Arterial switch operation (ASO) is currently the standard surgical repair for D-transposition of great arteries (D-TGA). As the procedure implies reimplantation of the coronary arteries into the neo-aortic root, long-term coronary complications are possible and potentially dangerous. However, routine coronary evaluation after ASO remains controversial. The purpose of this study is to perform a descriptive analysis of coronary computed tomography angiography (CCTA) findings in adolescent and young adults with D-TGA after ASO.
MethodsWe performed a retrospective single center study that included adolescent and young adults with D-TGA submitted to ASO who underwent CCTA. Demographic, clinical and imaging data were collected.
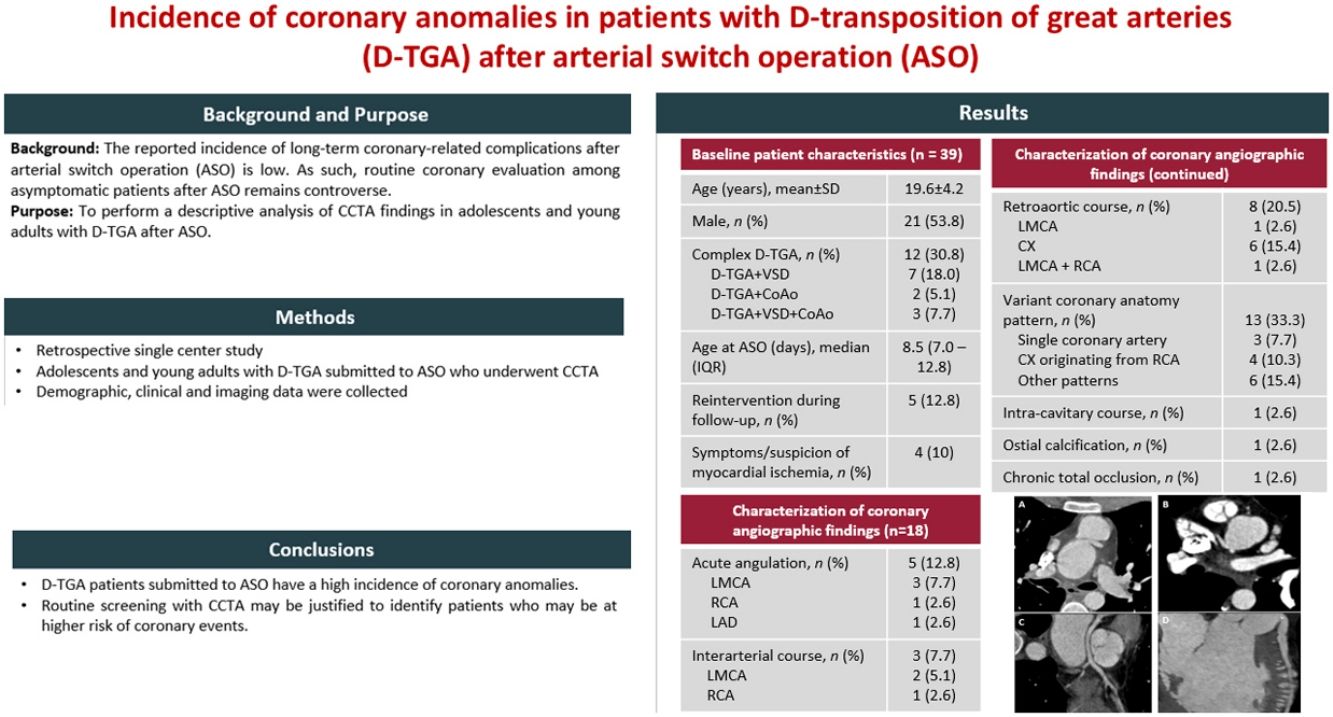
ResultsWe identified 57 patients with D-TGA submitted to ASO. Of these, 39 performed a CCTA. Mean age of patients was 19.6 (±4.2) years; 54% were male; 32% had complex D-TGA. In 35 patients (90%), CCTA was part of routine screening. In four (10%) patients CCTA was done due to symptoms or an abnormal non-invasive test suggestive of myocardial ischemia. Eighteen (46%) patients had coronary anomalies: five (13%) had an acute angulation at the coronary origin; 13 (33%) patients had anomalous origin of the coronary arteries. Interarterial course was described in two (5%) patients and retroaortic course reported in eight (21%) cases.
ConclusionsAdolescent and young adults with D-TGA submitted to ASO have a high incidence of coronary anomalies. Routine screening with CCTA may be justified to identify patients who may be at higher risk of coronary events.
A cirurgia de switch arterial é atualmente a técnica de cirúrgica de eleição para a reparação da dextro transposição das grandes artérias (D-TGA). Como o procedimento implica reimplantação das artérias coronárias na raiz neoaórtica, as complicações coronárias a longo prazo são um cenário possível e potencialmente grave. No entanto, a avaliação coronária por rotina após switch arterial permanece controversa. O objetivo deste estudo é realizar uma análise descritiva dos achados da angiografia por tomografia computadorizada coronária (CCTA) em adolescentes e jovens adultos com D-TGA corrigida com switch arterial.
MétodosRealizámos um estudo retrospetivo de centro único que incluiu adolescentes e adultos jovens com D-TGA corrigida com cirurgia de switch arterial que realizaram CCTA. Foram analisados dados demográficos, clínicos e imagiológicos.
ResultadosIdentificámos 57 doentes com D-TGA corrigida com switch arterial. Destes, 39 tinham avaliação por CCTA. Os doentes tinham em média 19.6 (±4.2) anos; 54% eram do sexo masculino; 32% tinham D-TGA complexa. Em 35 doentes (90%), a CCTA fez parte de uma avaliação por rotina. Em 4 (10%) dos doentes, foi feita por suspeita de isquemia miocárdica. Dezoito (46%) doentes tinham anomalias coronárias descritas: 5 (13%) tinham angulação aguda proximal; 13 (33%) tinham origem anómala. Dois (5%) tinham descrição de trajeto inter-arterial e 8 (21%) trajeto retro-aórtico.
ConclusãoAdolescentes e adultos jovens com D-TGA corrigida com switch arterial apresentam uma elevada prevalência de anomalias coronárias, o que pode justificar rastreio por rotina com CCTA de forma a identificar doentes com maior risco de eventos coronários.
D-loop TGA (D-TGA) is a complex congenital cardiac defect defined by atrioventricular concordance and ventricular-arterial discordance. Without correction, outcomes are poor, and most patients do not reach adulthood.1
Surgical methods for correction of the anomaly have evolved over time. Currently, the arterial switch operation (ASO) is the procedure of choice.2
This technique involves transection of the great arteries above the sinuses and translocation of the vessels to the opposite root, creating ventriculoarterial concordance. Reimplantation of the coronary arteries from the aorta into the neo-aortic root is a critical step during the procedure.
Overall perioperative mortality is low and long-term survival is excellent so far, with over 95% of patients reaching adulthood.3,4
Possible long-term complications include neo-aortic root dilation with resulting aortic regurgitation; supravalvular pulmonary stenosis and stenosis of the pulmonary branches, secondary to the Lecompte maneuver and dilation of the neo-aorta; and acute angulation with consequent obstruction and hypertension.1
Due to the nature of the procedure, coronary complications following ASO are also possible. Coronary events are an important cause of death, particularly early after the procedure.5 Late coronary stenosis are reported in 8–10% of cases, and a recent systematic review reported a prevalence of coronary anomalies in 23% of patients >20 years.2,5–8 These may result from ostial fibrosis at the suture lines, stretching and kinking due to the spatial rearrangement of the great arteries that occurs during growth, and extrinsic compression. Altered flow dynamics may predispose patients to developing atherosclerotic coronary artery disease.9
There is no consensus regarding postoperative evaluation of coronary abnormalities, particularly in asymptomatic patients.1,10 Non-invasive stress testing and coronary angiography are frequently used, but do not allow evaluation of the spatial relation between the coronary arteries and adjacent structures.
Recently, coronary computed tomography angiography (CCTA) has gained a prominent role in the evaluation of these patients, as it provides detailed characterization of the coronary anatomy and allows visualization of the course of the coronary arteries in relation to the great vessels.
However, recent studies report a low incidence of late coronary-related problems in asymptomatic patients after ASO, which leads us to question the value of routine coronary imaging in these patients.11
As such, there remains some controversy regarding the value of routine coronary evaluation among patients who undergo ASO.
ObjectivesThe objective of this study was to perform a descriptive analysis of the CCTA findings in adolescent and young adult patients with D-TGA after ASO.
MethodsWe conducted a retrospective single center cohort study that included adolescent (≥10 years) and young adults with D-TGA who had an ASO and underwent CCTA in our hospital between 2015 and 2022.
Data on demography, clinical features and CCTA results regarding coronary morphology and its relationship to the surrounding structures were collected from in-hospital and clinical records.
All examinations were performed using a dual-source CT scanner (SOMATON Definition Flash, Siemens). In all cases, prospective gating was used. All patients were in sinus rhythm. If appropriate, metoprolol (oral or intravenous) was administered before CT examination with the aim of lowering resting heart rate to less than 65 beats/min. Sublingual nitrates (5 mg) were administered in all patients.
CT scanning was performed with intravenous contrast enhancement, with iodine contrast agent being injected (Ultravist 370 mg/mL, 1 mL/kg, at a rate of 5 mL/s) with a power injector, followed by a chaser bolus of 40 mL saline into a peripheral vein.
Image analysis was performed by two experienced observers in consensus on a dedicated workstation.
Coronary lesions were described in accordance with the existing literature regarding patients with D-TGA after ASO.12,13
Acute proximal angulation of a coronary artery was reported based on the presence of an angulation of 30 degrees or less. Interarterial course was described when any part of the coronary artery had a pattern between the pulmonary trunk and aorta.
Statistical analysisContinuous variables are shown as mean±standard deviation and/or medians with interquartile ranges (IQR) as appropriate. Discrete variables were expressed as numbers or percentages. All statistical analyses were performed using the SPSS software (version 25.0, SPSS Inc., Chicago, Illinois).
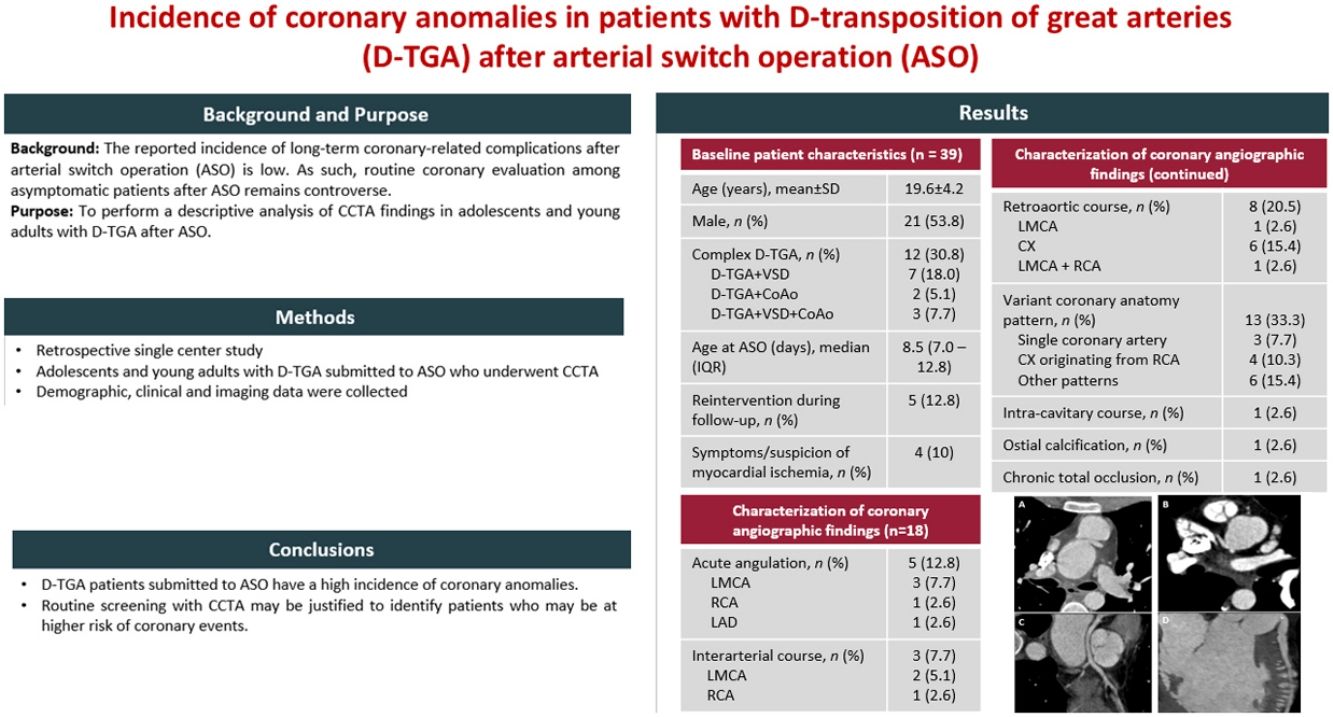
ResultsDuring the period of the study, we identified a total of 57 patients with D-TGA corrected with ASO. Of these, 39 underwent CCTA. Demographic data are reported in Table 1. The mean age of patients at the time of CCTA was 19.6 (±4.2) years (range 11–28 years). Thirty-four (87%) patients were 18 years or older; and twenty-one (54%) were male. Twenty-seven (69%) had simple D-TGA and 12 (32%) had complex D-TGA. Of these, seven had ventricular septal defect; two had coarctation of the aorta (CoAo) and three patients had both defects associated. Arterial switch was performed after a median age of 8.5 days (IQR 7.0–12.8). Nine (23%) patients underwent atrial septostomy prior to correction. In one of these, a modified Blalock-Taussig shunt was created before correction with ASO. One patient underwent myocardial revascularization with creation of an anastomosis from the left internal mammary artery to the left anterior descending artery.
Baseline demographic and clinical characteristics of patients.
| Variable | Patients (n=39) |
|---|---|
| Age in years, mean±SD | 19.6 (4.2) |
| Male, n (%) | 21 (53.8) |
| Complex D-TGA | 12 (30.8) |
| VSD | 7 (18.0) |
| CoAo | 2 (5.1) |
| VSD and CoAo | 3 (7.7) |
| Age in days at ASO, median (IQR) | 8.5 (7.0–12.8) |
| Atrial septostomy prior to correction, n (%) | 9 (23.1) |
| Reintervention during follow-up, n (%) | 5 (12.8) |
| Percutaneous pulmonary angioplasty | 3 (7.7) |
| Surgical widening of the main PA | 1 (2.6) |
| Surgical correction of CoAo | 1 (2.6) |
ASO: arterial switch operation; CoAo: coarctation of the aorta; IQR: interquartile range; PA: pulmonary artery; VSD: ventricular septal defect.
During clinical follow-up, five (13%) patients were reinterventioned: three underwent percutaneous pulmonary angioplasty because of severe supravalvular pulmonary stenosis; one underwent surgical widening of the main pulmonary artery; and one underwent surgical correction of CoAo.
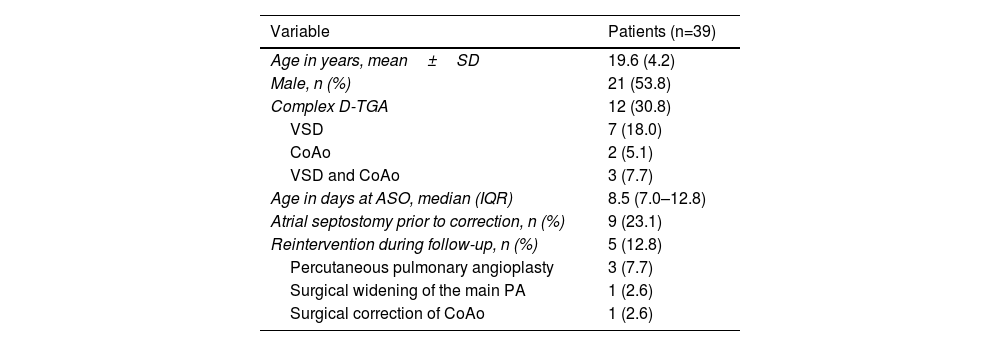
CCTA was performed in 35 patients (90%) as part of a routine screening. In four patients (10%), CCTA was done due to symptoms or an abnormal non-invasive test suggestive of myocardial ischemia. Regarding the coronary findings, 18 (46%) patients had reported coronary anomalies (Table 2).
Characterization of coronary angiographic findings.
| Coronary anomaly | Patients (n=39) |
|---|---|
| Acute angulation, n (%) | 5 (12.8) |
| LMCA | 3 (7.7) |
| RCA | 1 (2.6) |
| LAD | 1 (2.6) |
| Interarterial course, n (%) | 3 (7.7) |
| LMCA | 2 (5.1) |
| RCA | 1 (2.6) |
| Retroaortic course, n (%) | 8 (20.5) |
| LMCA | 1 (2.6) |
| CX | 6 (15.4) |
| LMCA+RCA | 1 (2.6) |
| Variant coronary anatomy pattern, n (%) | 13 (33.3) |
| Single coronary artery | 3 (7.7) |
| CX originating from RCA | 4 (10.3) |
| LMCA and RCA originating from anterior SOV | 2 (5.1) |
| LMCA and RCA originating from rightward SOV | 1 (2.6) |
| CX and RCA originating from rightward SOV | 2 (5.1) |
| LAD, RCA and CX originating from anterior SOV, with common origin of the LAD and RCA and independent origin of CX | 1 (2.6) |
| Intra-cavitary course*, n (%) | 1 (2.6) |
| Ostial calcification*, n (%) | 1 (2.6) |
| Chronic total occlusion*, n (%) | 1 (2.6) |
CX: circumflex artery; LAD: left anterior descending artery; LMCA: left main coronary artery; RCA: right coronary artery; SOV: sinus of Valsalva.
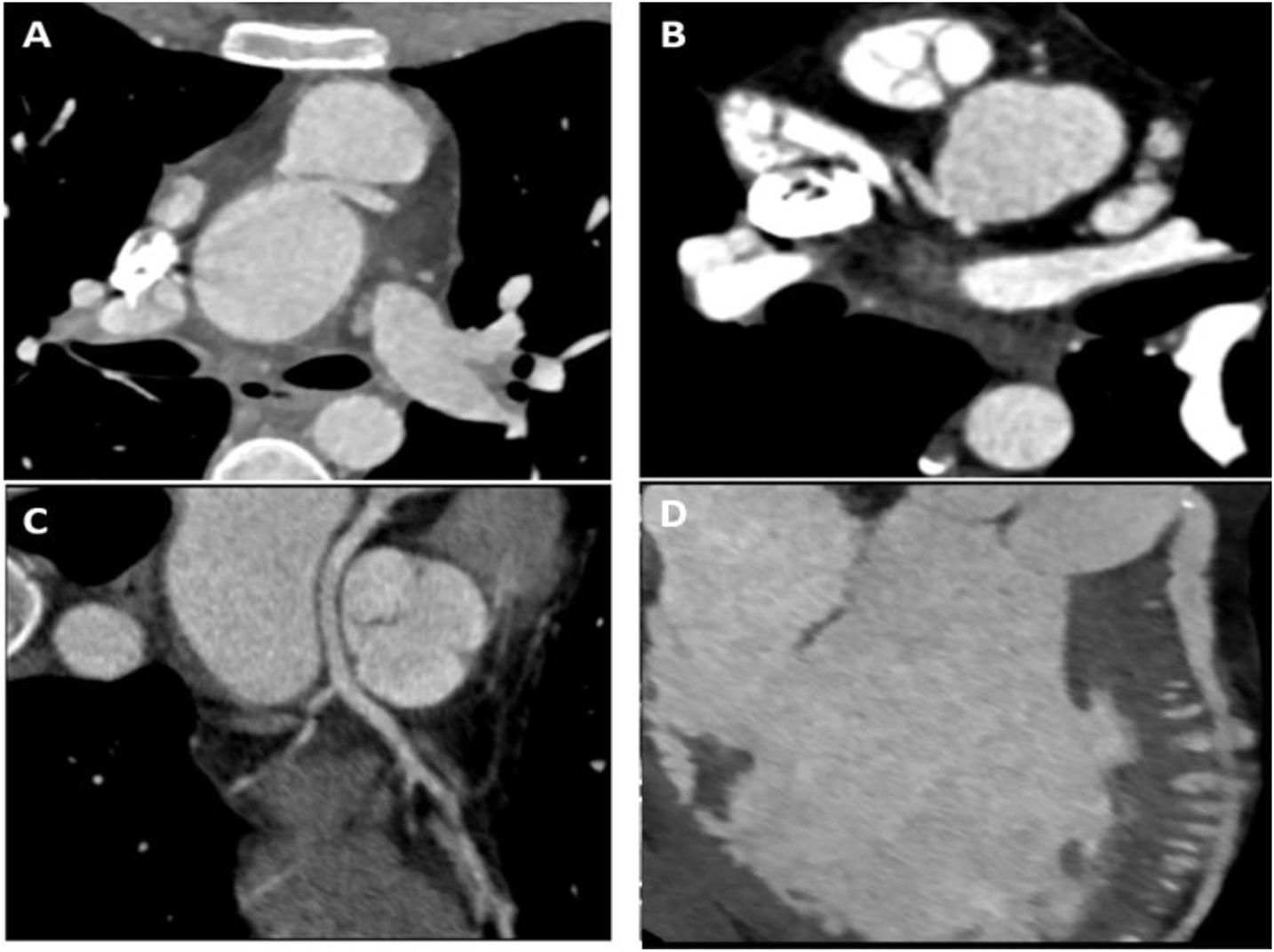
Five (13%) had acute angulation at the coronary origin (Figure 1A): three at the ostium of the left main coronary artery (LMCA); one at the ostium of the right coronary artery (RCA); and one at the ostium of the left anterior descending artery (LAD) which originated directly from the aorta.
Case examples of patients with abnormal coronary findings on computed tomographic coronary angiography. (A) Interarterial course of the left main coronary artery with acute angulation at the ostium. (B) Variant coronary anatomy pattern with both the left main coronary artery and right coronary artery originating from a rightward SOV. (C) Multiplanar reconstruction showing retroaortic course of the left anterior descending artery in a patient with a single coronary artery originating from a rightward sinus of Valsalva. (D) Multiplanar reconstruction of the left anterior descending artery showing intracavitary course into the right ventricle.
Thirteen (33%) patients had variant coronary anatomy patterns: three (8%) patients had a single coronary artery; six (15%) patients had anomalous origin at the sinus of Valsalva (SOV) (Figure 1B); and four (10%) patients had anomalous origin of the circumflex artery (CX) from the RCA.
Interarterial course was described in three (8%) patients – two of the LMCA and one of the RCA. None had evidence of extrinsic compression at rest. Retroaortic course was reported in eight (21%) cases. Of these, six were due to anomalous origin of the CX (four from the RCA, one from a rightward SOV and one from an anterior SOV). One case had a single coronary artery originating from a rightward SOV and the LAD had a retroaortic course (Figure 1C). The other patient had anomalous origin of the LMCA and RCA from a rightward SOV (with both arteries describing a retroaortic course). One patient had anomalous course of the LAD into the right ventricle (Figure 1D), a mild calcified ostial stenosis of the LMCA and chronic total occlusion of the RCA.
Among patients with coronary anomalies identified, only two of them were symptomatic (atypical chest pain). One had a common origin of the LMCA and RCA from the posterior aspect of the aorta, with a short retroaortic course of both arteries. Dobutamine stress echocardiogram was performed and did not show evidence of myocardial ischemia. The other patient had a single coronary artery: as symptoms were highly atypical, no further evaluation was performed. Regarding asymptomatic cases, 10 (55%) patients had non-invasive stress testing performed. No cases had evidence of myocardial ischemia. One asymptomatic patient underwent CCTA because of a positive electrocardiographic stress test. This patient had a single coronary artery with no evidence of stenosis or extrinsic compression and was not submitted to further evaluation. One patient with anomalous course of the LAD into the right ventricle and chronic total occlusion of the RCA was asymptomatic and had no evidence of ischemia on non-invasive testing.
DiscussionThis study demonstrated a high incidence of coronary anomalies among D-TGA patients who underwent ASO. These included congenital anomalies such as an anomalous origin of the CX from the RCA, the presence of a single coronary artery, or an intracavitary course. Acquired anomalies were also identified, such as the presence of acute proximal angulation, interarterial and retroaortic courses, and calcified ostial stenosis. The prevalence of these anomalies is in line with previous studies.14,15
These findings were not associated with symptoms or myocardial ischemia, and their clinical short- and long-term significance remains uncertain. Dilation of the neoaortic root is a well-known complication late after ASO. Some authors hypothesize that this progressive dilation could contribute to the development of acute angulation of a coronary origin in some cases.15 Aortic dilation may also be relevant among patients with interarterial course, as it can lead to extrinsic compression. The presence of an anomalous course may also have an impact on future surgical or percutaneous cardiac interventions.
There is currently no consensus regarding routine screening for coronary artery disease after ASO. Recent studies report a low incidence of sudden cardiac death or myocardial ischemia late after surgery.11,16 We believe that these results should be interpreted with caution, as long-term follow-up data are scarce. Accordingly, CCTA may be useful to identify individuals who may be at risk of coronary complications in the long term, particularly patients with acute proximal angulation and interarterial course, a subset of patients at risk of sudden cardiac death who may not be identified through functional testing and may benefit from specific lifestyle changes, closer follow-up, and surgical treatment in selected cases. It should be noted that patients with coronary artery stenosis or compression may be asymptomatic due to cardiac denervation after dissection of the cardiac plexus during ASO.17 Notably, none of the findings in our cohort of patients motivated immediate action to address the underlying anomaly. This may reflect the clinical uncertainty surrounding these findings, which should be acknowledged given the lack of longitudinal follow-up data.
LimitationsThis was a small single-center retrospective observational study inherently susceptible to biases, limiting the generalizability of the findings. Importantly, patients with typical symptoms or high-risk presentation (e.g., sudden cardiac death) may not have undergone CCTA, which may have resulted in underestimation of the prevalence of high-risk anomalies.
We did not have access to preoperative coronary anatomy and procedural data, which limits the contextualization of the coronary anomalies found.
ConclusionCoronary anomalies are frequent findings late after ASO in patients with D-TGA. However, the clinical relevance of these findings remains uncertain. While routine CCTA screening may be justified for identifying patients with potentially high-risk features, the long-term implications for clinical management are not fully understood. Multicentric longitudinal studies are crucial to better define the prognostic relevance of these anomalies and their impact on patient outcomes.
Ethical approvalNone declared.
FundingNone to declare.
Conflicts of interestThe authors have no conflicts of interest to disclose.