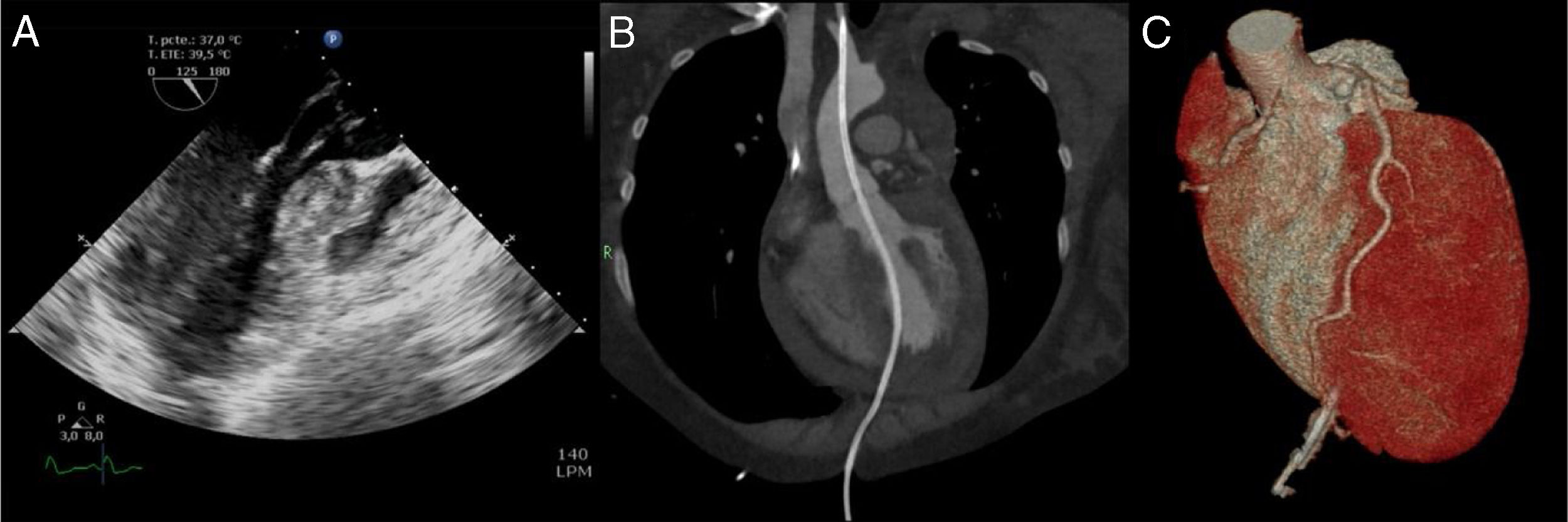
A 27-year-old woman was admitted to our center after emergency vascular surgery for spontaneous dissection of the left iliac artery. Congenital factor VIII deficiency and family history of complicated brain aneurysm were previously reported. Hemoperitoneum and hemothorax were identified after surgery as consequences of a severe coagulation disorder and the patient suffered cardiac arrest with pulseless electrical activity. A portable echocardiograph detected pericardial effusion and emergency blind subxiphoid pericardiocentesis was performed with recovery of pulse. An urgent cardiology evaluation was subsequently required. Transthoracic echocardiography views were severely limited, so it was decided to undertake transesophageal echocardiography. This revealed a catheter crossing the aortic valve to the ascending aorta (Figure 1A). Contrast-enhanced computed tomography angiography confirmed the intravascular placement of a drainage with its distal tip in the proximal segment of the left carotid artery (Figure 1B). The ventricular insertion point was in the anterior interventricular groove, close to the distal segment of the left anterior descending coronary artery (Figure 1C). Prior to entering the operating room, the patient suffered a new cardiac arrest and resuscitation maneuvers were ineffective. Subsequent autopsy revealed systemic vascular and tissue fragility (spontaneous liver and spleen lacerations, aortic rupture and hyoid bone fracture with minimal procedural manipulation), compatible with a diagnosis of type 4 Ehlers-Danlos syndrome.
Multimodality imaging of the path of the pericardiocentesis catheter crossing the aortic valve to the ascending aorta. (A) Two-dimensional transesophageal echocardiogram, left ventricular outflow tract projection; (B) computed tomography curved format reconstruction along the catheter; (C) three-dimensional volume-rendered computed tomography reconstruction of the catheter insertion point and its relationship with the anterior descending artery.
This report has two key messages. Pericardiocentesis is not free from severe complications and should be performed with imaging whenever possible. Moreover, a congenital connective tissue disorder should be suspected in young patients with spontaneous arterial complications.
Conflicts of interestThe authors have no conflicts of interest to declare.