Obstructive coronary artery disease (CAD) remains the most common etiology of heart failure with reduced ejection fraction (HFrEF). However, there is controversy whether invasive coronary angiography (ICA) should be used initially to exclude CAD in patients presenting with new-onset HFrEF of unknown etiology. Our study aimed to develop a clinical score to quantify the risk of obstructive CAD in these patients.
MethodsWe performed a cross-sectional observational study of 452 consecutive patients presenting with new-onset HFrEF of unknown etiology undergoing elective ICA in one academic center, between January 2005 and December 2019. Independent predictors for obstructive CAD were identified. A risk score was developed using multivariate logistic regression of designated variables. The accuracy and discriminative power of the predictive model were assessed.
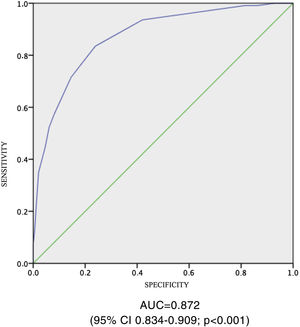
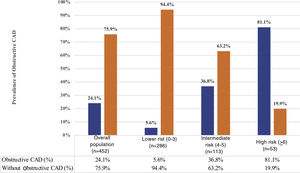
ResultsA total of 109 patients (24.1%) presented obstructive CAD. Six independent predictors were identified and included in the score: male gender (2 points), diabetes (1 point), dyslipidemia (1 point), smoking (1 point), peripheral arterial disease (1 point), and regional wall motion abnormalities (3 points). Patients with a score ≤3 had less than 15% predicted probability of obstructive CAD. Our score showed good discriminative power (C-statistic 0.872; 95% CI 0.834–0.909: p<0.001) and calibration (p=0.333 from the goodness-of-fit test).
ConclusionsA simple clinical score showed the ability to predict the risk of obstructive CAD in patients presenting with new-onset HFrEF of unknown etiology and may guide the clinician in selecting the most appropriate diagnostic modality for the assessment of obstructive CAD.
A doença arterial coronária (DAC) obstrutiva constitui a principal etiologia da insuficiência cardíaca com fração de ejeção reduzida (IC-FER). No entanto, é controverso se a angiografia coronária (AC) deve ser utilizada como primeira linha na exclusão de DAC em doentes que se apresentem com IC-FER «de novo». O nosso estudo teve por objetivo desenvolver um score clínico para quantificar o risco de DAC obstrutiva neste grupo de doentes.
MétodosEstudo transversal, incluindo 452 doentes com IC «de novo» de causa não estabelecida submetidos a AC eletiva num centro terciário, entre janeiro de 2005 e dezembro de 2019. Foram identificados preditores independentes para DAC obstrutiva. Foi desenvolvido um score de risco através de um modelo de regressão logística utilizando as variáveis identificadas. A acuidade e o poder discriminativo do score foram avaliados.
ResultadosApresentavam DAC obstrutiva 109 pacientes (24,1%). Seis preditores independentes foram identificados e incluídos no modelo: sexo masculino (2 pontos), diabetes mellitus (1 ponto), dislipidémia (1 ponto), tabagismo (1 ponto), doença arterial periférica (1 ponto) e presença de alterações segmentares no ecocardiograma (3 pontos). Os pacientes com um score -3 apresentaram uma probabilidade prevista <15% de DAC obstrutiva. O score apresentou um bom poder discriminativo (estatística-C 0,872; 95% IC 0,834–0,909: valor p<0,001) e de calibração (valor p=0,333, teste goodness of fit).
ConclusõesUm score clínico simples mostrou ser preditor do risco de DAC obstrutiva em doentes que se apresentam com IC-FER «de novo» e pode auxiliar o clínico a selecionar a modalidade diagnóstica mais apropriada para a avaliação de DAC obstrutiva.
In current clinical practice, obstructive coronary artery disease (CAD) remains the most common underlying cause of heart failure with reduced ejection fraction (HFrEF), with many of these patients having a history of myocardial infarction (MI) or revascularization.1 It is important to distinguish between CAD- and non-CAD-related HFrEF in the initial assessment of patients presenting with new-onset HFrEF of unknown etiology, since CAD-related HFrEF usually requires revascularization in order to improve symptoms and long-term prognosis.2,3 As such, it has been common practice to exclude CAD by invasive coronary angiography (ICA) independently of risk factors or medical history as a first-line approach. However, there are data showing that patients with left ventricular systolic dysfunction without chest pain or previous MI are unlikely to present extensive coronary disease that could explain left ventricular dysfunction or to have coronary anatomy suitable for bypass grafting.4
Although ICA remains the gold-standard technique for the assessment of obstructive CAD, it is known that outside the setting of an acute coronary syndrome (ACS), the prevalence of clinically meaningful CAD on ICA is low, even in patients with chest pain and previous positive noninvasive tests, as previously demonstrated by our group.5 Clinical guidelines have struggled to make clear recommendations regarding the management of patients presenting with new-onset HFrEF of unknown etiology.6 Some investigators advocate routine ICA in all subjects with left ventricular systolic dysfunction,4 while others suggest that ICA might be unnecessary in many patients and non-invasive imaging modalities, such as computed tomography coronary angiography, may be more appropriate as a gatekeeper to investigate or exclude obstructive CAD before ICA.7
Moreover, there is no reliable way to estimate the probability of obstructive CAD in patients with new-onset HFrEF of unknown etiology in the absence of previous ACS or known CAD.8 Accordingly, with the present study, we sought to derive a simple clinical score to estimate the risk of obstructive CAD in patients presenting with new-onset HFrEF of unknown etiology. As ICA is not a risk-free exam, this score may better assess the pre-test probability of CAD in HFrEF patients and thereby provide clinicians with a simple tool to determine the most appropriate strategy to assess the presence and severity of CAD.
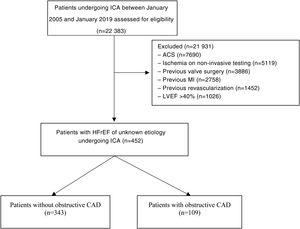
MethodsStudy populationThe study population consisted of all consecutive patients presenting with new-onset HFrEF of unknown etiology referred for ICA between January 2005 and 2019 and included in a local interventional cardiology database (Cardiobase™). Criteria for referral for ICA were at the discretion of the attending physician. The following exclusion criteria were applied: left ventricular ejection fraction (LVEF) >40%,1 severe valvular disease presumed to be the cause of HF, documented ischemia on non-invasive testing, previous known obstructive CAD (previous MI or coronary revascularization), previous cardiac surgery, and indication for ICA for other purposes. Patients with chest pain were included only if their primary diagnosis and clinical symptoms were predominantly of heart failure (HF).
Study designThis was a cross-sectional study performed at a single academic center. Demographic, clinical and angiographic data and vital status were prospectively collected in the ongoing ACROSS (Angiography and Coronary Revascularization On Santa cruz hoSpital) registry, which was approved by the local ethics committee, as previously published.9 All patients provided written informed consent and the study was approved by the ethics committee.
Obstructive CAD was defined as ≥70% luminal diameter stenosis by visual inspection in at least one coronary artery, or >50% in the left main.10
Two subgroups of patients were defined according to the angiographic findings: with obstructive CAD and without obstructive CAD. Logistic regression was used to identify independent clinical predictors of obstructive CAD. The beta regression coefficients of the selected variables were then used to develop a clinical model that estimates the probability of obstructive CAD for a given patient.
Data measures and statistical analysisNormally and non-normally distributed variables were expressed as mean±standard deviation and median and interquartile range, respectively.
The following variables were assessed for their association with obstructive CAD: age, gender, hypertension, diabetes, hypercholesterolemia, cigarette smoking, family history of CAD, chronic kidney disease, peripheral arterial disease (PAD), LVEF, anginal chest pain, and the presence of regional wall motion abnormalities on two-dimensional echocardiography. Univariate analysis was performed using univariate logistic regression.
In order to derive a predictive model for the presence of obstructive CAD, variables with p<0.05 in the univariate analysis were entered simultaneously in a multivariate logistic regression model performed with bootstrap sampling with replacement using 1000 samples. Bootstrapping was used for internal validation of the model and the 95% confidence intervals (CI) of the odds ratios were estimated using bias corrected accelerated bootstrapping.
To create a practical risk score, each of the independent predictors was assigned a number of weighted points proportional to its beta regression coefficient value, rounded to the nearest integer, yielding the multiplying coefficient for each variable in the score. The resulting score, defined as the sum of the points assigned to each weighted variable, was calculated for every patient. The population was then categorized according to the score into low- (predicted probability <15%), medium- (predicted probability 15–75%) and high-risk strata (predicted probability >75%) for the presence of obstructive CAD.
The performance of the prediction risk score was assessed using model discrimination and calibration. Model discrimination (i.e. the extent to which the model can differentiate between those who have and those who do not have obstructive CAD) was summarized using the area under the curve (AUC) on receiver operating characteristic analysis. The AUC can range from 0.5 to 1.0, with higher values indicating improved ability to predict or identify the endpoint of interest (in this case, the presence of obstructive CAD). Model calibration (reflecting how close predicted obstructive CAD prevalence rates are to the actual observed rates) was assessed using the Hosmer–Lemeshow goodness-of-fit test. A statistically significant p-value from this test would reject the null hypothesis that the features in the model fit the data well.
The statistical analysis was performed using IBM SPSS version 25.0 (IBM SPSS Inc., Chicago, IL, USA) for Mac OS. Statistical significance was set at p<0.05 (two-sided).
ResultsOf the 23838 consecutive patients who underwent elective ICA for all indications during the study period, 452 met the stated eligibility criteria and thus composed the final population of patients with new-onset HFrEF of unknown etiology. The study flowchart is summarized in Figure 1. The baseline characteristics of the study population are presented in Table 1 and a comparison of important clinical features between patients with and without obstructive CAD is shown in Table 2. Patients with obstructive CAD were older, had a higher prevalence of diabetes, and were more likely to have conventional cardiovascular risk factors and atherosclerosis in other vascular territories, as demonstrated by the higher prevalence of PAD. Mean LVEF and a family history of CAD did not differ between patients with and without obstructive CAD.
Baseline characteristics of the overall study population (n=452).
| Age, years | 64±12 |
| Male, n (%) | 361 (80) |
| Hypertension, n (%) | 289 (64) |
| Diabetes, n (%) | 122 (27) |
| Dyslipidemia, n (%) | 168 (37) |
| Family history of premature CAD, n (%) | 17 (4) |
| Smoking, n (%) | 172 (38) |
| LVEF | |
| 31–40%, n (%) | 209 (46) |
| <30%, n (%) | 244 (54) |
| Cerebrovascular disease, n (%) | 29 (6) |
| PAD, n (%) | 21 (5) |
| Anginal chest pain, n (%) | 89 (20) |
| Regional wall motion abnormalities, n (%) | 70 (16) |
| Coronary angiographic findings | |
| Normal angiography, n (%) | 275 (60.8) |
| Non-obstructive CAD, n (%) | 68 (15.0) |
| Obstructive CAD, n (%) | 109 (24.1) |
| No. of coronary arteries with >70% stenosis | |
| 1, n (%) | 63 (13.9) |
| 2, n (%) | 13 (2.9) |
| 2 (including proximal LAD), n (%) | 9 (2.0) |
| 3, n (%) | 19 (4.2) |
| Left main >50% stenosis, n (%) | 14 (3.1) |
CAD: coronary artery disease; LAD: left descending anterior artery; LVEF: left ventricular ejection fraction; PAD: peripheral arterial disease.
Univariate analysis for obstructive coronary artery disease.
| Without obstructive CAD (n=343) | Obstructive CAD (n=109) | OR (95% CI) | p | |
|---|---|---|---|---|
| Age, years | 63±12 | 69±11 | 1.04 (1.02–1.06) | <0.001 |
| Male, n (%) | 258 (75) | 103 (95) | 5.66 (2.40–13.4) | <0.001 |
| Hypertension, n (%) | 208 (61) | 84 (77) | 2.18 (1.33–3.58) | <0.001 |
| Diabetes, n (%) | 74 (22) | 48 (44) | 2.86 (1.81–4.52) | <0.001 |
| Dyslipidemia, n (%) | 110 (32) | 65 (60) | 3.13 (2.01–4.88) | <0.001 |
| Family history of premature CAD, n (%) | 13 (4) | 4 (4) | 0.97 (0.31–3.03) | 0.954 |
| Smoking, n (%) | 117 (34) | 55 (51) | 1.97 (1.27–3.05) | 0.002 |
| LVEF | ||||
| 31–40%, n (%) | 153 (45) | 55 (51) | 1.27 (0.82–1.95) | 0.286 |
| <30%, n (%) | 190 (55) | 54 (50) | 0.79 (0.51–12.2) | 0.286 |
| Cerebrovascular disease, n (%) | 18 (5) | 11 (10) | 2.03 (0.93–4.44) | 0.077 |
| Chronic kidney disease, n (%) | 22 (6) | 13 (12) | 1.98 (0.96–4.07) | 0.065 |
| PAD, n (%) | 8 (2) | 13 (12) | 5.67 (2.28–14.08) | <0.001 |
| Anginal chest pain, n (%) | 61 (19) | 28 (26) | 1.60 (0.96–2.66) | 0.072 |
| Regional wall motion abnormalities, n (%) | 17 (5) | 53 (49) | 18.15 (9.81–33.59) | <0.001 |
CAD: coronary artery disease; CI: confidence interval; OR: odds ratio; PAD: peripheral arterial disease.
The results of univariate and multivariate logistic regression analysis are presented in Tables 2 and 3, respectively. Eight variables associated with the presence of obstructive CAD were identified in univariate analysis and entered into a multivariate model, which was simplified by removing age and hypertension, as these were not significantly associated with obstructive CAD. The AUC of the simplified model was 0.872 (95% CI 0.834–0.909). This model is summarized in Table 3. The p-value from the goodness-of-fit test was 0.333, indicating that the simplified model fit the data well.
Simplified multivariate model for prediction of obstructive coronary artery disease.
| Feature | Adjusted OR (95% CI) | p | Parameter estimate |
|---|---|---|---|
| Intercept | −5.011 | ||
| Male, n (%) | 5.34 (1.87–15.2) | 0.002 | +1.674 |
| Diabetes, n (%) | 3.56 (1.92–6.60) | <0.001 | +1.268 |
| Dyslipidemia, n (%) | 3.20 (1.76–5.80) | <0.001 | +1.161 |
| Smoking, n (%) | 2.44 (1.32–4.50) | 0.005 | +0.890 |
| PAD, n (%) | 3.74 (1.27–11.05) | 0.017 | +1.319 |
| Regional wall motion abnormalities, n (%) | 22.51 (10.86–46.66) | <0.001 | +3.114 |
CAD: coronary artery disease; CI: confidence interval; OR: odds ratio; PAD: peripheral arterial disease.
The parameter estimates from the simplified model were used to develop a risk score to predict obstructive CAD. Each of the variables included in the simplified model was assigned a number of points proportional to its beta coefficient, i.e. the natural logarithm of the odds ratio point estimate for each variable in the model. The resulting scores assigned to each feature are presented in Table 4.
Risk score for prediction of obstructive coronary artery disease.
| Feature | Points |
|---|---|
| Male gender | +2 |
| Diabetes | +1 |
| Dyslipidemia | +1 |
| Smoking | +1 |
| PAD | +1 |
| Segmental wall motion abnormality | +3 |
| Score | Predicted probability of obstructive CAD |
|---|---|
| 0 | 0.024 |
| 1 | 0.033 |
| 2 | 0.012 |
| 3 | 0.130 |
| 4 | 0.345 |
| 5 | 0.552 |
| 6 | 0.750 |
| 7 | 0.889 |
| 8 | 1.000 |
| 9 | 1.000 |
CAD: coronary artery disease; PAD: peripheral arterial disease.
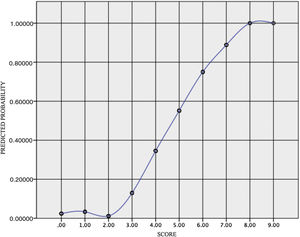
Individual calculated scores ranged from 0 to 9. The internally validated AUC for the score was 0.872 (95% CI 0.834–0.909), as depicted in Figure 2. Probabilities of obstructive CAD predicted by the score are summarized in Table 4 and ranged from 0.12 to 1.00.
Three risk categories for the presence of obstructive CAD were defined according to the probability of CAD predicted by the score: low (score ≤3 points; predicted probability 1.21–13.0%), intermediate (4–5 points; predicted probability 34.5–55.4%) and high risk (≥6 points; predicted probability: 75.0–100.0%). The distribution of patients in our population by risk category according to the presence or absence of obstructive CAD, and the probability of obstructive CAD predicted by the risk score, are illustrated in Figures 3 and 4, respectively. These three risk categories (high, intermediate and low) represent 63.3%, 25.0% and 11.7% of the total population, respectively, and may help the clinician in decision-making for the selection of the most appropriate diagnostic test according to the predicted probability.
Our work shows that 75.9% of patients referred for ICA in the setting of new-onset HFrEF without previously known CAD do not present obstructive coronary lesions. In this subset of patients, obstructive CAD predictors were male gender, diabetes, dyslipidemia, smoking, PAD and regional wall motion abnormalities on echocardiogram, with the low risk category (score 0–3) presenting a prevalence of obstructive CAD of only 5.6%. The reported prevalence of obstructive CAD in patients with HFrEF is heterogeneous, with data from randomized clinical trials suggesting obstructive CAD as the underlying cause of HFrEF in nearly 65% of patients, while observational data from studies including HFrEF patients without previous MI or angina suggest a much lower prevalence.11
In this study we developed a score that estimates the risk of obstructive CAD in patients presenting with new-onset HFrEF of unknown etiology. Two important aspects of the risk prediction model were assessed: discrimination (the ability to identify those who have obstructive CAD) and calibration (reflecting how close predicted obstructive CAD rates are to the actual observed rates). Our simplified model showed good discriminative power, as demonstrated by a C-statistic of 0.872. Model calibration was similarly good, with the goodness-of-fit test giving p=0.333, supporting the accuracy of the score.
Our analysis yielded six independent predictors of obstructive CAD: male gender, dyslipidemia, smoking, diabetes, PAD and the presence of segmental wall motion abnormalities on two-dimensional echocardiography. The presence of segmental wall motion abnormalities showed the strongest association with the presence of obstructive CAD, outweighing all other factors. There are data suggesting that the finding of a segmental wall motion abnormality has a high specificity (86%) for the presence of significant CAD and is a reasonable predictor for multivessel disease and for the presence of at least one diseased vessel with >70% stenosis.12 Although the interpretation of echocardiographic findings is subject to several well-known limitations, our findings suggest that not including this readily accessible finding would significantly compromise the score's accuracy.
PAD also emerged as an independent predictor of obstructive CAD. Atherosclerosis is a generalized vascular disease and PAD constitutes a sensitive marker of other forms of atherosclerosis such as obstructive CAD13,14 and can be regarded as a marker of a more diffuse and severe disease process.
Gender was also independently associated with the presence of obstructive CAD in our population, together with dyslipidemia and smoking. These are well-established risk factors for the development of obstructive CAD.15 In line with these findings, type 2 diabetes was also an independent predictor of obstructive CAD, given its association with clustered risk factors for cardiovascular disease.15
Although angina was more common in patients with obstructive CAD, it was also frequently observed in the absence of obstructive CAD, and was therefore not a significant predictor. Furthermore, this finding illustrates that patients with congestive HF may experience anginal-type chest pain in the absence of significant CAD, perhaps because of subendocardial ischemia associated with high left ventricular end-diastolic pressure.16
To the best of our knowledge, two other scores have been developed to predict the presence of CAD in patients with HFrEF of unknown etiology. The clinical prediction rule proposed by Doukky et al. included diabetes, electrocardiographic Q waves or left bundle branch block and ≥2 non-diabetes risk factors (age, dyslipidemia, hypertension and tobacco use) as predictors of obstructive CAD.17 The recently published CT-HF score8 was developed to identify HF patients with a low risk of obstructive CAD and included male gender, angina, smoking, hyperlipidemia, diabetes, extracardiac arteriopathy and age as predictors of obstructive CAD. The results of our study generally reinforce the findings reported in these studies and contribute further by adding resting segmental wall motion abnormalities as a predictor of obstructive CAD.
We believe that our score can prevent patients with new-onset HFrEF of unknown etiology from undergoing unnecessary invasive testing while helping clinicians to predict the individual probability of obstructive CAD in everyday clinical practice. However, even though our score was designed to estimate the presence of obstructive CAD and aid decision-making, it is no substitute for sound clinical judgment. There is currently no consensus on what constitutes an expected prevalence of CAD high enough that justifies referring patients with HFrEF of unknown etiology directly for ICA; this will probably depend on clinical setting, procedural risk and patient preference, among other factors. Consequently, thresholds of our risk score for selecting patients who should be referred directly for ICA were largely arbitrary and based on clinical expertise.
LimitationsThe present investigation has limitations that should be acknowledged. First, this was a retrospective analysis with the limitations and biases inherent to its design. Also, it relies on the quality of registry data, another limitation that is universally inherent to this type of study design. However, we provide an analysis that is based on common and easily reported variables and is thus potentially less prone to uncertainty. Furthermore, it was a single-center study, although from a large academic referral center, reflecting the diagnostic approach of multiple secondary centers. The indication for ICA was left at the referring physician's discretion and the echocardiographic findings were not reviewed by a core lab.
The exclusion of patients with acute symptoms and a history of MI, percutaneous coronary intervention or coronary artery bypass grafting may have increased the prevalence of non-CAD HFrEF. However, this might be regarded as a strength of our study, as it addresses the clinical question of the best strategy to exclude CAD as a cause of HFrEF in patients without an apparent etiology.
Demonstration of obstructive CAD as assessed by ICA does not necessarily imply causation, as it may be a concomitant bystander rather than the main etiology of HFrEF. The fact that the majority of patients with obstructive CAD in our population had single-vessel disease is further evidence that the prevalence of severe coronary disease in patients presenting with new-onset HFrEF without a previous history of ACS, angina or ischemia in non-invasive assessment is low, and that obstructive CAD as the main etiology for HFrEF is generally secondary to sequelae from acute coronary events, since HFrEF is a relatively uncommon form of presentation of obstructive CAD. This being so, the presence of obstructive CAD in HFrEF patients may not have a direct impact on prognosis. In addition, even though our score might be less specific for severe obstructive CAD (which has a higher probability of a causal relationship with left ventricular systolic dysfunction in the individual patient), it showed a high sensitivity for this subgroup, demonstrating the clinical safety of its use. This should be taken into account and highlights the importance of the appropriate selection of patients who should undergo ICA.
Although previously reported by Doukky et al.17 as a predictor of obstructive CAD in patients with HFrEF, electrocardiographic data were not included in the present investigation due to a high percentage of missing data, precluding proper statistical analysis.
Importantly, our model was not validated in a separate dataset, which precludes conclusions about its external validity. As such, further studies are needed to validate this score in other HFrEF cohorts and to confirm its value as a generalizable clinical prediction tool.
ConclusionsIn conclusion, an easy-to-use score with a limited number of variables showed the ability to predict the risk of obstructive CAD in a large cohort of patients presenting with new-onset HFrEF of unknown etiology undergoing ICA. This model may guide clinicians in the selection of the most appropriate diagnostic modality for patients presenting with new-onset HFrEF without an established etiology.
FundingNone to declare.
Conflicts of interestThe authors have no conflicts of interest to declare.