Coronavirus disease (COVID-19) has led to significant changes in healthcare systems and its impact on the treatment of cardiovascular conditions, such as ST-elevation myocardial infarction (STEMI), is unknown in countries where the healthcare systems were not saturated, as was the case in Portugal. As such, we aimed to assess the effect on STEMI admissions and outcomes in Portuguese centers.
MethodsWe conducted a single-center, observational, retrospective study including all patients admitted to our hospital due to STEMI between the date of the first SARS-CoV-2 case diagnosed in Portugal and the end of the state of emergency (March and April 2020). Patient characteristics and outcomes were assessed and compared with the same period of 2019.
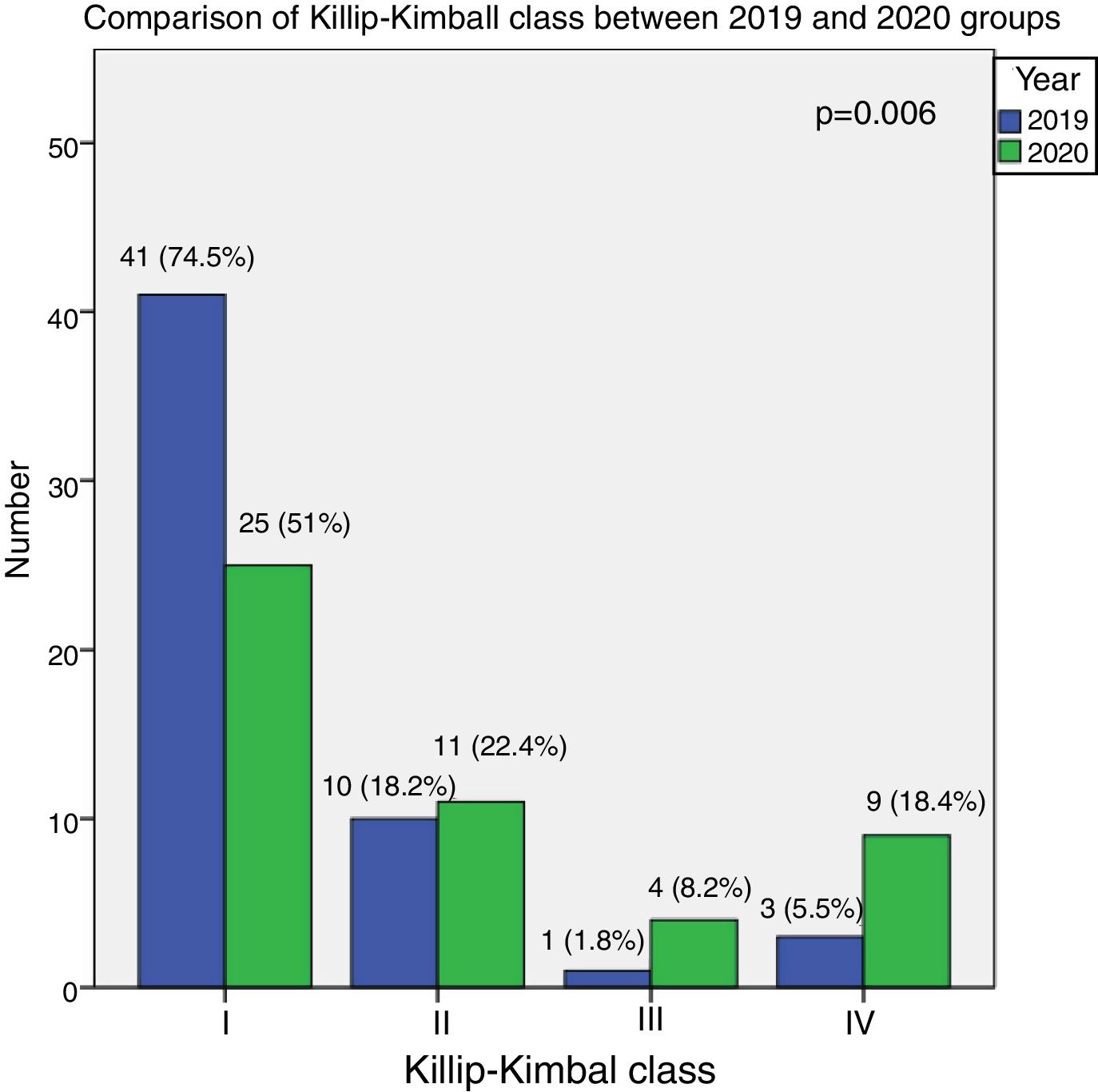
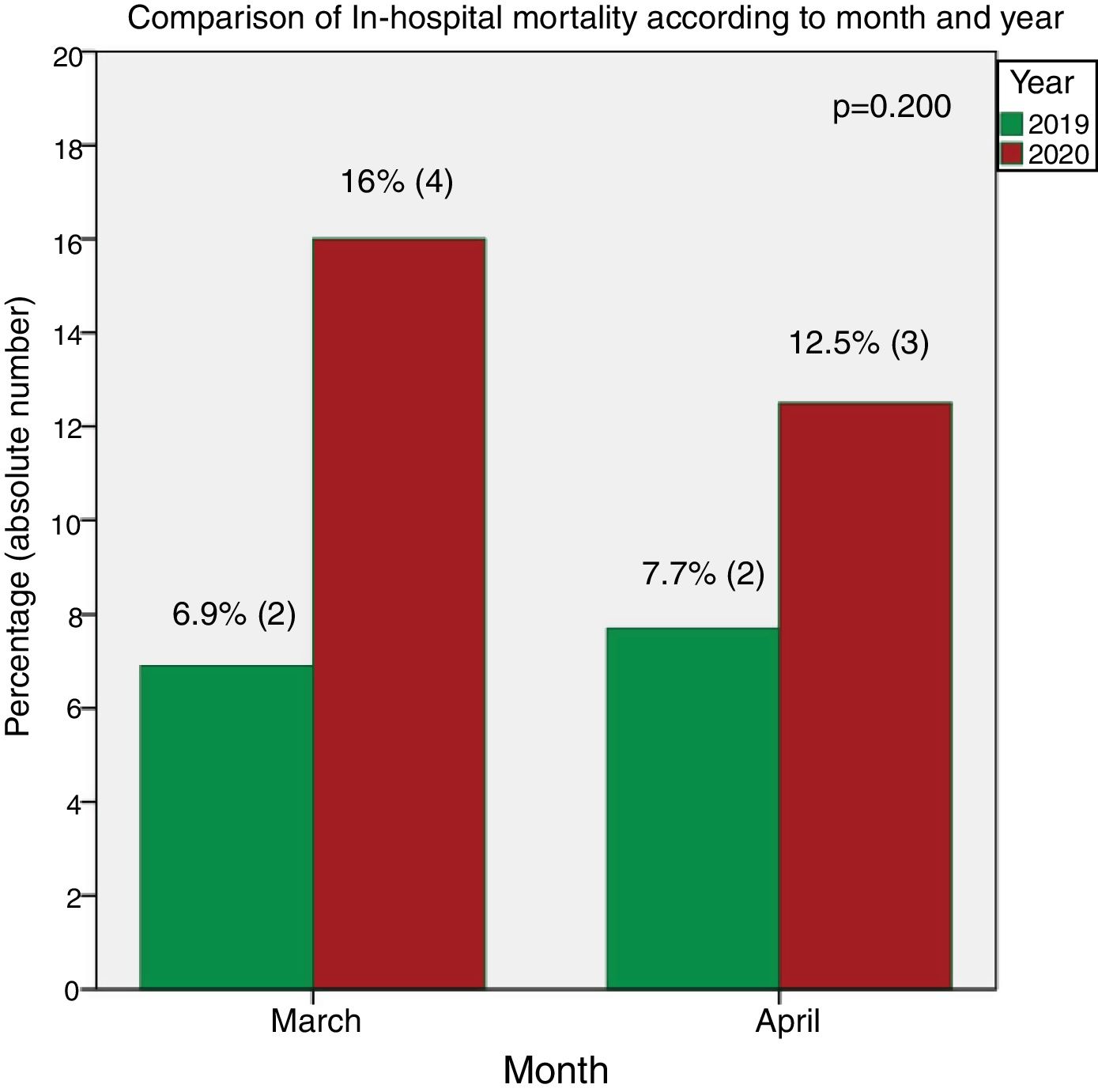
ResultsA total of 104 STEMI patients were assessed, 55 in 2019 and 49 in 2020 (-11%). There were no significant differences between groups regarding age (62±12 vs. 65±14 years, p=0.308), gender (84.8% vs. 77.6% males, p=0.295) or comorbidities. In the 2020 group, there was a significant decrease in the proportion of patients transported to the hospital in pre-hospital emergency medical transportation (38.2% vs. 20.4%, p=0.038), an increase in system delay (49 [30-110.25] vs. 140 [90-180] minutes, p=0.019), a higher Killip-Kimball class, with a decrease in class I (74.5% vs. 51%) and an increase in class III (1.8% vs. 8.2%) and IV (5.5% vs. 18.4%) (p=0.038), a greater incidence of vasoactive support (3.7% vs. 26.5%, p=0.001), invasive mechanic ventilation usage (3.6% vs. 14.3%, p=0.056), and an increase in severe left ventricular dysfunction at hospital discharge (3.6% vs. 16.3%, p=0.03). In-hospital mortality was 14.3% in the 2020 group and 7.3% in the 2019 group p=0.200).
ConclusionDespite a lack of significant variation in the absolute number of STEMI admissions, there was an increase in STEMI clinical severity and significantly worse outcomes during the SARS-CoV-2 pandemic. An increase in system delay, impaired pre-hospital care and patient fear of in-hospital infection can partially justify these results and should be the target of future actions in further waves of the pandemic.
A doença por coronavírus 2019 (COVID-19) originou alterações significativas nos sistemas de saúde e a sua influência no tratamento da patologia cardiovascular, como no caso do enfarte agudo do miocárdio com supradesnivelamento do segmento ST (EAMcSST), é desconhecida em países onde não ocorreu saturação da capacidade dos sistemas de saúde, como é o caso de Portugal. Assim, o nosso objetivo foi determinar o efeito nas admissões por EAMcSST e no seu prognóstico intra-hospitalar na região Centro de Portugal.
MétodosRealizou-se um estudo unicêntrico, observacional e retrospetivo, incluindo todos os doentes admitidos no nosso hospital por EAMcSST entre a data do primeiro caso de SARS-CoV-2 em Portugal e o término do estado de emergência (março e abril de 2020). Foram avaliadas as características e os resultados dos doentes e foi realizada uma comparação com o período homólogo de 2019.
ResultadosForam incluídos 104 doentes com EAMcSST, 55 em 2019 e 49 em 2020 (-11%). Não se verificaram diferenças significativas entre os grupos relativamente à idade (62±12 versus 65±14 anos, p=0,308), género (84,8% mulheres versus 77,6% homens, p=0,295) ou comorbilidades. No grupo de doentes de 2020 verificou-se uma diminuição significativa na proporção de doentes transportados para o hospital pela viatura médica do Instituto Nacional de Emergência Médica (38,2% versus 20,4%, p=0,038), um aumento no atraso do sistema de saúde (49 [30-110,25] versus 140 [90-180] minutos, p=0,019), uma maior classe Killip-Kimball, com uma redução de doentes em classe I (74,5% versus 51%) e um aumento na classe III (1,8% versus 8,2%) e IV (5,5% versus 18,4%) (p=0,038), uma maior incidência de suporte vasoativo (3,7% versus 26,5%, p=0,001), de ventilação mecânica invasiva (3,6% versus 14,3%, p=0,056) e um aumento da proporção de doentes com disfunção ventricular esquerda grave na alta hospitalar (3,6% versus 16,3%, p=0,03). A mortalidade intra-hospitalar foi de 14,3% no grupo de 2020 e de 7,3% no grupo de 2019 (p=0,200).
ConclusãoApesar de não se ter verificado uma variação significativa no número de admissões por EAMcSST, existiu um aumento da gravidade, com um prognóstico intra-hospitalar significativamente mais adverso durante a pandemia por SARS-CoV-2. Um aumento no atraso do sistema de saúde, um compromisso nos serviços pré-hospitalares e o receio por parte dos doentes de contraírem uma eventual infeção hospitalar podem justificar parcialmente estes resultados e devem ser planeadas ações para diminuir o seu efeito em novos surtos pandémicos.
The global pandemic caused by the novel acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in a newly termed coronavirus disease 2019 (COVID-19).1 Given its exponential growth in many European countries, patients with COVID-19 overwhelmed the emergency department (ED), medical floors, intensive care unit resources, personal protective equipment supplies, and medical staff. Healthcare systems, including the Portuguese Public Health Service, reduced elective procedures and outpatient clinic appointments to prepare for and manage infected patients. In Portugal, the first positive SARS-CoV-2 patient was documented on 2 March and the Government declared a nationwide lockdown on 16 March. The following week, on 22 March, a state of emergency was declared, severely reducing individual liberties and freedom of movement.2 Reflecting the implementation of early lockdown measures, and despite sharing its single, 1200 km long border with the hardest hit country in Western Europe, the progression of admissions and deaths was milder than in Spain, particularly in the central region of Portugal. The Portuguese Health System did not become saturated, especially pre-hospital care and the intensive care units (peak occupation was at around 30%). In the first pandemic wave, Portugal had one of the lowest case fatality ratios per million in Western Europe.3
The effect of the COVID-19 pandemic on medical care for non-COVID-19 conditions has been difficult to quantify. A decrease in ED admissions was detected, as well as a sudden rise in cardiac arrests in the field and a reduction in stroke patients treated with fibrinolysis due to a delay in medical presentation.4 A decrease in care for patients with acute cardiac conditions such as acute myocardial infarction (MI) may have deleterious consequences, since delayed treatment increases the incidence of sudden cardiac death or heart failure (HF). Indeed, a reduction in MI during the first months of the COVID-19 pandemic was recorded, as well as an increase in overall mortality, especially in highly affected countries as Italy and Spain.5–8 In Portugal, a sharp increase in all-cause mortality after March 2020 was observed well beyond that attributed solely to COVID-19 deaths.9 However, as Portuguese ST-elevation myocardial infarction (STEMI) referral network (Via Verde Coronária) maintained its responsiveness, we speculate whether other factors, including the fear of going to hospital, had a significant impact on the number of STEMI patients admitted to the ED.4
We therefore sought to compare the number of STEMI patients admitted to our ED in March and April 2020 with the same period of 2019. Additionally, we investigated whether patient outcomes were similar in both time periods.
MethodsStudy design and demographicsWe conducted an observational, retrospective study of all patients admitted to our hospital due to STEMI, including acute and sub-acute presentations, encompassing March and April 2020, i.e., between the first SARS-CoV-2 case in Portugal and the end of the state of emergency. Taking into consideration the seasonality of STEMI, we compared this period with the same months in 2019.
Our hospital is located in Coimbra, in the central region (NUTS I) of Portugal. It is a tertiary referral center, serving as the primary percutaneous coronary intervention (PPCI) hub for a population of 1.5 million inhabitants. We perform 350 PPCI per year and the hospital is integrated in the Portuguese STEMI referral network.10 STEMI diagnosis was given according to the Fourth Universal Myocardial Infarction Definition.11 All patients admitted during this period were systematically tested for SARS-CoV-2 by polymerase chain reaction after coronarography and had negative tests.
We collected data on patient characteristics and origin, patient and system delays, clinical evolution and outcomes. The primary endpoint was the number of STEMI patients admitted and the secondary endpoint was established as all-cause in-hospital mortality of STEMI patients. Left ventricular dysfunction was classified as severe if left ventricular ejection fraction (LVEF) was <35%. Patient delay was the time from symptom onset to first medical contact (FMC) or to national emergency call. System delay was the time from FMC or national emergency call to reperfusion therapy. Vasoactive support was considered when inotropes (dobutamine, adrenaline) or vasopressors (noradrenaline, dopamine) were prescribed.
The study protocol was approved by the Centro Hospitalar e Universitário de Coimbra Ethics Committee and complies with the Declaration of Helsinki.
Statistical analysisCategorical variables were expressed in frequencies and percentages and continuous variables as mean and standard deviation or median and interquartile ranges for variables with or without normal distribution, respectively. The Qui squared test was used to assess differences between categorical variables, including in-hospital mortality, and the Student's T test, or the Mann-Whitney U test was used to compare continuous variables with or without normal distribution, respectively. The Kolmogorov-Smirnov test was employed to test for the normality of distribution of continuous variables. Primary outcome was assessed using the unpaired Student's t test to compare the mean of the weekly number of STEMI patients. Statistical significance was accepted for p<0.05. Statistical analysis was performed using IBM SPSS Statistics version 23 (IBM, Armonk, New York) software.
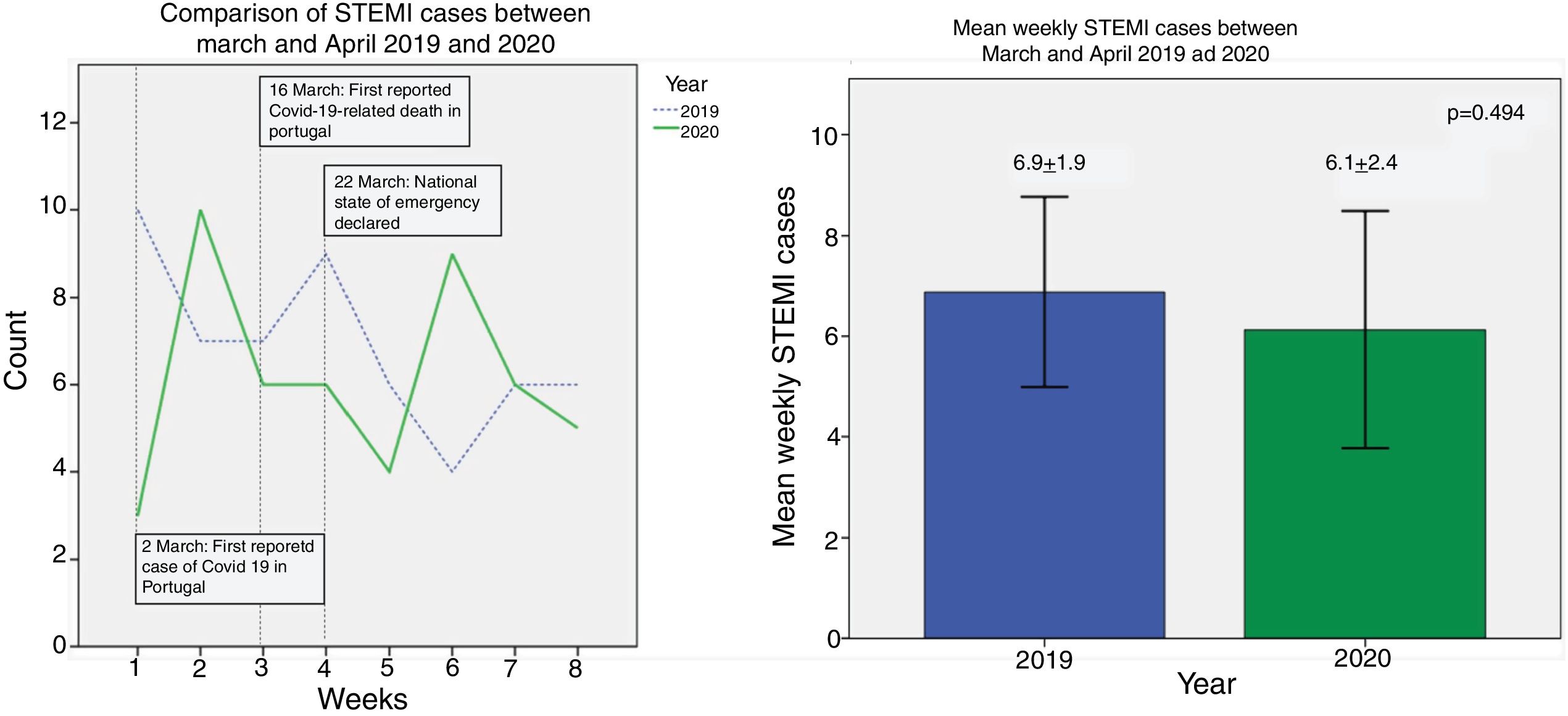
ResultsA total of 104 STEMI patients were assessed. There were 55 STEMIs in March and April 2019 and 49 STEMIs in the same period of 2020, a reduction of 11%. The mean weekly number of STEMIs was similar between periods, at 6.9±1.9 cases in 2019 and 6.1±2.4 cases in 2020, p=0.494. Also, some variation is usually present among STEMI incidence across months (Figure 1A and B). In January and February 2019, 50 STEMI patients were treated (-9% vs. March and April), whereas in May and June, 58 cases were registered (+5% vs. March and April).
(a) Weekly ST-elevation myocardial infarction (STEMI) admissions from week 1 (starting on 1 March) to week 8 (ending on 31 May). A decrease was evident in the first week, but afterwards, the incidence was similar over the weeks. (b) Comparison of mean weekly STEMI admissions showing a similar incidence between years. STEMI: ST-elevation myocardial infarction.
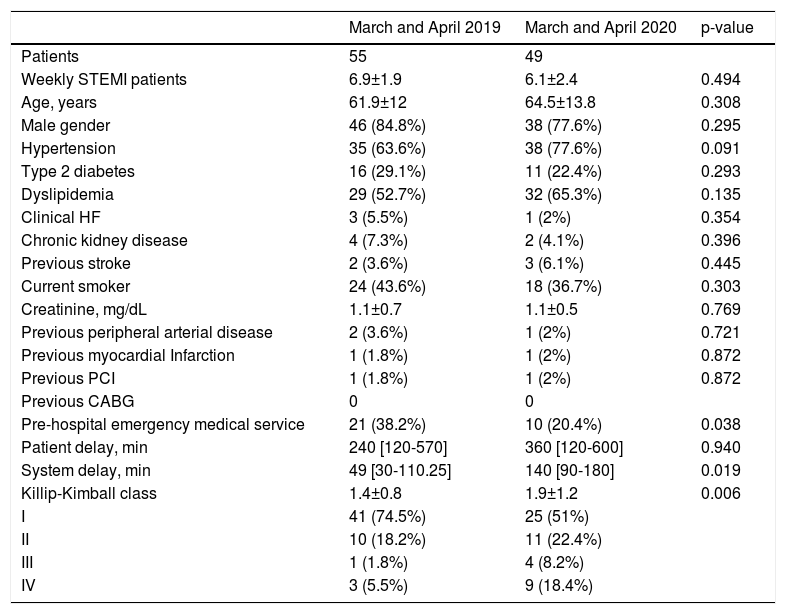
The baseline characteristics in both populations are presented in Table 1 and Table 2. No significant differences were found among groups (2019 vs. 2020) regarding age (62±12 vs. 65±14 years, p=0.308), gender (84.8% vs. 77.6% males, p=0.295), or comorbidities, including systemic arterial hypertension, type 2 diabetes, chronic kidney disease, smoking status or prior history of HF or stroke.
Comparison of STEMI patients’ baseline characteristics between March and April 2020 versus the same period of 2019. Categorical variables are expressed in frequencies, and percentages and numerical variables in means and standard deviations.
| March and April 2019 | March and April 2020 | p-value | |
|---|---|---|---|
| Patients | 55 | 49 | |
| Weekly STEMI patients | 6.9±1.9 | 6.1±2.4 | 0.494 |
| Age, years | 61.9±12 | 64.5±13.8 | 0.308 |
| Male gender | 46 (84.8%) | 38 (77.6%) | 0.295 |
| Hypertension | 35 (63.6%) | 38 (77.6%) | 0.091 |
| Type 2 diabetes | 16 (29.1%) | 11 (22.4%) | 0.293 |
| Dyslipidemia | 29 (52.7%) | 32 (65.3%) | 0.135 |
| Clinical HF | 3 (5.5%) | 1 (2%) | 0.354 |
| Chronic kidney disease | 4 (7.3%) | 2 (4.1%) | 0.396 |
| Previous stroke | 2 (3.6%) | 3 (6.1%) | 0.445 |
| Current smoker | 24 (43.6%) | 18 (36.7%) | 0.303 |
| Creatinine, mg/dL | 1.1±0.7 | 1.1±0.5 | 0.769 |
| Previous peripheral arterial disease | 2 (3.6%) | 1 (2%) | 0.721 |
| Previous myocardial Infarction | 1 (1.8%) | 1 (2%) | 0.872 |
| Previous PCI | 1 (1.8%) | 1 (2%) | 0.872 |
| Previous CABG | 0 | 0 | |
| Pre-hospital emergency medical service | 21 (38.2%) | 10 (20.4%) | 0.038 |
| Patient delay, min | 240 [120-570] | 360 [120-600] | 0.940 |
| System delay, min | 49 [30-110.25] | 140 [90-180] | 0.019 |
| Killip-Kimball class | 1.4±0.8 | 1.9±1.2 | 0.006 |
| I | 41 (74.5%) | 25 (51%) | |
| II | 10 (18.2%) | 11 (22.4%) | |
| III | 1 (1.8%) | 4 (8.2%) | |
| IV | 3 (5.5%) | 9 (18.4%) |
CABG: coronary artery bypass graft; HF: heart failure; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction.
Comparison of in-hospital data and evolution of ST-elevation myocardial infarction patients between March and April 2020 versus the same period of 2019. Categorical variables are expressed in frequencies and percentages and numerical variables in means and standard deviations.
| March and April 2019 | March and April 2020 | p-value | |
|---|---|---|---|
| Fibrinolysis | 2 (3.6%) | 7 (14.3%) | 0.056 |
| Interhospital transfer | 21 (38.2%) | 25 (51%) | 0.132 |
| Cardiorespiratory arrest at admission | 5 (9.1%) | 4 (13.3%) | 0.396 |
| Successful PCI | 55 (100%) | 46 (93.9%) | 0.101 |
| Multi vessel disease | 34 (61.8%) | 26 (53.1%) | 0.241 |
| Mechanical ventilation | 2 (3.6%) | 7 (14.3%) | 0.056 |
| Ischemia after PCI | 10 (18.5%) | 8 (16.3%) | 0.488 |
| Arrhythmia after PCI | 4 (7.4%) | 6 (12.2%) | 0.310 |
| Vasoactive support | 2 (3.7%) | 13 (26.5%) | 0.001 |
| Need for non-culprit PCI | 16 (29.1%) | 13 (26.5%) | 0.517 |
| Discharge LVEF, % | 47.5±11.1 | 43.9±13.8 | 0.225 |
| LVEF<35% at discharge | 2 (3.6%) | 8 (16.3%) | 0.03 |
| In-hospital death | 4 (7.3%) | 7 (14.3%) | 0.200 |
| • Before primary PCI (in the ED) | 1 (25%) | 2 (28.6%) | 0.721 |
| • Within 24h of admission | 1 (25%) | 1 (14.3%) | 0.618 |
| • After 24h and within first week | 1 (25%) | 3 (42.9%) | 0.530 |
| • After first week of admission | 1 (25%) | 1 (14.3%) | 0.618 |
| • Anoxic encephalopathy-associated | 0 | 1 (14.3%) | 0.636 |
ED: emergency department; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention.
In the 2020 group, there was a significant decrease in the proportion of patients transported to the hospital by pre-hospital emergency medical services (38.2% vs. 20.4%, p=0.038), showing an increased trend in patients who underwent fibrinolysis (3.6% vs. 14.3%, p=0.056) and a non-significant increase in interhospital transfers (38.2% vs 51.0%, p=0.132). Although there was no difference in patient delay (240 [120-570] vs. 360 [120-600] minutes, p=0.940), an increase in system delay was found (49 [30-110.25] vs. 140 [90-180] minutes, p=0.019).
Regarding the clinical status at admission, the 2020 group exhibited a higher Killip-Kimball class, with a decrease in class I (74.5% vs. 51%) and an increase in class III (1.8% vs. 8.2%) and IV (5.5% vs. 18.4%) patients (p=0.038) (Figure 2). Additionally, there was a greater incidence of vasoactive support initiation (3.7% vs. 26.5%, p=0.001). Moreover, an increase in invasive mechanic ventilation usage (3.6% vs. 14.3%, p=0.056) was observed.
There were no differences regarding PPCI success, incidence of multivessel disease, need for non-culprit coronary intervention, ischemic or arrhythmic events after revascularization. Creatinine at admission and LVEF at hospital discharge also revealed no differences between the groups, but there was a significant increase in patients discharged with severe left ventricular dysfunction (3.6% vs. 16.3%, p=0.03).
Regarding mortality (see Figure 3), there was an increase in in-hospital mortality in the 2020 group (14.3%) compared with the 2019 group (7.3%) (p=0.200) with no significant changes in the circumstances or timing of the deaths.
DiscussionIn our hospital, we found no significant differences in STEMI incidence between March and April 2020 in comparison with the same period of 2019. However, we noted a clear increase in case severity, as reflected by multiple indicators, such as more severe Killip-Kimball class on admission, a much higher proportion of patients in need of mechanical ventilation and vasoactive support, an increase in the proportion of patients with severe left ventricle systolic dysfunction at discharge, and almost double the level of in-hospital mortality. Although no differences in patient delay were found, an increase in system delay was observed, associated with a decrease in pre-hospital emergency medical transportation and a non-significant increase in interhospital transfers. These data are particularly interesting in the light of a STEMI response system that was not saturated by an insurmountable increase in COVID-19 cases, reflecting the existence of other confounding factors.
Our results are in line with prior reports of increased time from symptoms to treatment and mortality, but do not support the global perception of a substantial reduction in STEMI admissions.4,12,13
The absence of data on non-ST elevation myocardial infarction (NSTEMI) and total emergency admission is a limitation of our work and do enable a global understanding of the impact of COVID-19 on the incidence of all myocardial infarction types in our center. Observational studies report an asymmetrical impact, with a sharper decrease in admissions of NSTEMI than STEMI.14,15 On the other hand, preliminary data from Portugal showed a considerable reduction in emergency admissions with a decrease in all triage categories.9
The role of SARS-CoV2 as a trigger should also be considered and could be a reason that contributes to a non-reduction of STEMI admissions. The association between the influenza infection and myocardial infarction is well established and the SARS-CoV2 infection has been also hypothesized as a STEMI trigger.16,17 Previous cardiovascular disease and cardiovascular injury in the context of COVID-19 is associated with a worse prognosis but the pathogenic mechanisms are still not totally understood.18–20 Our study cannot assess this relationship, as there were no cases of SARS-CoV2 infection in STEMI patients admitted to our center.
At the start of the COVID-19 pandemic, there was local reorganization in healthcare, which may have disturbed the established reference network of care and might be linked to an increase in treatment delays.
At our center, STEMI patients after PCI were admitted to a buffer area in the Cardiac Intensive Care Unit while the SARS-CoV-2 test result was still unknown. All the other aspects of the STEMI protocol remained unchanged.
The increase in attendance at non-PPCI centers and a decrease in pre-hospital emergency services are known determinants of an increase in system delay.10 Patient fear of COVID-19 might explain this change. A reduced awareness of other medical conditions among the population may have led to a reduction in emergency calls. The pre-hospital emergency medical transportation enables prompt diagnosis and non-PPCI centers to be bypassed, reducing the time to PCI and, consequently, fibrinolysis. Also, the increased awareness of COVID-19 among health care workers in the triage system may have resulted in STEMI patients being inadvertently directed to COVID-19 areas, thus delaying diagnosis and prompt care.
The adequate treatment of STEMI requires timely reperfusion and system delay is a significant factor associated with in-hospital mortality21 and worse late prognosis.22 Our results showing an increased system delay may partially justify the greater clinical severity of STEMI patients and the non-significant rise in in-hospital mortality. This may be an additional problem during a pandemic and a modifiable factor contributing to economic costs.23
Although we did not find an increase in patient delay, this could be due to a higher proportion of missing data in severe patients, including the case of fatalities, where patient delay was expected to be higher.
In Portugal, the COVID-19 outbreak did not saturate the national public health care system, however, it may have disrupted the regional MI referral network, which associated with the widespread fear of infection in hospitals, delayed prompt treatment of STEMI patients. There is evidence of a sharp decrease in ED admissions around the world that can also be justified by fear of infection.4
As it is likely that we will be managing patients with COVID-19 over the next 12-18 months, we also need to ensure that the cardiovascular population continues to benefit from streamlined STEMI care. Therefore, continuous high-quality cardiovascular care must be available for all patients. This includes educational content for patients, advising them not to overlook cardiovascular symptoms, and dedicated pathways for pre-hospital and in-hospital STEMI care. It is extremely important not to decrease the provision of health-care services to the population, in order to optimize STEMI treatment, improve patient prognosis and reduce the global costs of care.
ConclusionDuring the COVID-19 pandemic in the central region of Portugal, a relatively low-incidence region in the context of Western Europe, a similar rate was observed in the number of STEMI admissions. However, an increase in STEMI clinical severity was found and among those who survived, there was a higher proportion of patients with severe left ventricle systolic dysfunction at discharge. An increase in system delay and a decrease in prehospital care usage might explain these results, which should be the focus of attention for future action during a new pandemic lockdown.
FundingThis research was funded by the Portuguese Science Foundation grant RIGHT2H POCI-01-0145-FEDER-032414.
Conflicts of interestThe authors have no conflicts of interest to declare.