidogrel resistance in women. High thrombus burden appears to be important in prognosis and may indicate the need for a more aggressive treatment.15 These factors were not accounted for in our study.
Despite the conflicting results, sex-based differences in AMI cannot be denied.7
Study limitationsThis study has several limitations, such as its observational and voluntary nature, with the possibility of inaccurate data and residual confounding factors that were not considered. Several noncardiac characteristics, including psychiatric comorbidities and hormone-related issues were not documented. Another concern is the underrepresentation of women, although our numbers were consistent with several previous analyses. Furthermore, missing follow-up data may result in the loss of significant endpoints. Lastly, the generalization of our findings should be made with caution, even within Portugal, as geographical differences in the management of these patients were not evaluated.
ConclusionThere are important sex-related differences in Portuguese STEMI patients. Compared with men, women were older and had a worse cardiovascular risk profile. In terms of clinical management, women were less likely to receive reperfusion therapy as well as other important medications with impact on prognosis. In-hospital mortality was higher in women. Nevertheless, this difference disappeared after attenuation analysis at the end of the first year.
According to our results there is room to improve the clinical management of women with STEMI. Efforts should be made toward achieving an equal standard of care. Standardized diagnosis and treatment protocols, as well as education campaigns targeting the general population and clinicians, may help reduce this sex bias. Noncardiac comorbidities should also be accounted for.
For a better understanding of sex differences in STEMI patients, further studies are needed, as they may help to improve medical therapy tailored according to sex and to reduce AMI mortality.
Authors’ contributionsDuring the preparation of this work the author(s) used ChatGPT 3.5 to correct grammar errors. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
Ethical approvalThe ProACS registry is approved by the Portuguese Data Protection Authority (No. 3140/2010) and registered at ClinicalTrials.gov (NCT01642329).
Conflicts of interestThe authors have no conflicts of interest to declare.