We present the case of a 53-year-old man, a former smoker with squamous cell lung carcinoma under palliative chemotherapy as relevant prior history.
The patient was admitted to the emergency department with sudden worsening of rest dyspnea and pleuritic chest pain. He was hemodynamically stable and had decreased breath sounds in the left lung. The electrocardiogram showed a widespread concave ST-elevation and PR-depression and reciprocal ST-depression and PR-elevation in lead aVR.
The transthoracic echocardiogram revealed normal biventricular function, no kinetic segmental changes, “swirling bubbles sign” in the pericardial sac and “air gap sign” (video 1), manifesting in the disappearance of the cardiac silhouette in systole.
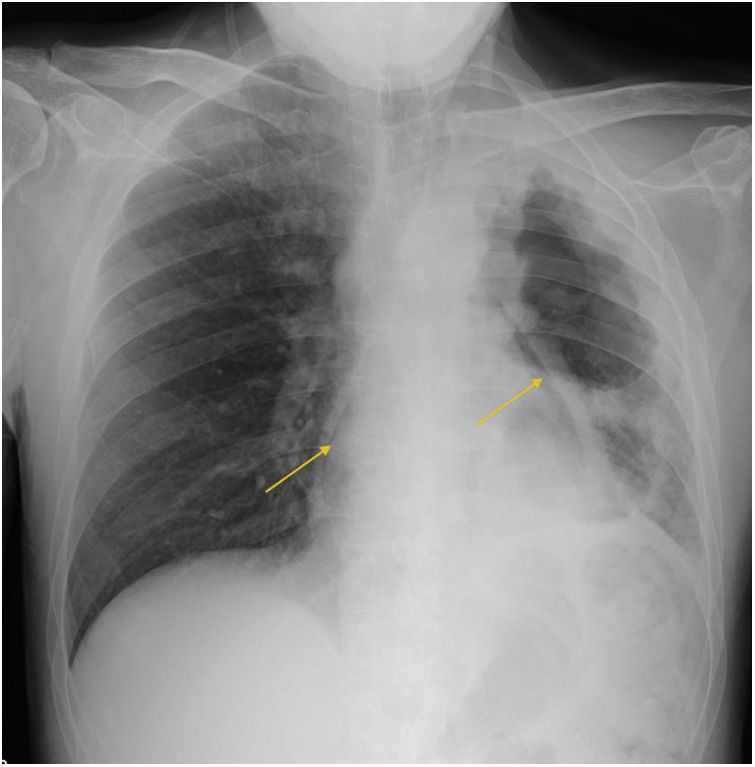
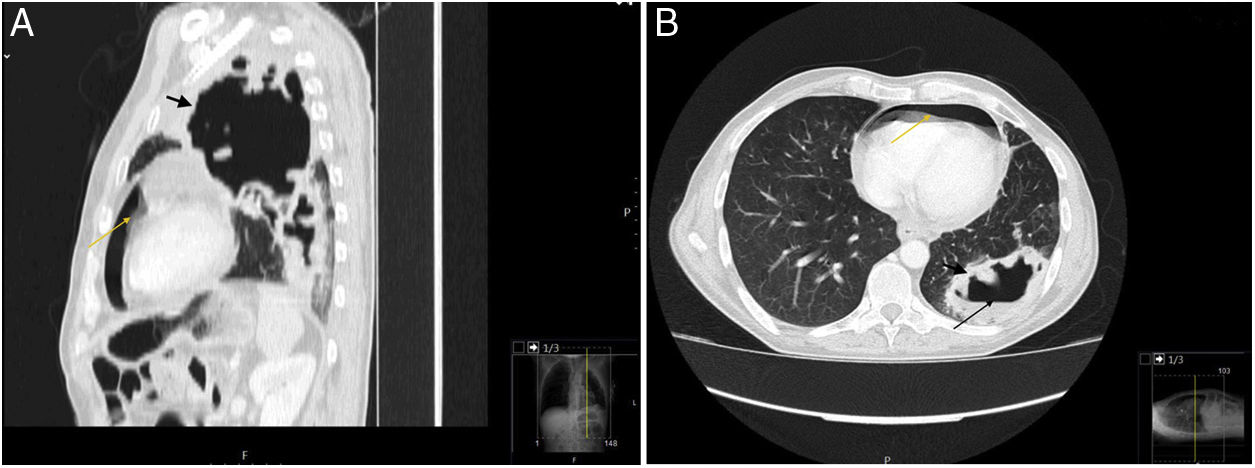
The chest radiography showed signs of pneumopericardium (Figure 1, long yellow arrows) and left cavitary lung mass. For better characterization, the patient underwent a computed tomography lung scan which revealed the extension (from the apex to the diaphragmatic surface) of the thick-walled gas-filled mass (Figure 2A/B, short black arrow) with an air-fluid level (Figure 2B, long black arrow) and distension of pericardial cavity with air-fluid level (Figure 2A/B, long yellow arrow) due to a direct pleuro-pericardial communication.
Due to hemodynamical stability, with no clinical or echocardiographic signs of tension pneumopericardium, the patient was monitored and managed conservatively under watchful observation. Unfortunately, the patient's condition deteriorated progressively, and he died 18 days later.
Conflicts of interestThe authors have no conflicts of interest to declare.