The indiscriminate use of different diagnostic criteria for the definition of dyslipidemia may result in inaccurate interpretations, which could compromise diagnosis and therefore the therapeutic and prophylactic actions to be taken.
ObjectiveTo analyze possible differences in prevalence rates of dyslipidemia in adolescents based on three diagnostic definitions.
MethodsA cross-sectional study was conducted of a representative sample of Brazilian adolescents between 11 and 16 years of age. Blood samples were collected from 1000 students (423 boys and 577 girls) to determine fasting total cholesterol (TC), HDL and LDL cholesterol, and triglycerides (TG). The prevalence of dyslipidemia was established according to three definitions: those of the National Cholesterol Education Program (NCEP), the Brazilian Society of Cardiology (BSC), and the National Health and Nutrition Examination Survey (NHANES).
ResultsSignificant differences (p<0.01) were found between the diagnostic criteria for TC (BSC 38.3%; NCEP 11.2%; NHANES 4.8%), HDL cholesterol (BSC 30.0%; NCEP 15.8% NHANES 18.4%), LDL cholesterol (BSC and NCEP 10.8% and NHANES 5.9%), and TG (BSC and NCEP 4.7% and NHANES 1.3%). The overall prevalence of dyslipidemia was 61% (BSC), 28.6% (NCEP) and 24.2% (NHANES). Agreement rates varied significantly (kappa 0.15–0.90).
ConclusionsAlthough a high prevalence of dyslipidemia was observed in this study regardless of the diagnostic criteria used, the wide variation in rates highlights the need to establish a single definition with appropriate discriminatory power for adolescents.
O uso indiscriminado de diferentes critérios diagnósticos para a determinação de dislipidemias pode resultar em interpretações imprecisas, podendo comprometer o diagnóstico e, consequentemente, as ações terapêuticas e profiláticas a serem empregadas.
ObjetivoAnalisar possíveis diferenças nas taxas de prevalência de dislipidemias em adolescentes, com base em três critérios diagnósticos.
MétodosEstudo transversal conduzido com uma amostra representativa de adolescentes brasileiros de 11 a 16 anos. Amostras de sangue foram coletadas de 1000 escolares (423 rapazes e 577 moças) para determinação do colesterol total (CT), HDL, LDL e triglicérides (TG) em jejum. A prevalência de dislipidemias foi estabelecida com base em três critérios diagnósticos: National Cholesterol Education Program (NCEP), Sociedade Brasileira de Cardiologia (SBC) e National Health and Nutrition Examination Survey (NHANES).
ResultadosDiferenças significantes (p<0,01) foram identificadas entre os critérios diagnósticos analisados para CT (SBC=38,3%; NCEP=11,2%; NHANES=4,8%), HDL (SBC=30,0%; NCEP=15,8%; NHANES=18,4%), LDL (SBC/NCEP=10,8% e NHANES=5,9%) e TG (SBC/NCEP=4,7% e NHANES=1,3%). No geral, a prevalência de dislipidemias foi na ordem de 61% (SBC); 28,6% (NCEP) e 24,2% (NHANES). Os índices de concordância variaram amplamente (Kappa=0,15 a 0,90).
ConclusõesEmbora uma elevada prevalência de dislipidemias tenha sido identificada neste estudo, independente dos critérios diagnósticos utilizados, a ampla variação nas taxas encontradas reforça a necessidade do estabelecimento de um critério único e com poder de discriminação adequado para adolescentes.
Coronary artery disease is one of the leading causes of death worldwide,1,2 and dyslipidemia is one of its main risk factors.3,4 In adolescents, an increase in the prevalence of dyslipidemia has been observed in several studies, especially during the last decade.5–11 Thus, although it does not usually manifest in children and adolescents, the beginning of the atherosclerotic process may occur early at these stages of life.12–14
Dyslipidemia is characterized by disorders in lipid metabolism, which lead to changes in the serum levels of circulating lipids and lipoproteins,4,15 and its subclassifications are established by determining the concentrations of triglycerides (TG), total cholesterol (TC) and its high-density lipoprotein (HDL-C) and low-density lipoprotein (LDL-C) fractions. However, one of the main problems faced by researchers and health care professionals is the indiscriminate use of different criteria for the diagnosis of dyslipidemia, particularly in adolescents.
According to the National Cholesterol Education Program (NCEP),16 dyslipidemia is defined as HDL-C <40 mg/dl and TC, LDL-C and TG levels ≥200, ≥130 and ≥130 mg/dl, respectively. This recommendation was adopted as a reference for the Brazilian population until the middle of the last decade, with the support of the Brazilian Society of Cardiology (BSC).15 In 2005, the current NCEP definition was revised by the BSC, which proposed more stringent cutoff points for adolescents.17
However, none of the above cutoff points considered differences between the sexes, which are particularly important regarding the maturation process. A new proposal was therefore presented based on data from the National Health and Nutrition Examination Survey (NHANES), establishing cutoff points for TC, LDL-C, HDL-C and TG levels according to the variables of age and gender: for boys aged 12–16, 223–233 mg/dl for TC, 144–153 mg/dl for LDL-C and 163–195 mg/dl for TG; and for girls, 208–225 mg/dl, 136–145 mg/dl and 158–180 mg/dl for TC, LDL-C and TG, respectively. HDL-C only shows variation in boys, with values 39–46 mg/dl, for the age-group in question.18
Considering the cutoff points recommended by each definition (NCEP, BSC and NHANES), our hypothesis is that the adoption of different criteria may significantly affect the prevalence rates of dyslipidemia, as was observed in recent studies analyzing the impact of the use of different criteria for the classification of metabolic syndrome in Brazilian adolescents.19,20
We believe that clarifying these issues could be of importance for both researchers and health professionals, helping in the implementation of strategies to prevent and treat dyslipidemia in adolescence. Thus, the aim of the present study was to analyze possible differences in the prevalence rates of dyslipidemia in adolescents of both sexes, based on three diagnostic definitions.
MethodsThe present study was based on data from a school-based cross-sectional study on the prevalence of metabolic syndrome and cardiovascular risk factors in adolescents from the city of Londrina, Paraná state, Brazil, carried out during the school year 2011. Sample size was established using an equation based on population parameters,21 which indicated a minimum of 848 subjects, based on the mean prevalence of dyslipidemia of nearly 57% reported in national studies,6,7,10,14 sample error of 4%, power of 80%, statistical significance of 5% (z=1.96), design effect of 2.0, and increase of 20% to compensate for possible losses and refusals.
Participants were selected by a two-stage sampling process. Initially, 55 public schools were listed and grouped according to their geographical location (north, south, east, west, central, and peripheral belt), and two or three schools were then randomly selected in each of these regions. All classes from the 6th to the 9th grades of elementary education were listed, some of which were randomly selected to participate in the study. All students enrolled in the selected classes were invited to participate. Inclusion criteria were: (1) reported good health status (not frequently taking medication or being treated for disease) and (2) return of the consent form duly signed by students and their parents or guardians. Among the 1244 subjects eligible for the study, 1000 adolescents (57.7% female) aged between 11 and 16 years and with complete data on the variables under analysis comprised the study sample. The study was approved by the local research ethics committee (decision 238/2010).
Body weight and height were measured according to the procedures described in the literature.22 For determination of lipid profile, 14 ml of venous blood was collected into vacuum tubes with separator gel and without anticoagulant by venous puncture in the antecubital fossa at an adapted classroom in each of the schools, after a 12-hour fast prior to collection. Samples were collected and immediately stored at a temperature of 8°C. After one hour, all samples were centrifuged for 3000 rpm for 15 min and serum aliquots were stored at –70°C until assayed. Subsequently, TG, TC, HDL-C and LDL-C concentrations were determined using a Siemens Dade Behring Dimension RxL Max chemistry analyzer. Dyslipidemia and its subclassifications were diagnosed as abnormal serum levels of circulating lipids and lipoproteins, based on criteria from NCEP, BSC and NHANES.
Statistical analysisThe Kolmogorov–Smirnov test was initially used to analyze data distribution. Since the data showed normal distribution, the general characteristics of the sample were expressed as mean and standard deviation. The Kruskal-Wallis test followed by the Mann-Whitney test were used to compare lipid values between ages groups. McNemar's test was applied to compare prevalences between the different definitions of dyslipidemia. The kappa index was used to analyze agreement between the results obtained with the different diagnostic criteria. Statistical significance was set at p<0.05. All analyses were processed using the statistical package SPSS 17.0.
This study was partly funded by the Brazilian Council for Scientific and Technological Development (483867/2009-8).
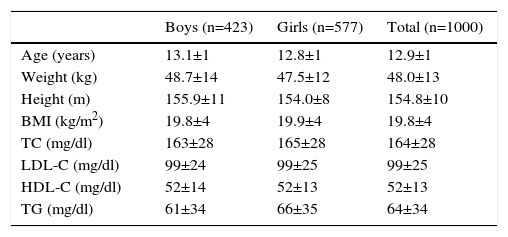
ResultsThe general characteristics of the sample stratified by gender are presented in Table 1.
General characteristics of the sample according to gender.
| Boys (n=423) | Girls (n=577) | Total (n=1000) | |
|---|---|---|---|
| Age (years) | 13.1±1 | 12.8±1 | 12.9±1 |
| Weight (kg) | 48.7±14 | 47.5±12 | 48.0±13 |
| Height (m) | 155.9±11 | 154.0±8 | 154.8±10 |
| BMI (kg/m2) | 19.8±4 | 19.9±4 | 19.8±4 |
| TC (mg/dl) | 163±28 | 165±28 | 164±28 |
| LDL-C (mg/dl) | 99±24 | 99±25 | 99±25 |
| HDL-C (mg/dl) | 52±14 | 52±13 | 52±13 |
| TG (mg/dl) | 61±34 | 66±35 | 64±34 |
BMI: body mass index; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides.
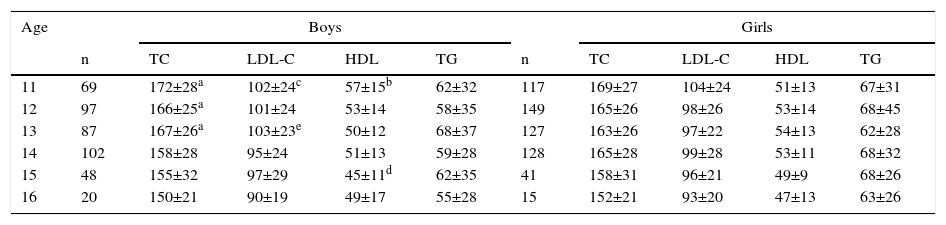
The age- and gender-stratified mean values for lipid profile are presented in Table 2. No significant differences were observed for the different ages in the female group. However, in the male group, adolescents aged 11 years had a mean TC concentration of 172 mg/dl, which was significantly higher than that for age 14 (p<0.05). Furthermore, mean HDL-C was also higher in boys aged 11 years compared to 13 and 15 years (p<0.05).
Mean values and standard deviations of total cholesterol, LDL cholesterol, HDL cholesterol and triglycerides according to age and gender.
| Age | Boys | Girls | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | TC | LDL-C | HDL | TG | n | TC | LDL-C | HDL | TG | |
| 11 | 69 | 172±28a | 102±24c | 57±15b | 62±32 | 117 | 169±27 | 104±24 | 51±13 | 67±31 |
| 12 | 97 | 166±25a | 101±24 | 53±14 | 58±35 | 149 | 165±26 | 98±26 | 53±14 | 68±45 |
| 13 | 87 | 167±26a | 103±23e | 50±12 | 68±37 | 127 | 163±26 | 97±22 | 54±13 | 62±28 |
| 14 | 102 | 158±28 | 95±24 | 51±13 | 59±28 | 128 | 165±28 | 99±28 | 53±11 | 68±32 |
| 15 | 48 | 155±32 | 97±29 | 45±11d | 62±35 | 41 | 158±31 | 96±21 | 49±9 | 68±26 |
| 16 | 20 | 150±21 | 90±19 | 49±17 | 55±28 | 15 | 152±21 | 93±20 | 47±13 | 63±26 |
LDL-C: low-density lipoprotein cholesterol; HDL: high-density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides.
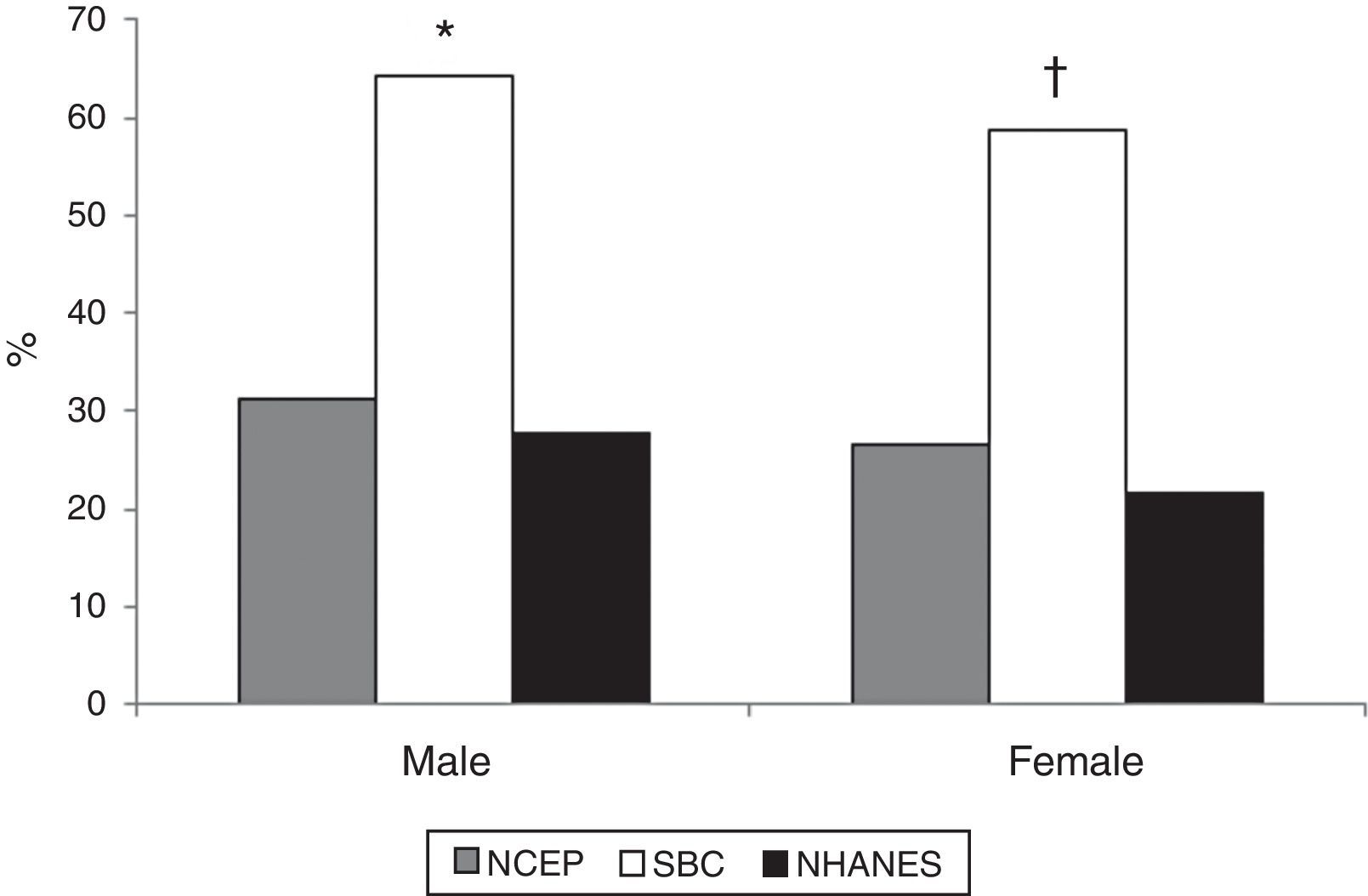
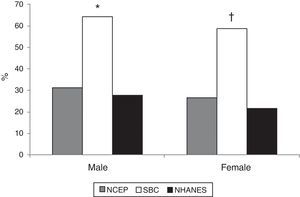
Figure 1 shows prevalences according to gender. The overall prevalence of dyslipidemia ranged from 24.2% (NHANES) to 61% (BSC). Smaller differences (4.4%) were seen in the comparison between the internationally used definitions (NHANES and NCEP). Significant differences (p<0.05) were observed in the female group with regard to the three definitions, while in the male group differences were limited to comparison between the BSC definition and the other definitions (p<0.05).
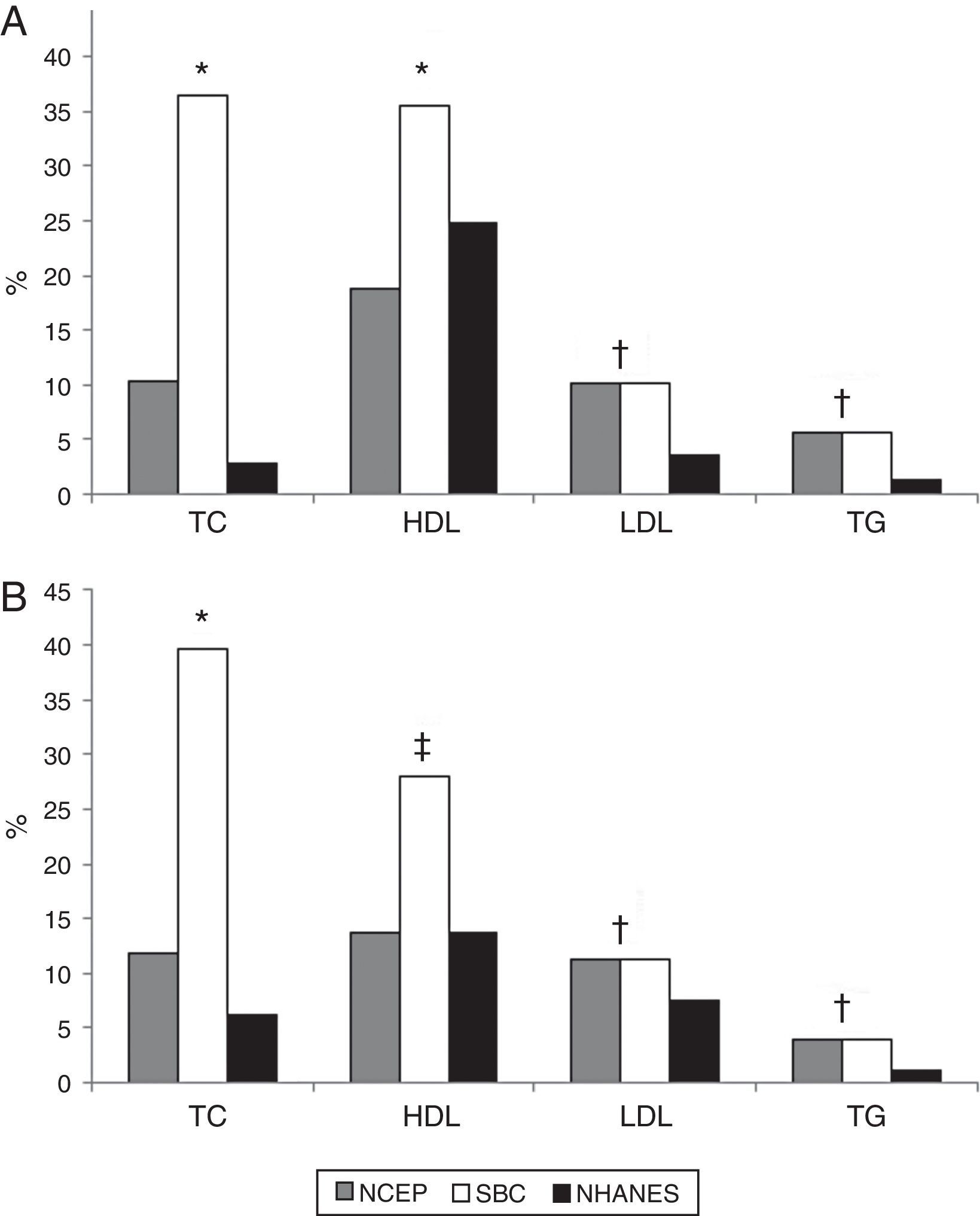
As for dyslipidemia subclassifications (Figure 2), the prevalence rates based on information obtained from the three definitions also varied considerably, regardless of gender, especially those for TC (BSC 38.3%; NCEP 11.2%; NHANES 4.8%) and HDL-C (BSC 30.0%; NCEP 15.8%; NHANES 18.4%). As for LDL-C and TG, the cutoff points for which by BSC and NCEP were similar, the prevalence rates were 10.8% vs. 5.9% (LDL-C) and 4.7% vs. 1.3% (TG) for BSC and NCEP and NHANES, respectively.
Prevalence of dyslipidemia subclassifications in male (A) (n=423) and female (B) (n=577) adolescents, according to the three diagnostic definitions. HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides. * p<0.05 (BSC≠NCEP≠NHANES); † p<0.05 (BSC=NCEP>NHANES); ‡ p<0.05 (BSC>NCEP=NHANES).
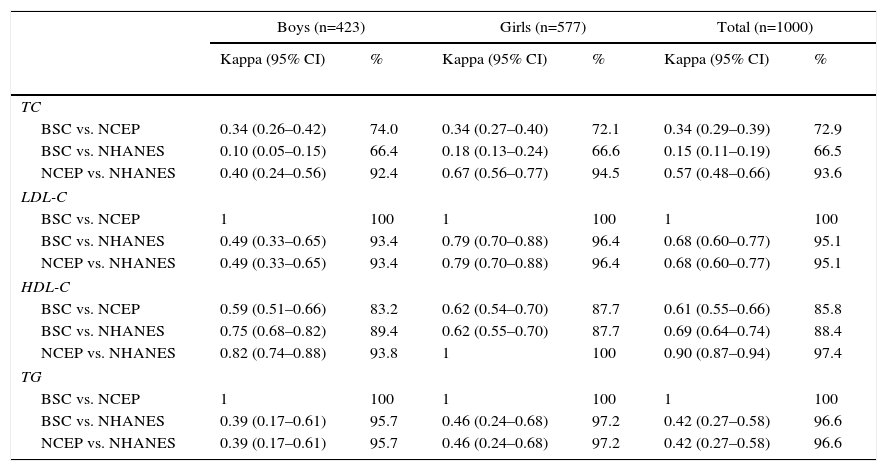
Table 2 displays agreement indicators for the different definitions. In general, although relative agreement was higher than 70% in most cases, kappa coefficients showed mostly low to moderate agreement (Table 3).
Analysis of agreement between the three diagnostic definitions used to assess the prevalence of dyslipidemia in adolescents.
| Boys (n=423) | Girls (n=577) | Total (n=1000) | ||||
|---|---|---|---|---|---|---|
| Kappa (95% CI) | % | Kappa (95% CI) | % | Kappa (95% CI) | % | |
| TC | ||||||
| BSC vs. NCEP | 0.34 (0.26–0.42) | 74.0 | 0.34 (0.27–0.40) | 72.1 | 0.34 (0.29–0.39) | 72.9 |
| BSC vs. NHANES | 0.10 (0.05–0.15) | 66.4 | 0.18 (0.13–0.24) | 66.6 | 0.15 (0.11–0.19) | 66.5 |
| NCEP vs. NHANES | 0.40 (0.24–0.56) | 92.4 | 0.67 (0.56–0.77) | 94.5 | 0.57 (0.48–0.66) | 93.6 |
| LDL-C | ||||||
| BSC vs. NCEP | 1 | 100 | 1 | 100 | 1 | 100 |
| BSC vs. NHANES | 0.49 (0.33–0.65) | 93.4 | 0.79 (0.70–0.88) | 96.4 | 0.68 (0.60–0.77) | 95.1 |
| NCEP vs. NHANES | 0.49 (0.33–0.65) | 93.4 | 0.79 (0.70–0.88) | 96.4 | 0.68 (0.60–0.77) | 95.1 |
| HDL-C | ||||||
| BSC vs. NCEP | 0.59 (0.51–0.66) | 83.2 | 0.62 (0.54–0.70) | 87.7 | 0.61 (0.55–0.66) | 85.8 |
| BSC vs. NHANES | 0.75 (0.68–0.82) | 89.4 | 0.62 (0.55–0.70) | 87.7 | 0.69 (0.64–0.74) | 88.4 |
| NCEP vs. NHANES | 0.82 (0.74–0.88) | 93.8 | 1 | 100 | 0.90 (0.87–0.94) | 97.4 |
| TG | ||||||
| BSC vs. NCEP | 1 | 100 | 1 | 100 | 1 | 100 |
| BSC vs. NHANES | 0.39 (0.17–0.61) | 95.7 | 0.46 (0.24–0.68) | 97.2 | 0.42 (0.27–0.58) | 96.6 |
| NCEP vs. NHANES | 0.39 (0.17–0.61) | 95.7 | 0.46 (0.24–0.68) | 97.2 | 0.42 (0.27–0.58) | 96.6 |
All kappa coefficients were significant (p<0.01). BSC: Brazilian Society of Cardiology; CI: confidence interval; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; NCEP: National Cholesterol Education Program; NHANES: National Health and Nutrition Examination Survey; TC: total cholesterol; TG: triglycerides.
The results of this study indicate that the indiscriminate use of different diagnostic criteria for the identification of dyslipidemia and its subclassifications in adolescents may lead to doubtful interpretations. Thus, of the 610 adolescents classified as dyslipidemic by the BSC (61%), only 286 received the same classification by NCEP (28.6%) and 242 by NHANES (24.2%). It should be noted that, in the present sample, the adoption of the international definitions would result in a false negative rate of nearly 35% according to the criteria of the BSC. Therefore, the lack of a single definition with appropriate discriminatory power may compromise both analysis of the prevalence rates of dyslipidemia in this population and decision-making for the implementation of therapeutic or prophylactic interventions.
Two previous studies7,23 analyzed the prevalence of dyslipidemia in a sample of children and adolescents based on the NCEP and BSC definitions. In the first23 the prevalence of dyslipidemia in private and public school students aged 5–16 years was 23% and 4%, respectively (NCEP definition) and 49% and 14%, respectively (BSC definition). In the second study,7 in which the sample consisted of children aged 5–9 years, the differences between the two definitions were smaller, while the prevalence rates were higher (NCEP 64.5% and BSC 68.4%). Thus, similarly to the present study, the BSC definition found a higher prevalence of dyslipidemia than the NCEP definition. However, the differences between the two criteria were greater in the present study, which can be explained at least in part by the different characteristics of the samples analyzed, including sample size, age and maturational status.
When analysis of the information obtained in this study was extended to dyslipidemia subclassifications, we found that, regardless of gender, high TC was the most frequent form of dyslipidemia according to the BSC definition, whereas low HDL-C was the predominant anomaly based on the NHANES and NCEP definitions. Of studies that adopted the BSC definition for the diagnosis of dyslipidemia in Brazilian adolescents, this appears to be the first to identify high TC as the predominant form of dyslipidemia, unlike other studies, in which high TG24 and low HDL-C7,25–27 were the main lipid anomalies.
The findings from the present study are of concern, since there is a continuous increase in cardiovascular risk with TC values higher than 180 mg/dl; it is thus important for health prevention that cutoff points remain below this value.28 On this basis, the cutoff points proposed by the BSC definition are perhaps the most appropriate for the diagnosis of dyslipidemia in adolescents.
On the other hand, other studies with adolescents based on the NCEP definition found that the predominant forms of dyslipidemia were high TC,28,29 high TG,3,4,9,30,31 and low HDL-C.6,10,32–34 Therefore, depending on the cutoff point adopted and on the specific characteristics of the sample analyzed (socioeconomic level, nutritional status, maturational level, etc.), identification of the predominant form of dyslipidemia can change.
Furthermore, since the cutoff points proposed by the NCEP require upgrading35 and changes in lipid levels during adolescence are dependent on age and maturity36 and show wide variations between sexes, the use of fixed cutoff points may be inappropriate in this age-group. In fact, when the mean lipid profile values of adolescents were compared in this study, it was observed that younger boys have higher TC and HDL-C than older boys. However, this was not observed in girls. Our results thus confirmed a gender-based difference.
In addition, there appears to be a need for tables with specific cutoff points for each population, since besides the different behavior between the sexes, variables of the lipid profile may be influenced by race and ethnicity.37,38 Furthermore, when the lipid profile values in this study were compared to the other studies described above,31,38 we identified differences in TC, with the highest values in Brazilian adolescents aged 11–15 years of both sexes. On the other hand, mean TG values were lower than those described by Yang et al.31 at all ages analyzed.
Considering that therapeutic or prophylactic measures should be implemented based on the categorization identified by the criteria adopted, inaccurate diagnosis can result in ineffective strategies. For example, in cases or populations in which low HDL-C is found as the predominant dyslipidemic subclass, increases in levels of physical activity and engagement in exercise programs may play a more important role than the adoption of other strategies for controlling other lipid alterations.
Some important limitations of the present study should be pointed out, such as the lack of a gold standard for comparison between the different criteria, which would be essential for sensitivity and specificity analysis. Moreover, there was no control for the maturational process, which could have provided valuable information for better stratification of the sample and extrapolation of the results. Additionally, although this is a school-based population study, generalization of the results is limited by the impact of the socioeconomic and cultural context on the behavior of the variables analyzed. Finally, the criteria analyzed were established on the basis of characteristics of other populations, at a different time, which also reduces the ecological validity of the present investigation.
In conclusion, the dyslipidemia prevalence rates found in adolescents of both genders in the present study were very high, despite the differences in the estimates obtained by the different definitions analyzed. The BSC definition, with its more stringent cutoff points, was the one that detected the highest rates, regardless of gender and the different dyslipidemia subclassifications. Finally, the results of the present study suggest that the indiscriminate use of different diagnostic criteria to estimate the prevalence of dyslipidemia in adolescents may result in inaccurate interpretations, which could compromise diagnosis and therefore the therapeutic and prophylactic measures to be taken.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the participants who voluntarily contributed to this study, the Local Education Authority of the city of Londrina, Brazil, and the 10 public schools which made this entire project possible. This study was supported (Process 483867/2009-8) by the Council for Scientific and Technological Development (CNPq/Brazil). The authors E.R.V.R. and D.P.R.S. were supported by the CNPq and E.S.C. was supported by the Coordination of Improvement of Higher Education Personnel (CAPES/Brazil).