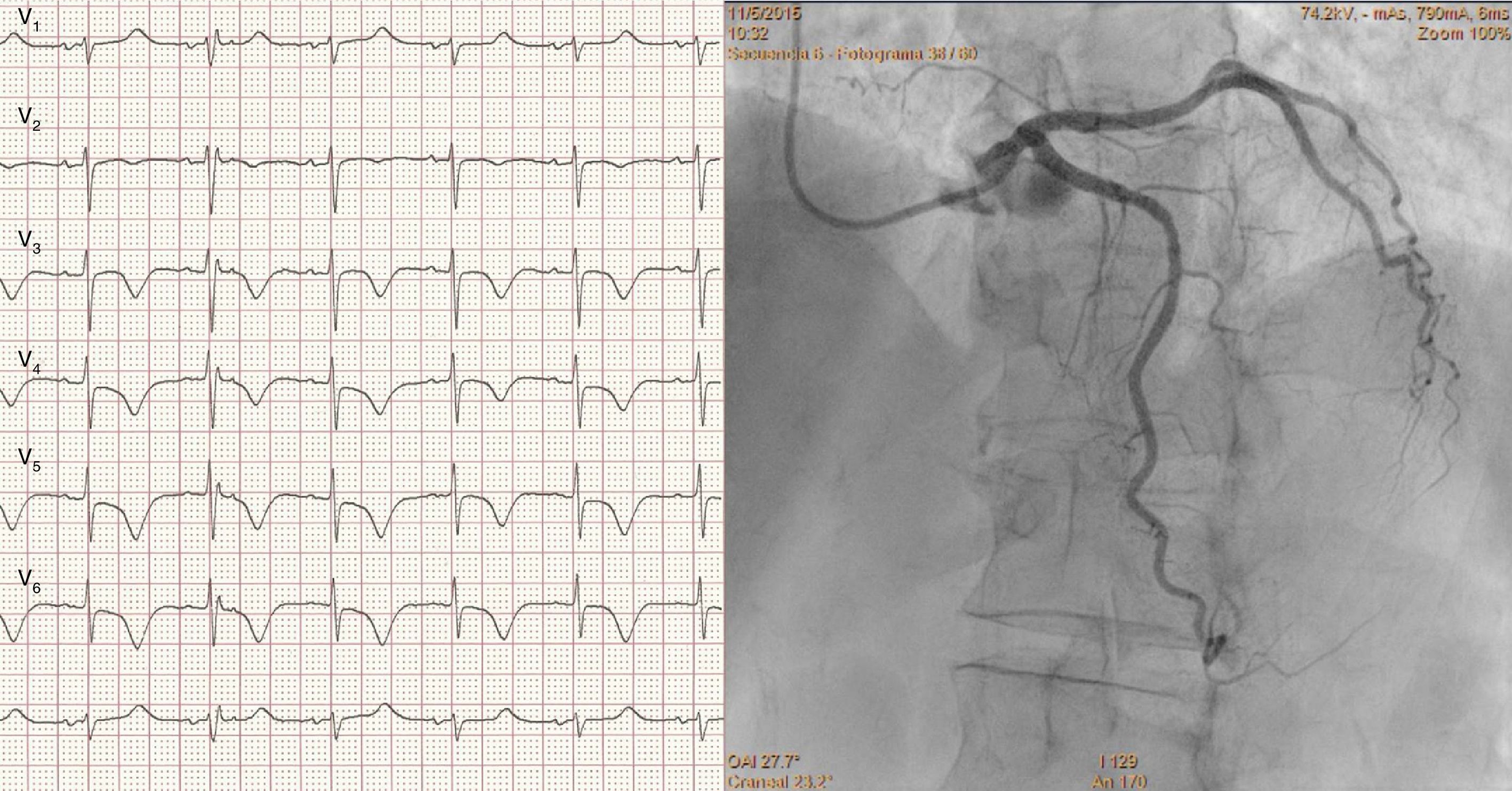
A 74-year-old woman presented with intermittent chest pain and dyspnea after emotional stress. The electrocardiogram showed sinus rhythm, deep and symmetric T-wave inversion in the anterior leads, and prolonged QT interval (corrected QT: 542 ms) (Figure 1, left). The echocardiogram revealed apical dyskinesia, so the patient was scheduled for early catheterization. Quantitative coronary angiography showed an intermediate tubular stenosis in the mid left anterior descending artery (Figure 1, right, and Supplementary Video), that was further functionally assessed by means of a pressure wire (PressureWire™ Guidewire, St. Jude Medical, Inc., St. Paul, MN).
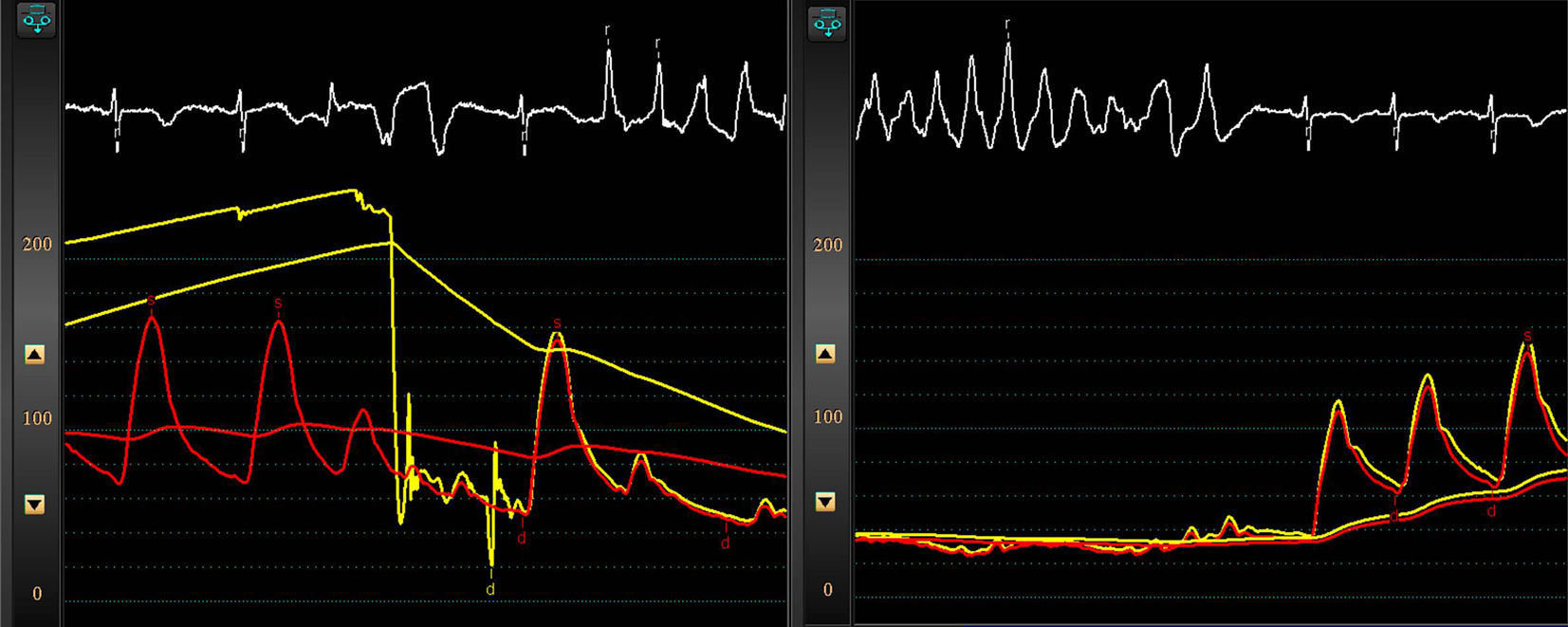
Baseline fractional flow reserve (FFR) was 0.97. An initial intracoronary adenosine injection of 120 μg triggered a presyncopal polymorphic ventricular tachycardia, self-limiting in 12 seconds (Figure 2). A second lower-dose injection of 60 μg was followed by another episode of non-sustained polymorphic VT. Then atropine 1 mg was administered intravenously, heart rate increased above 80 beats per minute, and further adenosine boluses (up to 240 μg) were well tolerated. Minimum FFR was 0.93, so intervention was safely deferred.
Left: afterdepolarizations and initiation of polymorphic ventricular tachycardia (VT) following adenosine injection. Note the absence of catheter damping or ischemia; right: self-termination of the VT, with restoration of blood pressure and minimal separation between pressure curves (Pd, red curve; Pa, yellow curve). Further adenosine injections demonstrated a minimum fractional flow reserve of 0.93 (non-significant).
Adenosine has largely replaced papaverine as the hyperemic agent of choice due to anecdotal evidence of ventricular arrhythmias with the latter. However, in patients with long QT interval adenosine may not be so safe, as it can promote triggered activity and precipitate ventricular tachycardia. A long QT interval is frequently seen in patients with stress cardiomyopathy. In these cases, premedication with atropine or determination of adenosine-free indices such as the instantaneous wave-free ratio can increase the safety of functional assessment of coronary stenosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.