Currently, the treatment for most valve diseases requiring intervention is surgical; and there are unmet clinical needs in patients who are inoperable due to high surgical risk. This is the case of up to 49% of patients requiring mitral valve intervention.1,2
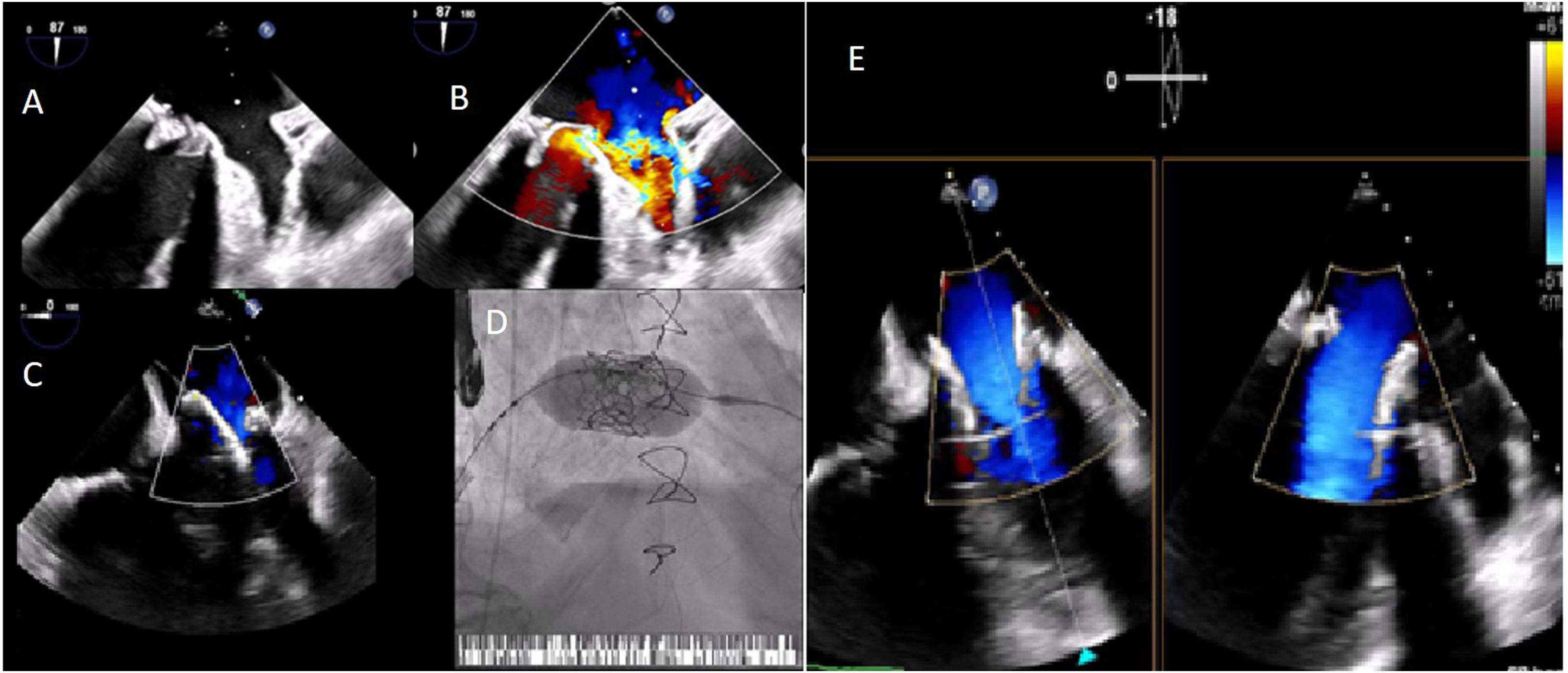
We describe the case of an 85-year-old man who underwent mitral replacement surgery with a biological prothesis (Carpentier-Edwards SAV 29) in 2011. In October 2020, he developed signs of heart failure. An echocardiogram was performed, revealing severe mitral bioprosthetic regurgitation, due to cusp prolapse (Video 1); preserved biventricular systolic function and major pulmonary hypertension. Due to his advanced age, frailty and having undergone previous cardiac surgery, the risk of new surgery was deemed too high. The decision was taken to perform a percutaneous mitral valve-in-valve implantation of a Sapiens 3 Ultra-29. The valve was inserted via transseptal puncture, with transesophageal echocardiogram and fluoroscopy guidance (Video 1). During valve deployment, rapid ventricular pacing was applied. After valve implantation, a small peri-prothesis leak was observed. There was no interference with the adjacent cardiac structures (Video 2); the mean transvalvular gradient was 5mmHg. The patient improved and was discharged five days later.
Biological valves are being used increasingly,3,4 however, their longevity is shorter and the consequently the number of patients with degeneration of bioprosethic valves will increase. The balloon-expandable Sapiens 3 valve is designed to be deployed in a rigid structure, so that the radial force of the balloon expanding valve provides support.2 This procedure should be considered in high surgical risk patients (Figure 1).
(A and B) Severe mitral prothesis regurgitation due to cusp prolapse, jets directed posterior-laterally and to the left atrial appendage; implantation of an Edwards Sapiens 3 Ultra-29 valve, with transesophageal echocardiography (C) and fluoroscopy (D) guidance; (E) final result: no signs of interference in the adjacent cardiac structures; a small lateral peri-prothesis leak was observed.
The authors have no conflicts of interest to declare.