Left ventricular false tendon (LVFT) is a chord-like structure composed of fibrous, fibromuscular, or muscular tissue that traverses the left ventricular (LV) cavity in some cases. It is a continuation of the innermost layer of the myocardium in the left ventricle. The size and length of the LVFTs can vary among different individuals. They can be classified, based on their thickness, into three types, although their functional differences are not clear. The fibrous type, which is less than 1.4 mm in thickness, the fibromuscular type that ranges from 1.5 to 2.4 mm, and the muscular type, which is greater than 2.5 mm in thickness. Echocardiographic studies have indicated an event rate ranging from 18% to 26%, while autopsy studies have reported a rate of about 34%.1,2 In earlier reports, the incidence was found to be as high as 83% in the pediatric population.3 Furthermore, a collection of autopsies and surgeries revealed a slightly greater prevalence among males.1 False tendons are typically benign anatomical structures, but when they rupture, they can resemble some pathologies such as vegetations, thrombi or ruptured chordae tendineae. In addition, LVFTs can occasionally be associated with some ventricular arrhythmias, ventricular dilation, and impaired cardiac systolic and diastolic function.4
During some cardiac surgeries or left ventricular catheter ablation procedures, the operator needs to be mindful of the existence of LVFTs.1 In post myocardial infarction states, false tendons can become necrotic and may rupture at their ventricular attachment. A similar condition can also occur during heart failure, when significant left ventricular enlargement or spherical remodeling causes false tendon tension and finally separation from the left ventricular wall. Echocardiography is an available tool to diagnose LVFTs. In previous studies, preoperative echocardiography has shown a sensitivity of 82% and a specificity of 85% in diagnosing LVFTs.2
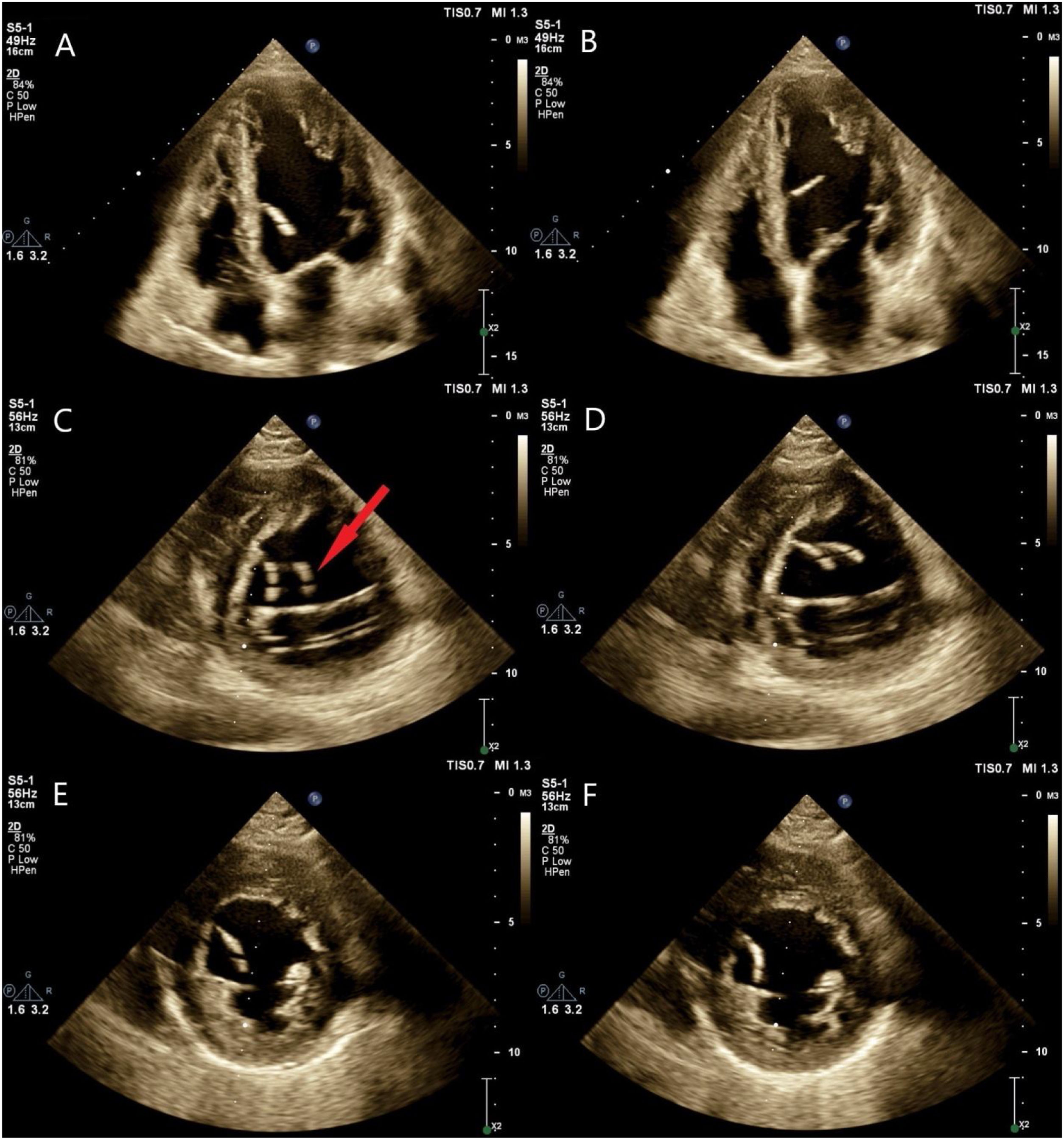
We present the case of a 63-year-old male patient who was referred to emergency department at our tertiary center with complaints of acute-on-chronic chest pain, which had intensified over four days. Following initial diagnosis of a neglected recent inferior posterior myocardial infarction, cardiac catheterization was performed, which revealed multiple coronary artery obstructions suitable for coronary artery bypass graft surgery (CABG). The transthoracic echocardiography performed as a part of preoperative evaluation revealed mild LV enlargement with severe systolic dysfunction (LV ejection fraction about 20%) as well as a hypermobile moderately echogenic strand-like structure within the LV cavity, measuring approximately 25 mm in length and about 2 mm in thickness, attached to the mid portion of the interventricular septum, suggestive of a ruptured false tendon. On the short axis view of the left ventricle, an interesting false image duplication was registered due to ultrasound beam refraction consistent with a “ghost artifact”, which was omitted by small angulation of the probe (Figure 1, Video 1). The patient underwent CABG, with no special measures for the ruptured false tendon.
(A and B) Apical four-chamber views of transthoracic echocardiography showing snapshots of a strand-like hypermobile structure within left ventricular (LV) cavity attached to the mid portion of the interventricular septum consistent with a ruptured fibromucular false tendon. (C and D) Parasternal short axis views of the same patient showing false duplication of the false tendon image due to refraction artifact (red arrow). (E and F) Omitting of the ghost artifact by small tilting of the probe so a little change in direction of ultrasound beam propagation.
The possible presence of echocardiographic artifacts is something important to be considered when interpreting echocardiographic images. These artifacts can lead to incorrect depiction of the true anatomy and so may result in some errors in diagnosis or measurement. One of these artifacts is the curiously named “ghost artifact”, which is produced when the refraction of ultrasound beam occurs in one part of the scanning plane due to its propagation through tissue interfaces with different propagation speeds. This can result in deceptive image duplication or even triplication.5
Conflicts of interestThe authors have no conflicts of interest to declare.