We report a case of temporary pacemaker lead malposition in the left ventricle crossing the interventricular septum (IVS). The majority of described cases occur due to a patent foramen ovale and are frequently incidental findings. A course across the IVS is rarely found and this complication with temporary leads is not even reported in the literature. This very rare location entails a risk of dangerous complications associated with left-to-right flow after lead removal. Echocardiography was an essential tool to diagnose the lead's course inside the heart and enabled secure removal of the lead with cardiac surgery backup.
Reportamos um caso de mau posicionamento de sonda de pacemaker temporário no ventrículo esquerdo com trajeto através do septo interventricular. A maioria dos casos descritos ocorre devido à existência de um foramen ovale patente e são frequentemente achados incidentais. O trajeto através do septo interventricular é raramente encontrado e esta complicação com sondas temporárias não está sequer descrita na literatura. Esta localização muito rara comporta um risco de complicações graves associadas a um fluxo esquerdo-direito após a remoção da sonda. A ecocardiografia foi uma ferramenta essencial para o diagnóstico do trajeto da sonda dentro do coração e permitiu a sua remoção de forma segura com backup de cirurgia cardíaca.
A 49-year-old male was admitted to the emergency department of our hospital during the night after two episodes of syncope in the previous two hours. The electrocardiogram (ECG) revealed advanced atrioventricular block with 3:1 conduction and heart rate of 35 bpm. Atropine was administered without chronotropic response. Blood tests were normal, with the exception of alcoholemia, which was 1.64 g/l. Meanwhile, reversion to sinus rhythm with bifascicular block (right bundle branch block and left posterior fascicular block) was documented. Given the risk of a new episode of syncope, a temporary pacemaker (PM) was implanted through the right femoral vein. The procedure was simple and uneventful, with lead position displaced slightly upward, but with good ventricular capture and low capture threshold.
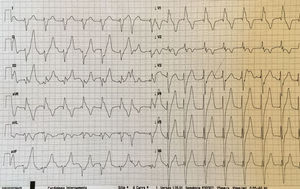
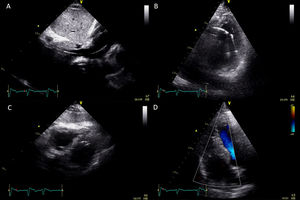
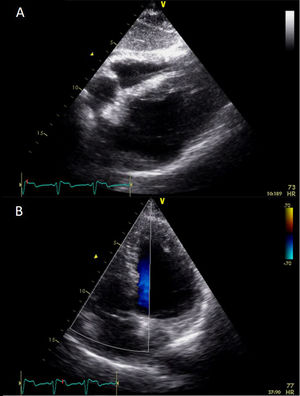
The patient remained monitored with telemetry, in sinus rhythm and asymptomatic until the next morning, when temporary pacing periods were detected. The ECG showed a paced right bundle branch block pattern (Figure 1), which raised the suspicion of an inappropriate lead position. Bedside echocardiography documented an anomalous course of the lead across the muscular portion of the intraventricular septum, with the tip in the left ventricle (LV) (Figure 2). There was no pericardial effusion and no shunt was detected with color Doppler. Biventricular systolic function was preserved.
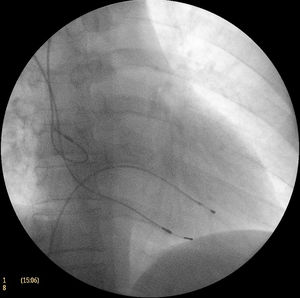
After discussion in the heart team, it was decided to first protect the patient from bradycardia by implanting a permanent PM and then to carefully remove the malpositioned lead. A dual-chamber permanent PM was implanted through the subclavian vein, with no complications. The course of the temporary lead could be visualized on fluoroscopy across the inferior vena cava and the heart, with the tip in the LV (Figure 3). The left ventricular lead was removed under the surveillance of a cardiac surgeon, the patient remaining hemodynamically stable and without complications.
At the end of the procedure, echocardiography confirmed the position of the PM leads in the right chambers, without pericardial effusion. After administration of agitated saline, no shunt was detected between right and left chambers (Figure 4). The patient progressed favorably, remained asymptomatic and was discharged from the hospital the next day. After three months he attended the pacemaker clinic and reported no related symptoms.
DiscussionMalposition of permanent pacemaker or cardiac defibrillator ventricular leads is a rare complication of pacemaker implantation.1 It may be overlooked by routine pacemaker interrogation and is frequently an incidental finding in asymptomatic patients. It is associated with an increased risk of thromboembolic events, and most patients are treated with lifelong anticoagulation, especially if the lead has been placed for a long time. However, if the diagnosis is made shortly after implantation, the lead should be removed percutaneously. Different locations have been described, including the LV. Lead displacement in the LV occurs most often due to a patent foramen ovale, whereas IVS perforation or crossing an interventricular septal defect are much rarer. Diagnosis and management can be very challenging. A right bundle branch block pattern on a 12-lead surface ECG is an important clue to the diagnosis, and should immediately raise the suspicion of displacement.2 Fluoroscopy is the mainstay imaging modality to guide lead placement, but echocardiography may be of value to detect a malpositioned lead, enabling location of the lead's course inside the heart. Although rare, this complication should be kept in mind, in order to enable early recognition and treatment and to avoid possible late complications such as thromboembolic events or endocarditis.
Conflicts of interestThe authors have no conflicts of interest to declare.