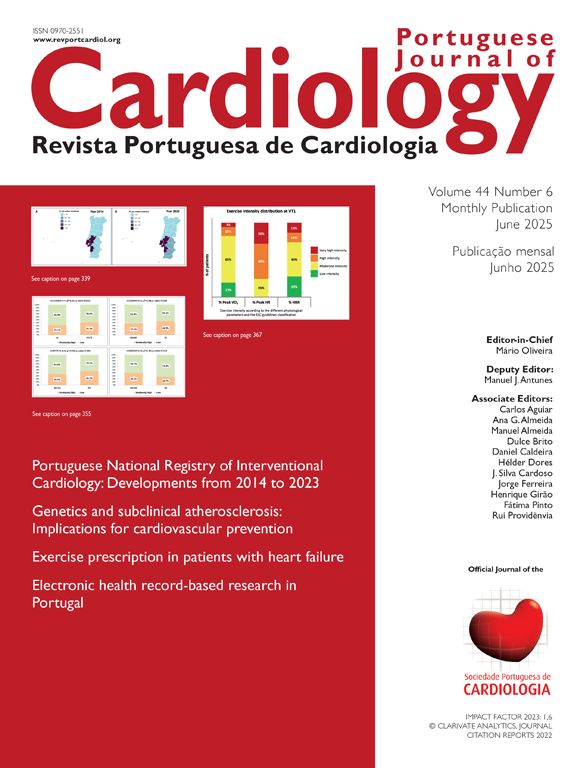
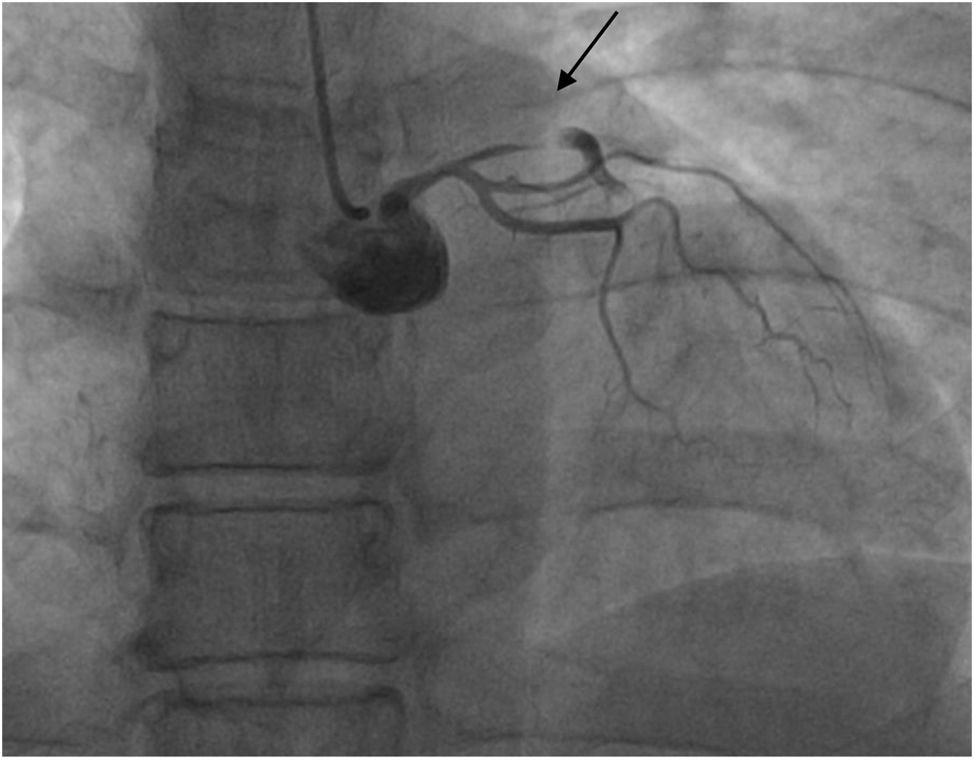
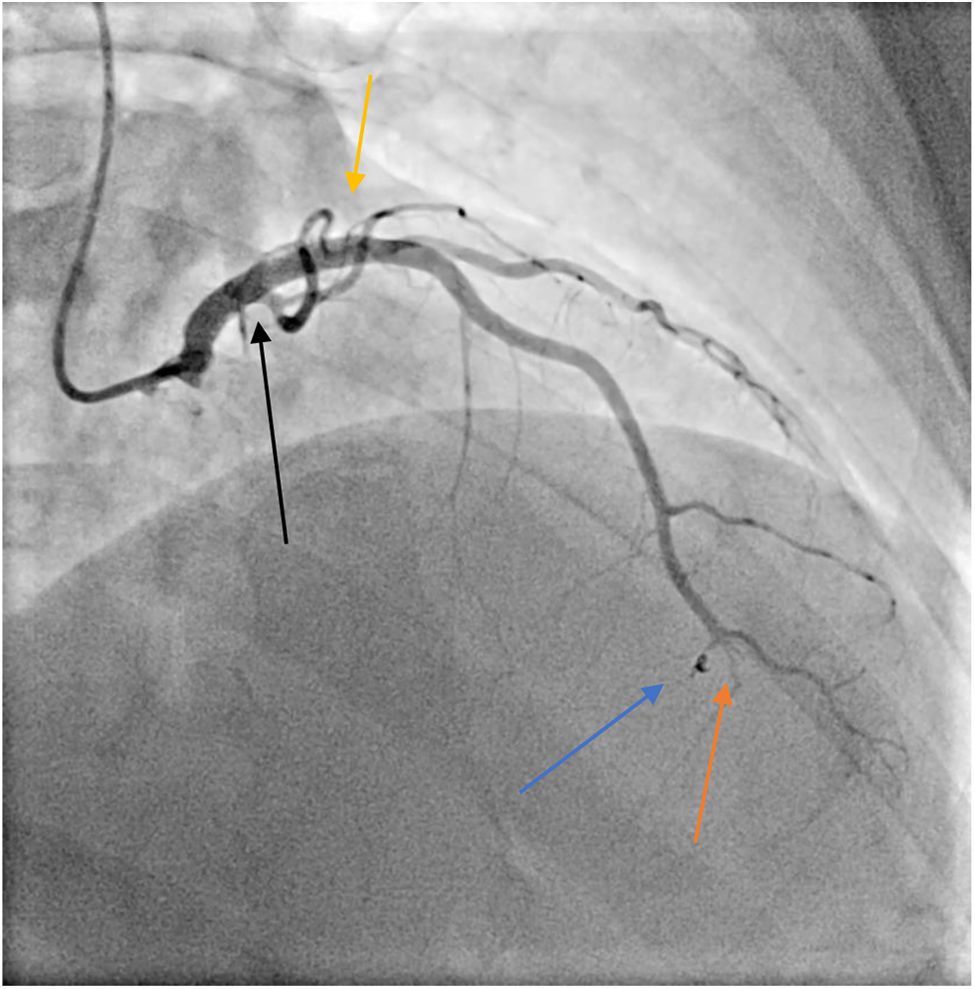
A 42-year-old female arrived at our hospital with epigastric pain: electrocardiogram (ECG) was negative and echocardiography normal, but troponin levels were elevated. Coronary angiography revealed a spontaneous dissection of the distal left anterior descending artery (LAD) – Type 2b according to the Yip-Saw classification.1,2 No angioplasty was performed, and she was discharged on aspirin. Two days later, she was readmitted for a large anterior ST elevation myocardial infarction; the first point of high-sensitivity troponin I (hs-TnI) was 5000 ng/L, prompting an urgent coronary angiography. This showed occlusion of the ostial LAD and wall hematoma, extending proximally to the left main artery (Figure 1 and Supplementary video 1). We pre-dilated the LAD, resulting in occlusion of the vessel and the diagonal branch, thus precipitating cardiogenic shock, requiring noradrenaline. Stenting of LAD and left main artery was then performed; the diagonal branch remained occluded, with evidence of circumflex coronary (CX) thrombosis and upstream of the stent in the left main (LM) (Figure 2). Due to persistent cardiogenic shock, an intra-aortic balloon pump (IABP) was inserted. Intravascular ultrasound revealed stent malapposition, necessitating post-dilation in the diagonal branch (Supplementary video 2). A small iatrogenic perforation in a distal septal branch required a microcoil insertion (Figure 2 and Supplementary video 3). The post-percutaneous coronary intervention echo revealed akinesia of the apex and anterior wall with reduced left ventricular ejection fraction (35%). The patient was transferred to cardiovascular intensive care with weaning from vasopressors and IABP in one day. A cerebral magnetic resonance to exclude fibromuscular dysplasia was negative. A pre-discharge coronary angiography showed residual occlusion of the distal LAD and complete recanalization of Cx (Figure 3 and Supplemntary video 4); in a few days ventricular function was fully recovered. The patient was successfully discharged after ten days in good clinical condition with the following home therapy: Cardio aspirin, clopidogrel, bisoprolol, pantoprazole, atorvastatin/ezetimibe.2
Pre-discharge coronary angiography showing a completely occluded distal left anterior descending artery (LAD) (orange arrow), good angiographic result of the previous ostial LAD stent (yellow arrow), excellent coil retention (blue arrow) in the septal artery, and complete resolution of the thrombosis in the circumflex artery (black arrow).
None declared.
Conflict of interestsThe authors state that they have no conflict of interests.