Cardiac rehabilitation (CR) is a multidisciplinary process for patients recovering after an acute cardiac event or with chronic cardiovascular disease that reduces mortality and morbidity and improves quality of life. It is considered a cost-effective intervention and is expressly indicated in the guidelines of the major medical societies.
In Portugal, only 8% of patients discharged from hospital after myocardial infarction are included in CR programs. In Europe overall, the percentage admitted to CR programs is 30%, while in the USA it is 20-30%.
In view of the underuse of CR in Portugal, we call the attention of the health authorities to the need to increase the number and national coverage of CR programs, while maintaining high quality standards. The aim is for all patients resident in Portugal who are eligible for CR programs to have the same opportunities for access and attendance.
In order to preserve the benefits and safety of this intervention, CR needs to be performed according to international guidelines. The fact that various initiatives in this field have been developed by different professional groups, some of them non-medical, that do not follow the European guidelines, has prompted us to prepare a series of norms defining mandatory criteria for CR, based on current knowledge and evidence. In this way we aim to ensure that the required increase in the number of CR programs, linked in a national network of CR centers, does not detract from the need to maintain their efficacy and quality. These criteria should serve as the basis for the future accreditation of CR centers in Portugal.
A reabilitação cardíaca é um processo multidisciplinar de recuperação do doente após evento cardiovascular agudo ou com doença cardíaca crónica, que conduz à redução da mortalidade e morbilidade e melhoria da qualidade de vida. Considera-se uma intervenção custo-eficaz com indicação formal expressa em recomendações das mais importantes sociedades científicas internacionais.
Em Portugal, apenas 8% dos doentes com alta hospitalar após enfarte são incluídos em programas de reabilitação cardíaca. Na Europa, a percentagem de admissão nesses programas é em média de 30%, enquanto nos Estados Unidos da América esse percentual se situa entre 20-30%.
Pela subutilização franca da reabilitação cardíaca em Portugal, chamamos a atenção das autoridades de saúde para a necessidade de aumentar o número e a distribuição dos programas de reabilitação cardíaca no território nacional e manter padrões de elevada qualidade. Pretende-se que todos os doentes residentes em Portugal elegíveis para programa de reabilitação cardíaca possam ter idênticas condições de acesso e atendimento relativamente aos programas.
Para que os benefícios e a segurança dessa intervenção sejam salvaguardados, implica que o programa de reabilitação cardíaca seja aplicado como é preconizado nas diretrizes internacionais. A existência de várias iniciativas por parte de diferentes grupos profissionais, inclusive não médicos, com pretensão de intervir nesse campo, sem respeito pelas recomendações formais europeias, levou à elaboração de um conjunto de normas que definem os critérios mandatórios para a reabilitação cardíaca, com base no conhecimento e na evidência científica atual. Pretendemos dessa forma garantir que o necessário aumento do número de programas de reabilitação cardíaca não seja dissociado da necessária eficiência e qualidade dos mesmos, articulados numa rede nacional de centros de reabilitação cardíaca. Esses critérios deverão servir de base à futura e necessária acreditação dos Centros de Reabilitação Cardíaca em Portugal.
The present paper is the product of study and reflection by members of the Portuguese Society of Cardiology (SPC), in particular the SPC's Working Group on Exercise Physiology and Cardiac Rehabilitation, most of whom are cardiologists, with the purpose of alerting the health authorities to the deficiencies in cardiovascular prevention and rehabilitation in Portugal and the need to increase the number and national coverage of cardiac rehabilitation (CR) programs, while assuring criteria of quality and efficacy, described below.
Only through rational and balanced distribution of a greater number of cardiac rehabilitation centers, with programs fulfilling the criteria defined in these recommendations, will it be possible to ensure equality of access for all cardiovascular patients to a cost-effective intervention that is safe and indicated as essential due to all its proven benefits.
These criteria for CR, based on the current guidelines of the European Society of Cardiology (ESC)/European Association of Preventive Cardiology (EAPC),1 the American Heart Association/American Association of Cardiovascular and Pulmonary Rehabilitation (AHA/AACPR),2 the American College of Cardiology/American Heart Association,3 the American College of Cardiology Foundation/American Heart Association,4 and the British Association for Cardiovascular Prevention and Rehabilitation,5 should be mandatory and serve as a basis for the future accreditation of CR centers in Portugal, to be developed in the short term.
RationaleDefinition of cardiac rehabilitationCR is defined as an intervention intended to help the patient recover or improve their physical, psychological, social and vocational functioning after an acute cardiac event or in the context of chronic cardiovascular disease (such as angina or heart failure). It consists of an integrated multidisciplinary process with various components, emphasizing physical exercise, changes in behaviors aimed at healthier lifestyles, control of risk factors and intervention in psychological factors, with the main purpose of delaying the progression of the underlying cardiovascular disease.2,3
The benefits of CR have been thoroughly demonstrated, including reductions in mortality and morbidity following myocardial infarction, and improvements in quality of life and functional capacity in cardiovascular disease, including heart failure.6–10
The ESC/EAPC1 and the AHA/AACPR2 classify CR as a therapeutic intervention with class I indication (mandatory), based on the highest levels of scientific evidence (A or B, according to the indications) in multiple cardiac conditions. Those eligible for this procedure are mainly coronary patients (with or without percutaneous intervention),3 those with heart failure (with or without devices)6,7 and those undergoing cardiac surgery (including revascularization, valve surgery and cardiac transplantation).4,6,7
Cardiac rehabilitation in Portugal, Europe and the worldCardiovascular disease remains the leading cause of death in Europe, and rapid, effective intervention is necessary. Although there have been significant improvements in pharmacological therapy, percutaneous coronary intervention and cardiac surgery, it is now urgent to invest in the areas of prevention and rehabilitation, complementing the other interventions.
Portugal has one of the lowest rates of inclusion in CR programs in Europe, due to cultural, scientific, organizational and financial factors.11–13 Only 8% of patients suffering myocardial infarction participate in these programs,12 in contrast to the European average of over 30% (in many countries it exceeds 50%).13
The last survey performed by the SPC, in 2013-2014,12 identified 23 centers in Portugal with CR programs, 12 public and 11 private, which represents an increase compared to 2007, when there were 16 centers.11 The percentage of patients discharged from hospital after myocardial infarction who participated in a CR program has almost tripled in recent years, increasing from 3% in 200711 to 8% in 2014,8 even though this figure is clearly insufficient to meet the country's needs.11,12,14
Portuguese cardiac patients with indication for a CR program, especially north of the Douro river (except for the Greater Porto area), in the Central region, and south of the Tejo river, are largely excluded from a therapeutic intervention known to be cost-effective, that reduces mortality and hospitalization, improves quality of life and accelerates the normalization of daily life, especially return to work.6,8,9,15–17 These benefits have positive effects on the psychosocial well-being of cardiovascular patients and on the economic status of individual patients, their families, and society as a whole.
The 2010 European survey on cardiac rehabilitation, the European Cardiac Rehabilitation Inventory,13 which covered 28 countries, showed considerable differences in the picture of cardiac rehabilitation, and placed Portugal among the 15 countries with CR use below 15%. These countries differ from the others in not having national associations, recommendations, legislation or funding for CR. Currently, according to data on the EAPC's Country of the Month project, available on the EAPC's website, the situation in Europe regarding CR remains heterogeneous, with different obstacles, participation rates and programs.18
In the US, the participation rate in CR programs is only 20-30%. It has been estimated that increasing this rate to 70% would save 25000 lives and prevent 18000 hospitalizations per year.19
Worldwide, only 38.8% of countries have CR programs: 68% of high-income countries, 28.2% of median-income countries and 8.3% of low-income countries. The availability of CR is much lower than that of other evidence-based interventions, such as revascularization and pharmacological therapy. In high-income countries, the density of CR programs ranges from 1:100000 to 300000 population, which if applied to Portugal, and using the lower figure, would require the existence of 100 programs for a population of 10 million.20 In fact, there are fewer than one fifth of the CR programs required in Portugal, and many of these have fewer than 50 admissions per year.
Role of the Portuguese Society of Cardiology in cardiac rehabilitation in Portugal: implementation, accreditation and certificationThe SPC has performed several national surveys of active CR centers since 1998,21 and has found centers to be concentrated in the areas of Greater Porto and Greater Lisbon, with only one center in the south (Faro) and none in Trás-os-Montes, the central and interior regions of the country, Ribatejo or the Alentejo. In view of this situation, implementation of a CR program in each cardiology or cardiothoracic department has been recommended, in order to widen national coverage.
In recent decades, the SPC has been the leading voice in promoting awareness and discussion of the issue of CR availability among cardiologists, physical medicine and other specialist physicians, other health professionals including psychologists, physiotherapists, exercise physiologists, nurses and nutritionists, and others. Recently, increased interest in CR has been noted from several groups of health professionals, who have expressed the intention to assume responsibility for coordinating CR programs, with no medical background or specific education or training in the area of CR.
Due to the need to develop and implement CR while following the international guidelines and ensuring that programs are performed by skilled multidisciplinary teams, the SPC, in conjunction with specialists from the Working Group on Exercise Physiology and Cardiac Rehabilitation, decided to prepare this document, which defines mandatory criteria for CR, in order to ensure the safety, efficacy and quality of CR programs.
The present recommendations constitute a solid basis for national accreditation of CR programs. The SPC considers desirable the creation of a specific competence in CR, to be recognized by the Ordem dos Médicos (the Portuguese Order of Physicians).
Basis for launching a cardiac rehabilitation programIt is important to be aware that it is not sufficient simply to create a program and call it ‘cardiac rehabilitation’ in order to intervene beneficially and safely in cardiovascular patients.
The establishment of a CR program should take into consideration the following questions:
Is there a need for a CR program?
According to the above considerations, there is no doubt concerning the need to establish quality CR centers and programs, with a more balanced national distribution.
What are the target populations?
Current developments in cardiology, particularly in terms of percutaneous and surgical interventions, as well as increasing awareness of the benefits of CR, are leading to a significant widening of CR indications22:
- •
Acute coronary syndromes
- •
Chronic heart failure (with or without resynchronization/defibrillator or left ventricular assist device)
- •
Post cardiac surgery (valvular, coronary, congenital and cardiac transplantation)
- •
Post percutaneous intervention (coronary, aortic valve implant, mitral clip, and others).
What is the location of implementation?
In view of the present state of cardiac rehabilitation in Portugal, we argue that phase I should be performed in the hospital where admission took place, and phase II in the same location or alternatively where periodic outpatient follow-up of cardiac patient is performed.
Patients who were discharged from the hospital after the acute event without CR, or who have difficulty in attending the hospital where the admission took place, should be referred in phase II to the most convenient and easily accessible CR center, at a maximum of 30 km from their place of residence or work, or alternatively to a home-based program linked to the admission hospital.
When phase II is concluded, long-term CR should be provided, which usually runs in centers external to the hospitals accredited for this purpose.
Do physicians consider rehabilitation?
Physicians’ awareness is an important aspect of cardiac rehabilitation. The large cardiovascular centers in Portugal recently had to demonstrate that they had CR programs in order to be considered referral centers in several areas, which demonstrates the importance of these programs. However, not all physicians place an appropriate value on CR.
Every cardiologist and cardiac surgeon has the responsibility to refer all eligible patients to a CR program, as part of a therapeutic plan of excellence. The involvement of the referring physician, hospital or outpatient cardiologist, cardiac surgeon, or generalist is crucial for the enrollment and continuation of the patient in the program.
Is it feasible?
The performance of CR programs depends on adequate funding and access of patients with formal indication.
Funding should be provided by the National Health Service, Social Security, health insurance, other entities or patients’ private payment, according to the organization of the local health system, and may vary over the course of the different phases of the program.
Access of all patients with formal indication for CR should be guaranteed for phases I and II in CR centers that fulfill the mandatory criteria set out in this document.
Structure of a cardiac rehabilitation programCentral componentsEach CR center should have previously defined its exercise and education program for each of the diagnostic groups of patients being treated, the following components being considered mandatory.2,5,22-24
Medical assessment- •
Clinical history of cardiovascular disease, risk factors, comorbidities; general physical exam, identification of locomotor and cognitive limitations.
- •
Assessment of functional capacity, including exercise testing in phases II and III in all patients except in cases of patient incapacity.
- •
Assessment and stratification of cardiovascular risk for exercise and determination of the level of supervision required.
- •
Initial blood and cardiac function tests (Table 1).
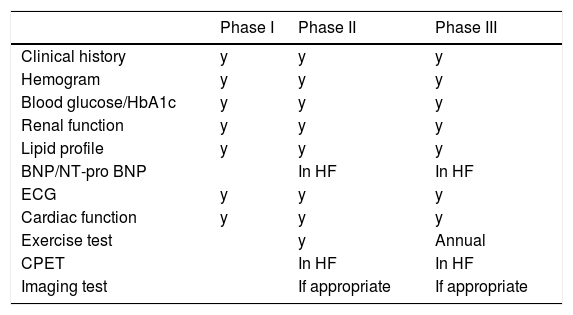
Table 1.Patient assessment at admission to the different program phases.
Phase I Phase II Phase III Clinical history y y y Hemogram y y y Blood glucose/HbA1c y y y Renal function y y y Lipid profile y y y BNP/NT-pro BNP In HF In HF ECG y y y Cardiac function y y y Exercise test y Annual CPET In HF In HF Imaging test If appropriate If appropriate BNP: brain natriuretic peptide; cardiac function: usually assessed by echocardiography; CPET: cardiopulmonary exercise test; HF: heart failure; NT-pro BNP: N-terminal pro-brain natriuretic peptide; y: yes.
- •
Individualized medical exercise prescription by a cardiologist or physical medicine specialist, specifying a structured exercise training program to ensure efficacy and safety.
- •
Supervision of exercise training will be performed, according to cases and phases (Table 2), by a physiotherapist, exercise physiologist or rehabilitation nurse in person, under coordination by a physician (Table 2).
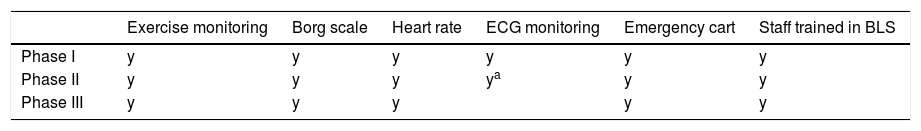
Table 2.Exercise monitoring during program phases.
Exercise monitoring Borg scale Heart rate ECG monitoring Emergency cart Staff trained in BLS Phase I y y y y y y Phase II y y y ya y y Phase III y y y y y - •
Medical advice on extra-program physical activity, including leisure, vocational and sexual activity, driving and traveling.
- •
Cardiology consultation
- •
Specific consultations as necessary for all risk factors: diabetes, smoking cessation, hypertension, dyslipidemia, obesity, and others.
- •
Nutritional consultation for all patients in general and specifically for diabetic, obese, frail, hypertensive and dyslipidemic patients.
- •
Psychological assessment of all patients, ideally through psychology and/or psychiatry consultations, according to the clinical indication
- •
Psychological intervention by a psychologist or psychiatrist, particularly through cognitive-behavioral techniques for lifestyle modification, control of cardiovascular risk factors and adherence to pharmacological and non-pharmacological therapy, and relaxation techniques when indicated.
Counseling for lifestyle modification by physicians, nurses, nutritionists, psychologists and other members of the CR team, including:
- •
Increased physical activity and appropriate diet
- •
Return to work, participation in sports (if possible), sexual activity, driving, and plane travel
- •
Adherence to pharmacological and non-pharmacological therapy
- •
Control of stress and anxiety through education programs, group therapy and different specialist consultations included in the CR program.
- •
Support from a social worker for patients to return to work
- •
Financial support from a social worker in cases of economic difficulties in obtaining essential medication and transport to the CR center.
- •
Follow-up in person in consultations, by phone and/or by mail, by physician and nurse
- •
Follow-up with coaching and motivational techniques, by psychologist and/or nurse.
- •
Clinical, exercise testing, echocardiogram, laboratory analysis and quality of life.
- •
Assessment of patients’ degree of satisfaction
- •
Assessment of the program's characteristics and conditions
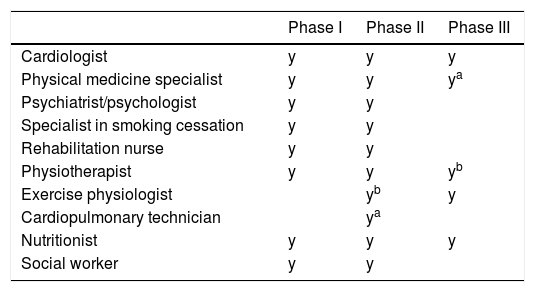
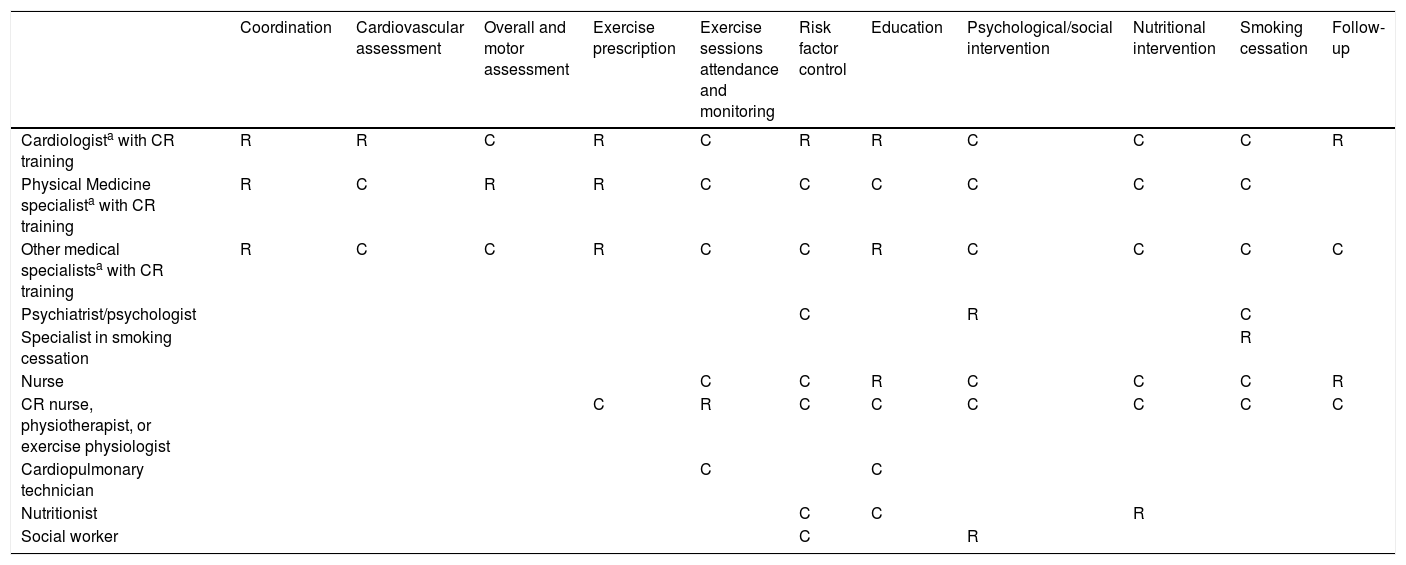
A multidisciplinary team is needed with specific tasks for each member (Tables 3 and 4).
Multidisciplinary team required in a cardiac rehabilitation program.
Roles of members of the multidisciplinary cardiac rehabilitation program team.
| Coordination | Cardiovascular assessment | Overall and motor assessment | Exercise prescription | Exercise sessions attendance and monitoring | Risk factor control | Education | Psychological/social intervention | Nutritional intervention | Smoking cessation | Follow-up | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiologista with CR training | R | R | C | R | C | R | R | C | C | C | R |
| Physical Medicine specialista with CR training | R | C | R | R | C | C | C | C | C | C | |
| Other medical specialistsa with CR training | R | C | C | R | C | C | R | C | C | C | C |
| Psychiatrist/psychologist | C | R | C | ||||||||
| Specialist in smoking cessation | R | ||||||||||
| Nurse | C | C | R | C | C | C | R | ||||
| CR nurse, physiotherapist, or exercise physiologist | C | R | C | C | C | C | C | C | |||
| Cardiopulmonary technician | C | C | |||||||||
| Nutritionist | C | C | R | ||||||||
| Social worker | C | R |
A local database is essential, and a national database would be desirable, bringing together data from national centers, as part of the SPC's National Center for Data Collection in Cardiology (CNCDC).
Internal assessment of the program should be performed through questionnaires evaluating patient satisfaction, analysis of individual and group gains, and indicators such as the proportion of eligible patients referred for CR and uptake and dropout rates.
External assessment should be performed periodically, using the mandatory criteria for CR, by independent entities that are responsible for accrediting and periodically checking centers.
Time phasesPhase I – hospital phaseThis is performed during hospital stay, beginning 24-48 hours after a non-complicated acute event.
A phase I program consists of early mobilization, low-intensity exercises, educational actions aimed at the adoption of a healthy lifestyle and control of risk factors, and encouragement to adhere to therapy and to participate in the following CR phases.2,25,26
Purposes- •
To avoid problems associated with prolonged immobilization: loss of postural reflexes, negative nitrogen balance, postural hypotension, atelectasis and pneumonia, thromboembolic phenomena, deconditioning, joint stiffness, muscle atrophy, depression, and urinary infections
- •
To identify and initiate control of risk factors
- •
To promote the adoption of a healthier lifestyle from the outset, working with both the patient and healthcare personnel
- •
To identify and minimize psychological disturbances caused by the acute event
- •
To establish a positive attitude that motivates the patient to continue the rehabilitation process and to take responsibility for long-term self-care with the help of professionals.
Individuals eligible for a phase I program are:
- •
Patients with acute coronary syndrome
- •
Patients with heart failure, including those undergoing cardiac transplantation (before and after)
- •
Patients with left ventricular assist or resynchronization devices, defibrillators or pacemakers
- •
Patients undergoing coronary artery bypass grafting or percutaneous coronary intervention
- •
Patients undergoing valve surgery or percutaneous implantation of prosthetic valves or clips
- •
Patients undergoing surgery to correct congenital heart disease.
Phase I begins as soon the patient stabilizes after the acute event, usually after 24-48 hours, according to the indication of the intensive care unit physician.
Before patients begin a phase I program, they should be assessed by the CR team, observing the admission criteria, contraindications and levels and progression of physical activity set out in the international guidelines.25,26
Exercise testing is not indicated in phase I. The intensity of exercise in this phase is defined by the subjective perception of effort as assessed by the Borg scale, without allowing heart rate to exceed resting heart rate by 20-30 bpm, according to the patient's clinical condition.27,28
Cardiac rehabilitation program teamThe core components of CR require the contribution of different health professionals. The composition of the multidisciplinary team may differ, but it will need to provide the knowledge and skills needed for the core components, inclusion of the following being mandatory:
- •
Cardiologist
- •
Physical medicine specialist
- •
Rehabilitation nurse/physiotherapist
- •
Nurse
- •
Nutritionist
- •
Psychologist/psychiatrist.
The CR team may need to request support from other specialist physicians, such as internists, endocrinologists or pneumologists, to manage the patients’ various comorbidities.
The program coordinator will be a cardiologist or other physician with qualifications in cardiac rehabilitation, recognized by the Order of Physicians.
Location and equipmentLocation
Many of the activities in Phase I are executed in bed – in the intensive care unit or in the ward, using areas located nearby, such as corridors and stairs.
Some centers subdivide Phase I into:
- •
Phase Ia – performed in the intensive care unit
- •
Phase Ib – performed in the ward.
If the department already has specific areas reserved for phase II, patients can be directed to this sector in the final part of phase Ib.
Ideally there will be a place for meetings used for individual and group educational activities (not mandatory in phase I).
Equipment
The following equipment is essential:
- •
Heart rate monitor or electrocardiograph (ECG) (by telemetry or portable monitor)
- •
Sphygmomanometer
- •
Scales
- •
Oximeter.
This phase covers patients after hospital discharge. It can be performed in the hospital, in a specialized CR center or, in some cases, at the patient's home.
In any of the above settings, the exercise program prescribed is individualized in terms of intensity, type (aerobic, continuous or interval, resistance), duration, frequency and modality.
Formal programs for patient education and lifestyle modification are considered essential components of this phase.
Purposes- •
To improve cardiovascular function, functional capacity, strength, balance and flexibility
- •
To optimize pharmacological therapy
- •
To detect and treat arrhythmias or hemodynamic and electrocardiographic changes occurring during exercise
- •
To educate the patient regarding how exercise and to remain active in the long term
- •
To work with the patient and their close family or caregiver to help them adopt a healthier lifestyle
- •
To improve the patient's psychological condition
- •
To individualize the exercise program in terms of intensity, duration, frequency, modality, and the type of physical activity
- •
To promote patients’ autonomy regarding their treatment program.
All patients who are eligible for phase I, whether or not they participate in this phase, are eligible for phase II. Besides these, individuals at high cardiovascular risk, diabetic, hypertensive and dyslipidemic patients, and smokers, may be indicated for phase II CR.
When to beginThe patient should start phase II as soon as possible, preferably within two weeks of discharge or after diagnosis (for non-hospitalized patients). If not begun before, it may be performed up to six months after the acute cardiac event.
The initial assessment and cardiovascular risk stratification (low, intermediate or high) is undertaken by the program's cardiologist. This stratification is based mainly on symptom severity, degree of left ventricular dysfunction, functional capacity, and the presence of residual ischemia or arrhythmias.29,30 Complementary exams required for this assessment include exercise testing (preferably cardiorespiratory testing in heart failure patients), echocardiogram (and other imaging methods if necessary), and 24-hour Holter monitoring (mostly for patients with arrhythmias).
Exercise testing is also essential for prescription of an exercise program, and is performed in all cases except in cases of complete patient incapacity.
In these specific and limited cases, possible alternatives are the six-minute walk test or other functional tests. Holter monitoring and new blood tests may be required.
At the end of this phase the patient should be reassessed to ascertain the extent to which the purposes were achieved, to quantify the gains of CR, and to help optimize therapy.
Cardiac rehabilitation program teamThe CR team to implement phase II should include:
- •
Cardiologist
- •
Physical medicine specialist
- •
Exercise specialist: physiotherapist, exercise physiologist or rehabilitation nurse
- •
Nutritionist
- •
Psychiatrist/psychologist
- •
Nurse
- •
Cardiopulmonary technician
The coordinator of a phase II CR program, as in phase I, should be a cardiologist or other certified physician with specific competence in cardiac rehabilitation.31 The coordinator is responsible for the efficacy and safety of the program and for defining the programs offered in the center according to pathology, as well as for ensuring that the members of the team have certification and training in basic life support and resuscitation. He or she should assess the patient's progress and the achievement of program outcomes, supervise the quality of care offered by the team, ensure the implementation of legislation, and produce periodic reports on the CR program's activities.31
Prescription of the intensity of aerobic exercise and other types of exercise (Tables 4 and 5) should be determined by the cardiologist, the exercise specialist's task being to apply this during the program's exercise sessions, informing the prescribing cardiologist of how the patient and the exercise specialist perceive the level of intensity, as well as the clinical response to the type of activity prescribed.
The exercise specialist coordinates exercise training under medical supervision and is responsible for the diversification and progression of training.
As a general rule, a ratio of one exercise specialist to 5-10 low- or intermediate-risk patients per session should be used. For high-risk patients, the ratio should be higher: one exercise specialist to 2-3 patients, according to severity.
During the training sessions, the cardiologist does not need to be present in the exercise room in most cases, but must be nearby and contactable to identify and rapidly intervene in the event of complications and to resolve questions regarding training or clinical problems, including adjustment of pharmacological therapy. In this case, health personnel with training in interpretation of ECG traces, such as a cardiopulmonologist, should always be present.
Location and equipmentLocation
- •
There should be at least 3-4 patients per session32
- •
Minimum area of 6 m2 for ergometry (cycle ergometer or treadmill)
- •
Dressing-room (ideally with shower)
- •
Waiting room
- •
Education room (which can be the exercise room).
It is not mandatory for complementary exams such as the exercise test, echocardiogram, Holter and other exams to be performed in the CR center, but these should be able to be performed rapidly in accredited centers.
Equipment
The CR program should offer different activities, if possible using various ergometers and other equipment for functional training, adapted to the needs of the target population.
As a minimum, the following should be available:
- •
Treadmills and cycle ergometers
- •
Elastic bands and weights
- •
Sphygmomanometer
- •
Chronometer
- •
Digital oximeter
- •
Continuous ECG monitoring, except for low-risk patients
- •
Cardiorespiratory resuscitation equipment including defibrillator and emergency cart
- •
Plan for urgent evacuation
Monitoring should be appropriate for the patient's cardiovascular risk level (Table 6), taking into account the risk due to the underlying disease, the program phase, and the time the patient has been participating in the program.
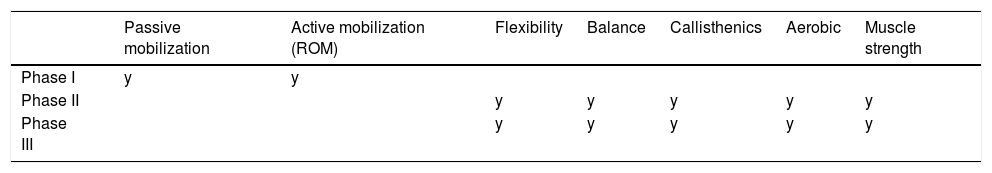
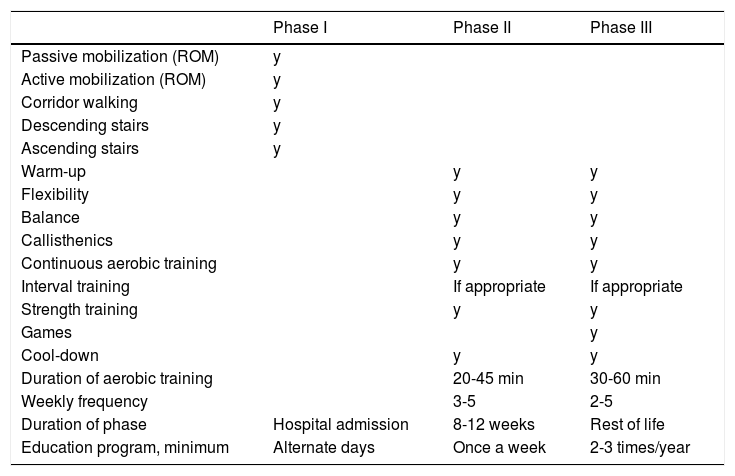
Minimal program in the different phases of a cardiac rehabilitation program.
| Phase I | Phase II | Phase III | |
|---|---|---|---|
| Passive mobilization (ROM) | y | ||
| Active mobilization (ROM) | y | ||
| Corridor walking | y | ||
| Descending stairs | y | ||
| Ascending stairs | y | ||
| Warm-up | y | y | |
| Flexibility | y | y | |
| Balance | y | y | |
| Callisthenics | y | y | |
| Continuous aerobic training | y | y | |
| Interval training | If appropriate | If appropriate | |
| Strength training | y | y | |
| Games | y | ||
| Cool-down | y | y | |
| Duration of aerobic training | 20-45 min | 30-60 min | |
| Weekly frequency | 3-5 | 2-5 | |
| Duration of phase | Hospital admission | 8-12 weeks | Rest of life |
| Education program, minimum | Alternate days | Once a week | 2-3 times/year |
ROM: range of movement; y: yes.
Low-risk patients can be monitored with a heart rate monitor only, while moderate- and high-risk patients need telemetry or continuous monitoring, at least during the first eight weeks.
Patients should be encouraged to wear sports shoes and loose, comfortable clothing.32
Integration between cardiac rehabilitation centers and attending physiciansFrom the outset, the phase II team should coordinate with the attending physicians (cardiologists, generalists, internists and others) and with phase III centers, in order to ensure the continuity of the patient's CR program.
Phase III centers should be coordinated by those of phase II, in terms of clinical assistance, education and training, and investigation.
Referral from a phase II to a phase III center should include a discharge report from phase II, to ensure the continuity of the intervention. This report should provide information on the patient's current situation and clinical and functional evolution, limitations, difficulties, and issues which need improvement.
Phase III – long-term phaseThe long-term phase usually begins after phase II, according to the physician's indication, and should last for the rest of the patient's life. This phase covers other low-risk patients who did not participate in phase II and are referred (six months or more after the acute event) by phase II CR centers, after medical assessment.
Purposes- •
To provide professional supervision of exercise, with clinical monitoring of symptoms and signs, heart rate, blood pressure and ECG (if required; only in high-risk patients)
- •
To teach self-monitoring
- •
To maintain patients’ awareness of the behavioral aspects of cardiovascular disease and the need to continue preventive measures (annually)
- •
To maintain long-term control of cardiovascular risk factors and adherence to pharmacological therapy and healthy lifestyles
- •
To ensure annual assessment of patients through clinical, functional (exercise test) and laboratory tests and echocardiogram (when indicated).
Patients with previously established indications for phases I and II CR programs, those who have completed phase II, and those who did not participate in phase II six or more months after the acute cardiac event, are eligible for long-term CR programs, if they are stable and present no contraindications.
When to beginAfter phase II, or as soon as they are identified if they have not participated in a phase II program.
Cardiac rehabilitation program teamIn this phase the minimum CR team should be composed of:
- •
Cardiologist, physical medicine specialist or other physician with competence in CR recognized by the Order of Physicians
- •
Exercise specialist: exercise physiologist or physiotherapist
Exercise specialists who implement the exercise sessions need to be certified to perform basic life support. Plans to deal with possible events, although rare, need to be rehearsed and contacts of the emergency team, transportation (ambulance) and referral hospitals need to be easily available. The presence of other health professionals is optional.
Location and equipmentLocation
Long-term programs should be implemented in sites that can accommodate a variety of activities, including games, aerobic exercise, walking, dancing, running, and strength exercises. In some cases they can occupy the same site as the phase II program.
The size of the space and type and structure of the location are dictated by the activities which are offered. It may include closed spaces and/or open spaces.
Some programs can home-based, especially in low-risk patients, which eliminates the need for travel to CR centers and removes problems with scheduling. Monitoring of parameters and periodic supervision by a team which includes a nurse or physiotherapist are essential in home-based programs.
Equipment
A variety of options should be provided, to fulfill the specific needs of each patient and to meet safety standards:
- •
Equipment for cardiopulmonary resuscitation, including emergency cart, defibrillator and certified team for immediate life support
- •
Facilities for monitoring high-risk patients (with the need for medical supervision, as in phase II)
- •
Ergometers (cycle, rowing and arm cycle ergometers, treadmills, and/or stair steppers (minimum areas as for phase II)
- •
Equipment for muscle training
- •
Equipment for functional training and non-competitive sports and recreational activities.
Following the norms defined in the international guidelines and based on the above criteria, which are crucial to ensure the quality of a CR program, it will be possible to obtain the benefits of CR demonstrated in randomized clinical trials, without increasing the patient's cardiovascular risk.
It is essential for every hospital cardiology department to offer phase I CR programs and to include a CR center (preferably inside the hospital) to which, following phase I, cardiovascular patients can be referred for phase II, directly and without impediment, in order to continue their CR program.
Links should then be established between hospitals and non-hospital outpatient centers, to offer long-term phase III CR, which in principle is for life. These outpatient centers may be located in health centers, community sport centers, or university sports faculties, in liaison with the originating hospital centers.
It is essential to carry out all components of the program, which should always performed by the multidisciplinary team. Liaison between the CR team coordinator and attending physicians (cardiologist and generalist) is crucial.
Only patient follow-up, promoting healthy lifestyles, continuation of pharmacological therapy and patients’ personal autonomy in the treatment of their disease, will enable long-term adherence and the success of the program.
Finally, home-based CR for low-risk patients, which will enable various problems to be overcome, needs to be introduced carefully and appropriately, following specific standards that are still to be defined.
Good clinical practice in CR, with quality programs, depends on thorough internal and external evaluation by means of audits, performed by experts and by patients.
The SPC is strongly committed to the implementation of CR programs and to the maintenance of their quality, through accreditation and evaluation of CR centers and competences, and certification of health personnel qualified for CR.
Conflicts of interestThe authors have no conflicts of interest to declare.