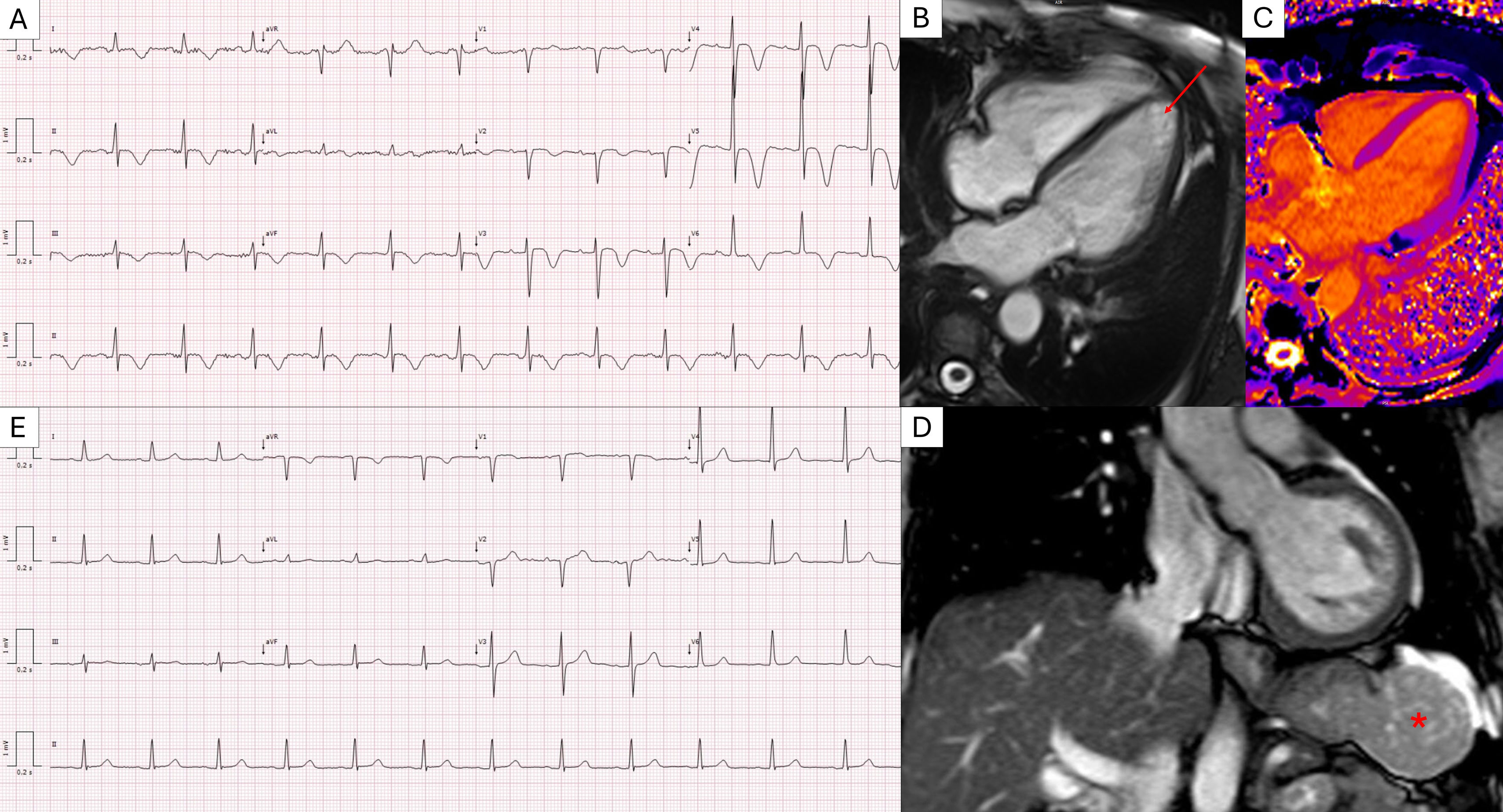
A 67-year-old female was referred to the cardiomyopathy clinic following an abnormal electrocardiogram (ECG) with the suspicion of apical hypertrophic cardiomyopathy. The ECG showed high-voltage R waves and deep, symmetrical T-wave inversions (Figure 1A). These findings emerged during evaluation for unexplained anorexia and significant weight loss. Her history included hypertension and dyslipidemia. Physical examination and family history were unremarkable.
(A) ECG showing high-voltage R waves and global symmetrical T-wave inversion. (B) Cardiac MRI cine b-SSFP four-chambers image showing non-thickened biventricular walls (e.g. interventricular septum of 7 mm) and no signs of apical hypertrophy (red arrow). Tissue characterization sequences including STIR T2-weighted imaging, native T1 mapping (C), and LGE were unremarkable, showing no evidence of myocardial edema, fibrosis, or infiltration. (D) Cardiac MRI coronal TRUFI image showing a round and relatively homogeneous solid lesion in the greater gastric curvature (red asterisk). (E) ECG at one-year follow-up demonstrating complete resolution of the previously observed R and T wave abnormalities.
Multimodal imaging, including transthoracic echocardiography, cardiac computed tomography (CT), and magnetic resonance imaging (MRI), revealed no structural heart disease, ventricular hypertrophy, or myocardial/pericardial inflammation (Figure 1B and C). A thoracoabdominal CT identified a 5.5 cm homogeneous contrast-enhanced lesion on the greater curvature of the stomach. A subsequent CT demonstrated rapid tumor growth in close anatomical proximity to the heart, without evidence of compression or displacement of cardiac structures. The mass showed defined demarcation from the surrounding tissues on MRI (Figure 1D). A CT-guided biopsy identified a gastrointestinal stromal tumor (GIST). Following subtotal gastrectomy, pathology confirmed a low-risk GIST with clear margins. Postoperative follow-up at six months revealed no residual disease, and serial ECGs over the following year demonstrated full normalization of prior abnormalities (Figure 1E).
We hypothesize that the preoperative ECG abnormalities were caused by the anatomical proximity of the large GIST to the heart, resulting in localized distortion of the cardiac electrical field and affecting surface ECG recordings. The absence of structural or functional cardiac abnormalities and the resolution of ECG changes following tumor resection support this hypothesis.
This case highlights the importance of considering extracardiac causes of abnormal ECG findings, particularly when multimodal imaging demonstrates a structurally and functionally normal heart.
FundingNone declared.
Conflicts of interestNothing to disclose.