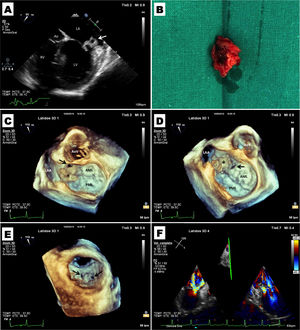
An 18-year-old male presented to the emergency department with persistent fever (up to 39°C) and progressive fatigue. On admission, physical examination revealed heart rate of 92 bpm, temperature of 37.4°C and a grade 4/6 pansystolic murmur at the apex radiating to the left axillary area. Complete blood count was normal, but C-reactive protein was elevated at 207 mg/l (normal 0-5 mg/l). Transthoracic echocardiography (TTE) showed an echodense mass located at the mitral annulus associated with severe mitral regurgitation. Three of four blood cultures were positive for Haemophilus parainfluenzae. Transesophageal echocardiography (TEE) showed an annular abscess at the anterolateral commissure measuring 16 mm×18 mm (Figure 1A and Video S1), complicated by two fistulas: one directed toward the lateral wall of the left atrium with three-dimensional (3D) effective regurgitant orifice (ORE) of 0.28 cm2 (Figure 1C and E, Video S2) and another located more medially as a possible perforation of the anterior leaflet at the A1 level, with 3D ORE of 0.38 cm2 (Figure 1D and E, Video S3), which together were causing severe mitral regurgitation (Figure 1F). These echocardiographic findings were confirmed at surgery, in which resection of the anterolateral commissure (Figure 1B) and commissurotomy were performed without intraoperarative complications and with an excellent postoperative course. Control TTE showed minimal early systolic central regurgitation, and no residual fistula was observed (Videos S4-S6).
(A) Transesophageal echocardiography (TEE) of the mitral valve at 55°. Note the abscess at the anterolateral commissure of the mitral valve (arrow); (B) surgical specimen consisting of the mitral valve abscess; (C) TEE at 110° with three-dimensional (3D) reconstruction of the mitral valve (‘surgical’ view), showing perforation of the anterior leaflet at the A1 level and the abscess (asterisk); (D) TEE at 110° with 3D reconstruction of the mitral valve (‘surgical’ view), showing the other fistula directed toward the lateral wall of the left atrium and the abscess (asterisk); (E) TEE at 110° with 3D reconstruction of the mitral valve view from the ventricular side. Note the two fistulas in the same view; (F) TEE at 125° of the mitral valve with color Doppler showing the mitral regurgitation jets of both fistulas.
This case highlights the usefulness of 3D-TEE for accurate assessment of the mitral valve apparatus, as it enables cardiac surgeons to perform a comprehensive preoperative anatomical and functional assessment of this condition.
Conflicts of interestThe authors have no conflicts of interest to declare.
The following are the supplementary material to this article: