Implantable cardioverter-defibrillator (ICD) monitoring zones (MZ) provide passive features that do not interfere with the functioning of active treatment zones. However, it is not known for certain whether programming an MZ affects arrhythmia detection by the ICD. The aim of the present study is to assess the clinical relevance of MZ in a population of patients with ICDs.
MethodsIn this retrospective analysis of patients with ICDs, with or without cardiac resynchronization therapy, for primary prevention under remote monitoring, the MZ was analyzed and recorded arrhythmias were assessed in detail.
ResultsA total of 221 patients were studied (77% men; age 64±12 years). Mean ejection fraction was 30±12%. The mean follow-up was 63±35 months. One hundred and seventy-four MZ events were documented in 139 patients (62.9%): 74 of non-sustained ventricular tachycardia (NSVT), 42 of supraventricular tachycardia, 44 of atrial fibrillation/atrial flutter, and five cases of noise. Among the 137 patients who presented with arrhythmias in the MZ (excluding two cases with noise detection only), 22 (16.1%) received appropriate shocks and/or antitachycardia pacing (ATP), while of the other 84 patients, 15.5% received appropriate ICD treatment (p=NS). In patients who presented with NSVT in the MZ, 15 (20.5%) received appropriate shocks and/or ATP. In accordance with the MZ findings, physicians decided to change outpatient medication in 41.7% of all patients in whom arrhythmic events were reported.
ConclusionVentricular and supraventricular arrhythmias are common findings in the MZ of ICD patients. Programming an MZ is valuable in the diagnosis of arrhythmias and may be a useful tool in clinical practice.
A zona de monitorização (ZM) de cardioversor desfibrilhador implantável (CDI) permite uma funcionalidade passiva que não interfere com o funcionamento das zonas de tratamento ativo. Contudo, não é perfeitamente conhecido se a programação de ZM afeta a deteção de arritmias pelo CDI. O objetivo do presente estudo é avaliar a relevância clínica de ZM numa população submetida a implantação de CDI.
MétodosAnálise retrospetiva de doentes submetidos a implantação de CDI, com ou sem terapia de ressincronização cardíaca, em prevenção primária, sob monitorização remota. ZM foi analisada e as arritmias documentadas avaliadas em detalhe.
ResultadosForam estudados 221 doentes (77% homens; 64±12 anos). Fração de ejeção média foi 30±12%. O período de seguimento médio foi 63±35 meses. Foram documentados 174 eventos na ZM, em 139 doentes (62.9%): taquicardia ventricular não sustentada (TVNS) – 74, taquicardia supraventricular – 42, fibrilhação/flutter auricular – 44, ruído – 5. Dos 137 doentes que apresentaram arritmia na ZM (excluindo dois casos de deteção de ruído), 22 (16,1%) receberam choques apropriados ou pacing antitaquicardia (PAT), enquanto que dos restantes 84 doentes, 15,5% receberam terapias apropriadas do CDI (p=NS). Dos doentes que apresentaram TVNS na ZM, 15 (20,5%) receberam choques apropriados e/ou pacing anti-taquicardia (PAT). De acordo com os achados em ZM, o médico decidiu alterar a terapia oral de ambulatório em 41,7% de todos os doentes com eventos arrítmicos reportados.
ConclusãoArritmas ventriculares e supraventriculares são achados comuns na ZM de CDI. A programação de ZM é importante no diagnóstico de arritmias e poderá ser um elemento útil na prática clínica.
Implantable cardioverter-defibrillators (ICDs) are the treatment of choice for primary prevention against sudden cardiac death.1 Arrhythmia therapy is delivered in the form of antitachycardia pacing (ATP) or shock. An ICD is able to terminate potentially life-threatening ventricular arrhythmias, preventing syncope, hypotension and, most importantly, sudden cardiac death. Device algorithms and thresholds for detection and therapies are programmed according to age, indication and the underlying cardiac disease.2
For lower heart rates, monitoring zones (MZ), in which the device does not deliver therapy but monitors the heart rhythm, are commonly used in clinical practice. MZ provide passive features that do not interfere with the functioning of active treatment zones. MZ can also classify events as supraventricular or ventricular arrhythmias.3 However, it is not known for certain whether the programming of an MZ affects arrhythmia detection by the ICD or the clinical management of these patients.
The aim of the present study is to assess the benefit in clinical practice of MZ for treatment in a population of patients with ICDs or cardiac resynchronization therapy-defibrillator (CRT-D) devices for primary prevention.
MethodsThis was a retrospective analysis of patients implanted with an ICD or CRT-D for primary prevention at a tertiary center between 2006 and 2015. Devices were implanted according to international guidelines.4 Patients with indication for implantation for secondary prevention were excluded.
All patients with a programmed MZ were considered for the study. This zone was programmed according to heart rate (140-170 bpm) and persistence (number of consecutive cycles >50). Therapy zones were programmed for 170-200 bpm for 30 out of 40 cycles (ATP attempts or shock), and >200 bpm for 12 out of 18 cycles (ATP during charge or shock).
The MZ criteria were changed according to the arrhythmia data obtained via the device during follow-up. ATP-based therapy was activated only in patients presenting with slow VT (below the cut-off of 170 bpm).
All enrolled patients received a remote monitoring (RM) system. The RM equipment was provided at the first outpatient visit after ICD or CRT-D implantation and reports were reviewed by trained staff under the supervision of a senior electrophysiologist.
Initially a retrospective analysis was performed of MZ reports through the RM system and recorded arrhythmias were assessed in detail. In patients with single-chamber devices, atrial fibrillation (AF) detection was based on heart rate combined with absence of stability criteria, according to cycle length irregularity during the arrhythmia. Sinus tachycardia, supraventricular tachycardia and non-sustained ventricular tachycardia (NSVT) were differentiated by the onset criteria and using comparison with native QRS complex morphology and cycle length. In patients with arrhythmic events documented in the MZ, the decision of the physician at the outpatient clinic visit regarding the treatment approach was analyzed by reviewing patient files. A second analysis of MZ reports through RM systems was then performed to determine the impact of changes in medication or invasive strategy on the recurrence of arrhythmic events. For all patients, data were collected regarding arrhythmic events, device programming and appropriate and inappropriate therapies via ICD or CRT-D.
Statistical analysisThe statistical analysis was performed using IBM SPSS Statistics, version 19 (IBM SPSS, Chicago, IL). Continuous variables were expressed as mean ± standard deviation and categorical variables were expressed as percentage. Study groups were compared using the Student's t test or the Wilcoxon-Mann-Whitney test for continuous variables, and Pearson's chi-square or Fisher's exact test for categorical measures, as appropriate. A p-value <0.05 was considered statistically significant.
ResultsDuring the study period, 898 patients underwent ICD and CRT-D implantation, of whom 221 received the device for primary prevention with facilities for RM. The baseline characteristics of the study population are shown in Table 1. Of the overall population, 77% were men, mean age was 64±12 years, and mean left ventricular ejection fraction was 30±12%. Dilated and ischemic cardiomyopathy were the most common underlying conditions, followed by hypertrophic cardiomyopathy, primary electrical cardiac disease and congenital heart disease.
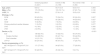
Baseline characteristics of the study population.
| Overall population (n=221) | Events in MZ (n=139) | No events in MZ (n=82) | p | |
|---|---|---|---|---|
| Age, years | 64±12 | 64.7±12.4 | 63.0±15.1 | 0.364 |
| Male, n (%) | 170 (76.9%) | 103 (74.1%) | 67 (81.7%) | 0.120 |
| LVEF, % | 30±12 | 27.6±11.0 | 33.5±12.0 | 0.002 |
| Etiology, n (%) | ||||
| DCM | 95 (43.0%) | 75 (54.0%) | 20 (24.4%) | 0.007 |
| ICM | 94 (42.5%) | 50 (36.0%) | 44 (53.6%) | 0.027 |
| HCM | 15 (6.8%) | 7 (5.0%) | 8 (9.8%) | 0.237 |
| Primary electrical cardiac disease | 11 (5.0%) | 3 (2.2%) | 8 (9.8%) | 0.077 |
| CHD | 4 (1.8%) | 3 (2.2%) | 1 (1.2%) | 0.300 |
| VHD | 2 (0.9%) | 1 (0.6%) | 1 (1.2%) | 1.000 |
| Device, n (%) | <0.001 | |||
| ICD | 138 (62.4%) | 73 (52.5%) | 65 (79.3%) | |
| Single-chamber | 124 (89.9%) | 65 (47.1%) | 59 (42.8%) | |
| Dual-chamber | 14 (10.1%) | 8 (5.8%) | 6 (4.3%) | |
| CRT-D | 83 (37.6%) | 66 (47.5%) | 17 (20.7%) | |
| Device programming, n (%) | ||||
| MZ 140 bpm/VT 170 bpm/VF 210 bpm | 171 (77.4%) | 94 (67.6%) | 77 (93.9%) | |
| MZ 140 bpm/VT 170 bpm/VF 214 bpm | 50 (22.6%) | 45 (32.4%) | 5 (6.1%) | |
CHD: congenital heart disease; CRT-D: cardiac resynchronization therapy-defibrillator; DCM: dilated cardiomyopathy; HCM: hypertrophic cardiomyopathy; ICD: implantable cardioverter-defibrillator; ICM: ischemic cardiomyopathy; LVEF: left ventricular ejection fraction; MZ: monitoring zone; VHD: valvular heart disease.
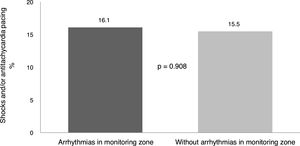
Mean follow-up after implantation was 63±35 months, during which MZ data were collected. One hundred and seventy-four events were documented in the MZ in 139 patients (62.9% of the overall population) (Figure 1). Supraventricular arrhythmias accounted for almost half of all findings (49.4%), with a similar incidence of supraventricular tachycardia and AF/atrial flutter. In 29 patients (20.9%), AF and other supraventricular arrhythmias were diagnosed based on electrograms from single-chamber ICDs. NSVT occurred in 74 patients (42.5% of all events) in the MZ. Only five events were due to noise. Regarding ICD therapy delivery, of the 137 patients who presented arrhythmic events in the MZ (excluding two patients with noise detection only), 22 (16.1%) received appropriate shocks and/or ATP, while in the other 84 patients without events in the MZ, 15.5% received appropriate ICD therapies (p=0.908) (Figure 2). In patients with NSVT in the MZ the frequency of appropriate ICD therapy was not significantly different from the others, with 15 patients (20.5%) receiving device therapy.
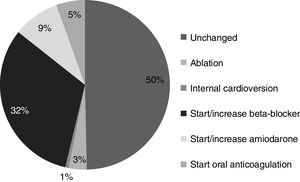
In accordance with the MZ findings, physicians decided to change outpatient medication in 58 patients (41.7% of all patients in whom arrhythmic events were reported in the MZ), due to supraventricular arrhythmia in 24 cases and to ventricular tachycardia in 34. In the presence of NSVT in the MZ, the initiation or titration of antiarrhythmic drugs (mainly beta-blockers and amiodarone) was based on the presence of symptoms and/or NSVT length and burden. Among these 58 subjects, six started beta-blockers, 11 started amiodarone, and eight (13.8%) started chronic oral anticoagulation. The previously prescribed antiarrhythmic drug dosage was titrated in 44 patients. Beta-blocker dosage was increased in 41 patients and amiodarone/sotalol dosage was increased in three cases. In addition to optimization of medical treatment, two patients underwent ablation of supraventricular arrhythmias detected in the MZ (atrial flutter and atrioventricular nodal reentrant tachycardia) and three underwent atrioventricular junction ablation due to AF with rapid ventricular response (and low percentage of biventricular pacing). Furthermore, internal cardioversion via the ICD was performed in one patient with persistent AF (Figure 3). Since there was uncertainty whether the AF burden justified oral anticoagulation, the initiation of this medication was based on the physician's decision. However, in view of the high risk in this population, patients presenting AF episodes lasting >5 min were prescribed anticoagulation therapy.
After optimization of medical therapy, 37 patients (63.8%) did not have recurrence of arrhythmic events in the MZ, 70.8% in the supraventricular arrhythmia subgroup and 55.6% in the ventricular tachycardia subgroup. In those with recurrence, 16 individuals presented NSVT episodes, five showed supraventricular tachycardia and two had paroxysmal AF. In three cases there was more than one type of arrhythmia. Despite changes in medication, 15 patients (25.9%) had recurrence of the same arrhythmia.
Among the 65 patients with NSVT, in whom antiarrhythmic medication was increased, during a follow-up of 10.0±7.5 months no appropriate therapies were delivered by the device, and more than half (55.6%) did not present recurrence of documented arrhythmias in the MZ. In the overall population, arrhythmic events in the MZ were detected in 62.9%, which led to treatment changes in 27.1%, with a consequent 17% decrease in the arrhythmic events detected in the MZ. There were no clinical or technical complications reported in relation to the activation of MZ.
DiscussionProgramming an MZ for primary prevention in ICD patients leads to the detection of symptomatic or asymptomatic arrhythmias, indicating that it may be a useful tool in the optimization of medical and interventional treatment in this population.
The benefits of RM in preventing hospital admission for heart failure or cardiovascular death are well documented.5–7 However, its usefulness in optimization of antiarrhythmic treatment has not been so extensively studied. As highlighted in the present study, RM enables early detection of new-onset or paroxysmal arrhythmias in the MZ and hence early therapeutic intervention.
In our sample, arrhythmic events were documented in the MZ in 62.9% of patients. These findings had a significant impact on clinical practice, since in half of the patients outpatient medication was changed and/or ablation was performed. This optimization in patient management resulted in a considerable reduction in arrhythmic events reported in the MZ.
As previously reported, patients with cardiac devices presented a high incidence of atrial arrhythmias, even in the absence of symptoms.8 Around 50% of ICD carriers can be expected to experience AF during the lifetime of the device.9 In our population, new-onset paroxysmal AF/atrial flutter was found in a significant proportion of patients (20%), leading to the initiation of oral anticoagulation. This incidence is similar to data reported by Ricci et al., who found an AF incidence of 26% in pacemaker/ICD patients.10 Since AF, even if paroxysmal or asymptomatic, is associated with a five-fold increase in the risk of ischemic stroke,11 recognition of these episodes and initiation of anticoagulation may provide protection against thromboembolic events such as stroke. Programming an MZ provides valuable information on AF occurrence, AF burden and consequent stroke risk. These continuous monitoring data (particularly when combined with RM systems) can be of considerable value, since many AF episodes with clinically significant duration are asymptomatic.12 Improvements in use of and adherence to oral anticoagulation based on continuous ICD monitoring have recently been demonstrated.13
The impact of appropriate shocks on quality of life and morbidity in ICD patients remains a concern,14–16 and reducing the rate of shock therapies is a real challenge for the ICD outpatient clinic. Initiation or titration of antiarrhythmic drugs in patients with NSVT documented in the MZ has the potential to reduce the rate of shocks and ATP delivered to patients. In fact, in our population, among patients with NSVT whose antiarrhythmic medication was optimized no shocks or ATP were delivered via the device, and 55.6% of these patients did not present recurrence of documented arrhythmias in the MZ. Since NSVT is associated with an increased risk of death in both ischemic16 and non-ischemic cardiomyopathy,17–19 its detection and consequent therapeutic optimization can potentially reduce ICD therapies in these patients.
It is also important to emphasize that in our study, regardless of the type of arrhythmia recorded, analysis of the MZ had the potential to change physicians’ decisions in 27.1% of cases, with an impact on arrhythmia recurrence.
There have been concerns that MZ can be associated with increased risk of inappropriate device therapy,20,21 however in our study only two patients (0.9%) received inappropriate therapies due to AF with rapid ventricular response. This incidence is much lower than that described in the Detect Supraventricular Tachycardia Study, in which the rate of inappropriate detection of supraventricular tachycardias was 31%,22 or in a study by van Rees et al. of a prospective registry, with 13% of inappropriate shocks.23 High-rate cut-off programming for detection and therapy in primary prevention has been shown to decrease this rate substantially to 6.6%.24
The present study showed that continuous rhythm monitoring by the cardiac device unmasks arrhythmias in asymptomatic and symptomatic patients, with an impact on clinical management, leading to a significant decrease in arrhythmic events detected in the MZ.
Study limitationsThis is an observational long-term retrospective study with the inherent limitations, including the absence of a control group. The relatively small sample size results from the single-center nature of the study. However, our results reflect a real-life long-term clinical practice experience based on an RM program.
ConclusionDetection of spontaneous ventricular and supraventricular arrhythmias are common findings in a population with implantable cardiac devices for primary prevention with a programmed MZ. The MZ appears to be of value in the diagnosis of arrhythmias, and may be a useful tool in clinical practice. In our study, the treatment approach was changed in about half of the patients based on MZ reports. It is also important to emphasize that anticoagulation was started in patients with previously unknown paroxysmal AF, providing an important measure in stroke prevention.
Conflicts of interestThe authors have no conflicts of interest to declare.