Pulmonary artery sarcoma is a rare type of tumor and is easily misdiagnosed. We report a case of pulmonary artery sarcoma in a 26-year-old young man who presented with acute onset of dyspnea. Computed tomographic angiography of the chest had revealed a large filling defect within the main pulmonary artery (PA) that extended into both right and left PAs. Because pulmonary embolism was suspected, both anticoagulant and thrombolytic therapies were initiated. The patient responded poorly to these therapies, leading to the resection of the mass. After an uneventful postoperative course, the patient was discharged from the hospital on postoperative day ten. He was subsequently treated with chemotherapy and continued to show no evidence of disease. Multimodal therapy can provide prolonged survival.
O sarcoma da artéria pulmonar é um tumor raro, de diagnóstico difícil. Apresentamos um caso de sarcoma da artéria pulmonar num jovem de 26 anos que se manifestou por um quadro de dispneia aguda. A angiografia computadorizada do tórax revelou um extenso defeito de preenchimento no tronco da artéria pulmonar que se estendia para ambos os seus ramos. Devido à suspeita de embolia pulmonar, foi iniciada terapêutica anticoagulante e trombolítica. O doente respondeu mal a este tratamento tendo posteriormente sido efetuada a resseção da massa. O doente teve alta ao 10° dia pós-operatório, sem complicações. Foi posteriormente submetido a quimioterapia, sem recidiva da doença, revelando que a terapêutica multimodal pode prolongar a sobrevivência desta patologia.
Pulmonary artery sarcoma (PAS) is a rare tumor of the pulmonary artery (PA) that is easily misdiagnosed as pulmonary thromboembolism (PTE). Patients often miss the opportunity for early diagnosis and treatment, which severely affects their prognosis.1,2 We report a case in which PAS was found in a young man who presented with acute onset of dyspnea. The patient was misdiagnosed and treated for pulmonary embolism (PE).
Case reportA 26-year-old man was transferred from another hospital for treatment of PAS. The patient had reported acute onset of chest tightness, shortness of breath and dyspnea for one month. When he was admitted to hospital, his symptoms were aggravated, heart rate 108 bpm and blood pressure 92/40 mmHg. The patient had not undergone any major surgery/trauma, prolonged immobilization, and other high-risk factors for deep venous thrombosis recently. The patient had no family history of thrombotic events or known genetic coagulation disorders in the family. Arterial blood gas analysis showed that partial pressure of oxygen was 56 mmHg, partial pressure of carbon dioxide was 32 mmHg. Echocardiography revealed a mass arising from the main PA and extending into the right and left PAs. He had severe tricuspid regurgitation, right heart enlargement, and right ventricular systolic pressure of 65 mmHg. Computed tomographic angiography (CTA) of the chest had revealed a large filling defect within the main PA that extended into both right and left PAs, complicated by left pleural effusion and right heart enlargement. He had been treated with thrombolytic and anticoagulant agents without clinical improvement. After he transferred to our hospital for further evaluation and treatment, the decision was made to proceed with PA embolectomy.
After admission, the patient underwent related tests. The DIC revealed INR 1.27, D-dimer 1.57 μg/ml, fibrinogen degradation product (FDP) 8.7 μg/ml; troponin I 0.25 ng/ml; C-reactive protein 140.05 mg/L; γ-glutamyltransferase 235.9 KU/L; lactate dehydrogenase 331.24 U/L; α-hydroxybutyrate dehydrogenase 296 U/L; erythrocyte sedimentation rate 52 mm/h; brain natriuretic peptide 13.8 pg/ml. No significant abnormalities were found in other examinations. A repeat echocardiography revealed a mass arising from the main PA and extending into the right and left PAs with no change in size since the previous imaging exam (Figure 1). Left ventricular ejection fraction was 0.65, with severe tricuspid regurgitation, right heart enlargement, and right ventricular systolic pressure of 70 mmHg. The patient then underwent a chest CTA again at our hospital, revealing a filling defect within the lumen of the main PA, extending into both right and left PAS. There was no change between this and the previous CTA (Figure 2). There was no obvious abnormality on the electrocardiogram.
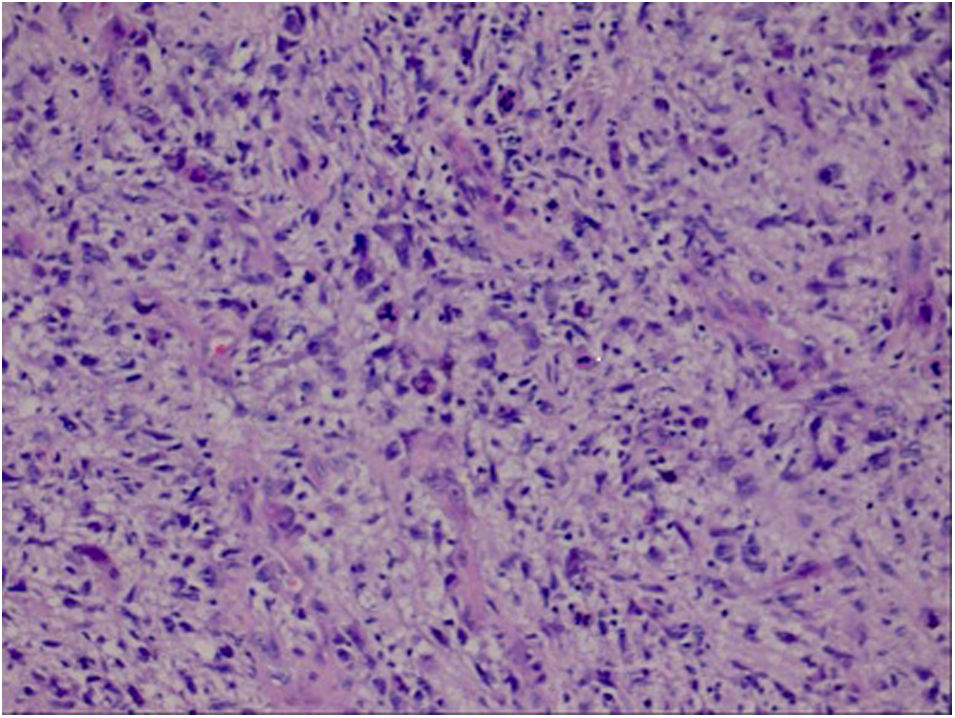
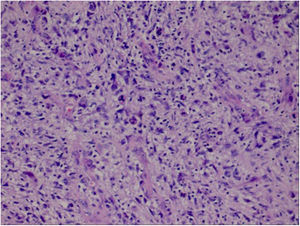
The PAS was resected under general anesthesia and cardiopulmonary bypass. The PA was incised longitudinally during the operation. The tumors were seen in the main trunk of the PA and the proximal end of the left and right PAs. The soft and easily exfoliated tissue was removed and the intima of the PA was stripped. Pathological examination of the PAS was performed. Immunohistochemical results revealed a malignant spindle cell tumor, PAS (Figure 3).
After an uneventful postoperative course, the patient was discharged from hospital on postoperative day 10. The patient was treated with regular chemotherapy after discharge. The patient was followed up by telephone for more than six months after discharge, in acceptable general condition. There were no symptoms of chest tightness, shortness of breath or heart failure. CTA revealed no obvious filling defect in the pulmonary artery.
DiscussionPulmonary artery sarcoma is a malignant disease originating from the intimal and mural portions of the PA. The exact incidence of PAS is unknown, ranging from 0.001% to 0.030%.1 To date, there have been few reports of the entity worldwide. Most patients are misdiagnosed as PE before surgery, the proper diagnosis is usually made during surgery or autopsy.2 This patient was misdiagnosed with PE before surgery and the diagnosis was confirmed by histopathological examination. The usual survival period is 12–18 months after the onset of symptoms.3 Prognosis primarily depends on whether there is recurrence or metastasis of the tumor. Tumor location can affect hemodynamics; therefore, it has a substantial influence on its course.4
The clinical manifestations of PAS are non-specific; therefore, early diagnosis is difficult. Lee found that the incidence was not easy to detect, primarily manifesting as shortness of breath, chest pain, cough, hemoptysis or blood in sputum and syncope, and some were even asymptomatic.5 This patient had progressive dyspnea and chest tightness (course of disease more than one month).
There are two types of PAS: intimal and mural. Intimal sarcoma has a polypoid pattern in the lumen, obstructing the lumen of the PA. Mural sarcoma is very rare and it differs from intimal sarcoma. According to the histological subtype, intimal sarcoma is a soft tissue sarcoma (leiomyosarcoma).6 Our patient's tumor was an intimal sarcoma that grew into the lumen, obstructing the PA and the Initial part of the left and right PAs. It is difficult to distinguish PAS from PA thrombosis on imaging data such as echocardiography and CT. PAS metastasizes early; therefore, PET/CT often shows signs of hypermetabolism in the thorax or other parts, and its standard uptake value is far greater than that of thrombus.7 However, no magnetic resonance imaging or PET/CT examination was performed in this patient. The patient was suspected to have PAS based on intraoperative findings and pathological examination.
Currently, surgery is considered to be the first and most effective treatment for PAS patients. Pulmonary artery endarterectomy is the preferred surgical procedure because it can preserve the function of the pulmonary vasculature and pulmonary tissue, relieving the symptoms of pulmonary hypertension and right ventricular insufficiency caused by tumor obstruction, even in cases of pulmonary artery obstruction. In the context of extensive metastasis of tumors, palliative treatment can also be provided to some extent.8 Pulmonary artery endarterectomy was adopted for this patient.
According to some studies, the average duration of survival of PAS patients without surgery is about one and a half months, while the average survival time of PAS patients who undergo surgery can be extended to more than 12 months.9 It has been reported that a PAS patient survived 36 months after adjuvant chemotherapy and radiotherapy.10 Our patient received regular chemotherapy immediately after operation. At present, six months post-operatively, no recurrences have occurred. This may suggest that the timely combination of radiotherapy and/or radiotherapy post-operatively can prolong life of these patients.
ConclusionsIn patients with progressive worsening of shortness of breath as the main manifestation and imaging findings of PA space-occupying lesions, there should be a suspicion of possible non-thrombotic diseases. When patients are misdiagnosed as PE, thrombolysis and anticoagulation therapy are often ineffective. Even after radical resection, the prognosis is usually unsatisfactory in PAS. Therefore, we must strive to choose a combination of less invasive surgery and postoperative radiotherapy and chemotherapy for these patients in order to improve their survival rates.
Ethical approvalThe study was approved by the ethics committee of the First Hospital of Lanzhou University, Lanzhou, China. The patient provided written informed consent.
Authors’ contributionsAll authors were involved in the treatment of patients. Xiaofang Yang participated in the writing and revising of the paper. Yuanmin Li reviewed the paper.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interestAll authors declare that they have no conflicts of interest to disclose.