The coronavirus disease 2019 (COVID-19) spread quickly around the world. Although mainly a respiratory illness, there is growing interest in non-respiratory manifestations, particularly cardiovascular ones. At our center, mobilization of cardiologists with intensive care training was needed. Our aim is to describe patients with severe COVID-19 admitted to a Portuguese intensive care unit (ICU), the cardiovascular impact of the disease and the experience of cardiologists working in a COVID-19 ICU.
MethodsData from adult patients with COVID-19 admitted to the ICU of Centro Hospitalar de Vila Nova de Gaia/Espinho between 16 March 2020 and 21 April 2020 were analyzed retrospectively.
ResultsThirty-five patients were admitted. Mean age was 62.6±6.0 years and 23 (65.7%) were male. Dyslipidemia was the most common cardiovascular risk factor (65.7%, n=23), followed by hypertension (57.1%, n=20). Mean ICU stay time was 15.9±10.0 days. Patients had high rates of mechanical ventilation (88.6%, n=31) and vasopressor support (88.6%, n=31). Low rates of new onset left systolic dysfunction were detected (8.5%, n=2). One patient required venoarterial extra-corporeal membrane oxygenation. Mortality was 25% (n=9). Acute myocardial injury and N-terminal pro-B-type natriuretic peptide (NT-proBNP) elevation was detected in 62.9% (n=22). Patients that died had higher NT-proBNP compared to those discharged alive (p<0.05). Care by cardiologists frequently changed decision making.
ConclusionsThe cardiovascular impact of COVID-19 seems relevant but is still widely unknown. Studies are needed to clarify the role of cardiac markers in COVID-19 prognosis. Multidisciplinary care most likely results in improved patient care.
A doença pelo novo coronavirus (COVID-19) espalhou-se rapidamente pelo globo. Embora tenha atingimento essencialmente respiratório, existe interesse nas manifestações extrarrespiratórias, nomeadamente nas cardiovasculares. No nosso centro, foi necessária a mobilização de cardiologistas com experiência em cuidados intensivos para enfrentar este desafio. O objetivo desta investigação é descrever a população internada com COVID-19 grave numa UCI portuguesa, o impacto cardiovascular desta doença e a nossa experiência enquanto cardiologistas numa UCI COVID-19.
MétodosDados de adultos com COVID-19 internados na UCI do Centro Hospitalar de Vila Nova de Gaia/Espinho entre 16/03/2020 e 21/04/2020 foram analisados retrospetivamente.
ResultadosForam internados 35 doentes. A média de idade foi 62,6±6,0 anos e 23 (65,7%) doentes eram homens. A dislipidemia foi o fator de risco cardiovascular mais prevalente (65,7%, n=23), seguida pela hipertensão (57,1%, n=20). O tempo médio de internamento em UCI foi 15,9±10,0 dias. A necessidade de ventilação mecânica (88,6%, n=31) e suporte vasopressor (88,6%, n=31) foi alta, mas poucos doentes desenvolveram disfunção sistólica de novo (n=2,85%). A mortalidade foi de 25% (n=9). Foi detetada lesão miocárdica aguda e elevação do NT-proBNP em 62,9% (n=22) dos doentes, sendo os níveis de NT-proBNP mais elevados nos doentes que faleceram (p<0,05). A participação de cardiologistas na UCI alterou frequentemente a decisão clínica.
ConclusãoO impacto cardiovascular da COVID-19 parece relevante mas é parcamente conhecido, sendo necessários mais estudos para clarificar o papel dos marcadores cardíacos no prognóstico da COVID-19. As equipas multidisciplinares provavelmente melhoram os cuidados de saúde prestados a estes doentes.
On 31 December 2019, the Wuhan Health Commission reported a cluster of atypical pneumonia cases in the city of Wuhan, China.1 These were later known to be caused by a novel coronavirus, which became known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the disease, named coronavirus disease 2019 (COVID-19), spread quickly around the world, causing a pandemic with over three million cases and 200 000 deaths worldwide, at the time of writing.2 This disease is mainly characterized by a respiratory illness of varying severity, ranging from asymptomatic or mildly symptomatic patients to severe respiratory failure, acute respiratory distress syndrome and multi-organ failure.
Multiple risk factors have been suggested for the development of severe COVID-19. Conventional cardiovascular risk factors, such as hypertension, and established cardiovascular disease (such as coronary artery disease (CAD) and chronic heart failure), appear to be associated with more severe disease at presentation and higher mortality.3 A potential harmful role for the anti-hypertensive drugs angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor 2 blockers (ARB) has also been suggested, although recent evidence brings this into question.4,5 Thus, the relationship between both cardiovascular disease (CVD) and risk factors and COVID-19 is still poorly understood.
Lately, there has been a growing interest in the non-respiratory manifestations of the disease. Namely, cardiovascular ones, from apparently isolated acute myocardial injury to frank cardiomyopathy and cardiogenic shock, seem relevant and have been associated with poorer outcomes,6 with some patients requiring high-dose vasopressor and inotropic support and even mechanical circulatory support with venoarterial extra-corporeal membrane oxygenation (VA-ECMO).7 However, discrepant observations regarding the prevalence and impact of these manifestations have been made across cohorts from different countries and regions,8 suggesting distinct disease presentations across different populations, while highlighting the need for local studies to hone local clinical practice. In Portugal, studies on the characteristics of local patients affected by COVID-19 are lacking and, to our knowledge, analyses focusing on the cardiovascular aspects of the disease in the local population have yet to be published.
In Portugal, COVID-19 has also taken its toll, with almost 29 000 cases and over 1000 deaths due to the disease.9 As such, a high health care worker mobilization occurred, in light of the increased strain and burden placed on the national health system. At our center, a total of six cardiologists or cardiology residents with varying degrees of training in intensive care volunteered to help in the hospital's COVID-19 dedicated intensive care unit (ICU), in an attempt to aid patients and colleagues alike.
With this study we aim to: describe the patients admitted to a Portuguese ICU with severe COVID-19, their CVD and risk status; determine the impact of the severe form of the disease on the cardiovascular system; and report the experience of this center's cardiologists delivering care to these patients.
MethodsData from adult patients admitted to the general ICU of our center (Centro Hospitalar de Vila Nova de Gaia/Espinho, Portugal) between the 16 March 2020 and 21 April 2020 was retrospectively analyzed. Only patients with atypical pneumonia caused by SARS-CoV-2 were included. Patients with confirmed COVID-19 without evidence of respiratory disease that still needed intensive care for other reasons were excluded from analysis.
We defined acute myocardial injury as one measurement of cardiac troponin above the 99th percentile upper reference limit, together with a rise/fall of troponin values, as per the Fourth Universal Definition of Myocardial Infarction;10 left ventricular systolic dysfunction as a left ventricular ejection fraction under 50%; hypertension as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or being on anti-hypertensive medication; diabetes as fasting plasma glucose ≥7.0 mmol/L (≥126 mg/dL), HbA1c ≥48 mmol/mol (≥6.5%), two-hour post-load plasmatic glucose ≥11.1 mmol/L (≥200 mg/dL) during an oral glucose tolerance test, or being under treatment with a hypoglycemic drug; dyslipidemia as low-density lipoprotein ≥4.14 mmol/L (≥160 mg/dL), high density lipoprotein <1.03 mmol/L (<40 mg/dL), triglyceride ≥2.26 mmol/L (≥200 mg/dL), or being under anti-dyslipidemic medication; heart failure (HF) as the presence of typical symptoms and/or signs accompanied by a structural or functional cardiac abnormality leading to reduced cardiac output and/or elevated cardiac pressures at rest or during stress; and chronic kidney disease as an abnormality in kidney structure or function present for >3 months.
All the categorical variables were described using frequencies and percentages, and the continuous variables were presented using means and standard deviations or medians. Troponin T and N-terminal pro brain natriuretic peptide (NT-proBNP) values were compared between those discharged alive and those that died during their hospital stay using independent sample T-tests. Patients with known HF and high ambulatory NT-proBNP were excluded from analysis. NT-proBNP was measured by electrochemiluminescence using the Elecsys proBNP II kit (Roche, Basel, Switzerland).
Data was collected using the built-in data extracting tool in the medical software used in daily medical practice at the ICU (B-ICU.Care, B-Simple, Oporto). Statistical significance was set at a p <0.05. Statistical analysis was performed with the Statistical Package for the Social Sciences software, version 20.0 (IBM, Armonk, New York, USA).
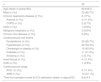
ResultsOne patient was excluded from analysis (complete heart block with cardiogenic shock and positive nasopharyngeal swab for SARS-CoV-2 with no evidence of pneumonia). Table 1 shows the characteristics of the population. A total of 35 patients were admitted in the mentioned time frame. The total capacity of the ICU was 20 beds for most of this period. Mean age at admission was 62.6±6.0 years and 23 (65.7%) patients were male. Dyslipidemia was the most common cardiovascular risk factor (65.7%, n=23), followed by hypertension (57.1%, n=20). Fifteen (42.9%) patients were obese or overweight and 11 (31.4%) had diabetes. Four patients (11.4%) had previously known HF and only one (2.9%) patient had known CAD. Only two patients (5.7%) had chronic pulmonary disease. Four patients (11.4%) were under treatment with ACE inhibitors and 13 (37.1%) with ARBs with a total of 17 patients (48.6%) with either drug.
Description of clinical characteristics of patients admitted to the intensive care unit.
| n | 35 |
|---|---|
| Age (mean in years±SD) | 62.6±6.0 |
| Male (n (%)) | 23 (65.7%) |
| Chronic respiratory disease (n (%)) | 6 (17%) |
| Asthma (n (%)) | 4 (11.4%) |
| COPD (n (%)) | 2 (5.7%) |
| CKD (n (%)) | 1 (2.9%) |
| Malignant neoplasia (n (%)) | 3 (8.6%) |
| Chronic liver disease (n (%)) | 0 (0%) |
| Cardiovascular risk factors | |
| Dyslipidemia (n (%)) | 23 (65.7%) |
| Hypertension (n (%)) | 20 (54.3%) |
| Overweight or obesity (n (%)) | 15 (42.9%) |
| Diabetes (n (%)) | 11 (31.4%) |
| Smoking (n (%)) | 2 (5.7%) |
| Heart failure (n (%)) | 4 (11.4%) |
| CAD (n (%)) | 1 (2.9%) |
| Cardiovascular drugs | |
| ACE-I (n (%)) | 4 (11.4%) |
| ARB (n (%)) | 13 (37.1%) |
| Time from symptom onset to ICU admission (mean in days±SD) | 9.6±4.4 |
ACE: angiotensin converting enzyme; ARB: angiotensin receptor 2 blocker; CAD: coronary artery disease; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; ICU: intensive care unit; SD: standard deviation.
Mean time from symptom onset to ICU admission was 9.6±4.4 days. Mean ICU stay time was 15.9±10.0 days. Table 2 shows outcomes and treatments received by patients during their ICU stay. Patients showed high rates of mechanical ventilation (88.6%, n=31) and vasopressor support with norepinephrine (88.6%, n=31). Low rates of direct cardiac compromise were detected, with only 8.5% (n=2) showing new onset left ventricular systolic dysfunction. Both patients received initial inotropic support with dobutamine and subsequently with levosimendan, with one of them requiring mechanical circulatory support with VA-ECMO. All patients received treatment with hydroxicloroquine. No complex ventricular dysrhythmias were noted. Mortality in the ICU was 25% (n=9). All the patients successfully discharged from the ICU were alive at the time of writing.
Treatments, outcomes, and complications during intensive care unit stay.
| Treatment with hydroxichloroquine | 35 (100%) |
| Need for invasive mechanical ventilation (n (%)) | 31 (88.6%) |
| Need for vasopressor support (norepinephrine) (n (%)) | 31 (88.6%) |
| Need for inotropic support (dobutamine and levosimendan) (n (%)) | 2 (5.7%) |
| Need for mechanical circulatory support with VA-ECMO (n (%)) | 1 (2.9%) |
| Acute myocardial injury (n (%)) | 24 (62.9%) |
| Ventricular arrhythmias | 0 (0%) |
| Cardiogenic shock (n (%)) | 2 (5.7%) |
VA-ECMO: veno-arterial extra-corporeal membrane oxygenation.
Acute myocardial injury was detected in 62.9% (n=22), with a median troponin T value of 112.0ng/L. NT-proBNP was also elevated in 62.9% (n=22) patients, with a median value of 1946.5pg/mL. The median values of both troponin T and NT-proBNP were higher in patients that died compared with those who were discharged alive from the ICU (115.0 ng/L vs. 37.5ng/L for troponin T; 6184.0 pg/mL vs. 622.5 pg/mL for NT-proBNP); however, this difference only reached statistical significance for NT-proBNP (p<0.05).
DiscussionThis was a retrospective analysis of the experience of a team of cardiologists working in a COVID-19 dedicated ICU, aimed at describing the affected population, the cardiovascular implications of the disease and their personal experience.
We noted a high prevalence of cardiovascular risk factors in our population. This is in stark comparison to the lower rates observed for pulmonary disease. Although surprising at first glance, these results bear a close resemblance to descriptions from most sites, in particular, Italy,11 New York City8 and China.7 However, lower rates of cardiovascular comorbidities were reported in China, in contrast to what we and other investigators from Italy and New York City observed, especially regarding hypertension. Differences in ethnic and cultural background between western and eastern countries could explain these findings.
We also noticed a significant rate of patients under ACE inhibitors or ARBs. Even though initial reports have suggested that the use of these drugs could lead to worse outcomes,12 expert consensus and guidelines were reluctant to go by these first reports. Of note, one recent, large, observational study with 12 594 patients points to no relationship between these drugs and mortality.4 Even though our sample is too small to draw conclusions regarding outcomes, the high rate of ACE inhibitors and ARBs in our population could be a coincidence, as it can be explained by the significant number of hypertensive patients, with either drug being prescribed in 85% of hypertensive patients. All included patients were treated with hydroxicloroquine for at least 10 days. The treatment regimen consisted of 400 mg once on the first day and 200 mg twice daily thereafter. Although one of the main concerns with the use of this drug is the development of acquired long-QT syndrome and polymorphic ventricular tachycardia, we did not witness this complication, which might be explained by the small sample size and tight control of other QT prolonging factors. Also, the QT interval was only monitored with three-lead telemetry recording, which may not be as sensitive as a 12-lead electrocardiogram for long-QT syndrome. Additionally, the prescription and use of hydroxicloroquine in this setting was highly controversial during the study timeframe, both inside the scientific community and the local medical staff; in fact, in light of recent evidence,13 the use of hydroxicloroquine is no longer encouraged and this drug is no longer in use for the treatment of COVID-19 at our center.
Our patients showed high requirement for invasive mechanical ventilation and vasopressor support. Although the criteria for invasive mechanical ventilation in these patients has been under question, the need for vasopressor support observed in mechanically ventilated patients is in line with various reports from different regions.8,14,15 Only two patients developed cardiogenic shock, with one warranting support with VA-ECMO. Although not present in a relevant number, the impact on the outcome that the development of severe cardiogenic shock can have warrants our attention. Moreover, as cardiologists, we developed particular interest in these patients. Even though SARS-CoV-2 myocarditis is a cause of cardiogenic shock in these patients,16 we made the putative diagnosis of Takotsubo syndrome in these patients, since both presented with discrepant troponin and NT-proBNP values, typical left ventricle segmental contractile abnormalities consistent with the diagnosis and quick recovery of left ventricular systolic function. Additionally, this complication has been reported by other studies, including in critically ill patients.17,18 Both patients were successfully weaned from mechanical and pharmacologic hemodynamic support and were discharged alive from the ICU.
Although data regarding the frequency of acute myocardial injury in COVID-19 patients are sparse, our findings suggest abnormally high rates when compared with other reports currently available.19,20 However, these reports refer to COVID-19 patients requiring hospitalization but not exclusively intensive care, which may explain the registered differences. To our knowledge, this is the first report describing the rate of acute myocardial injury in ICU-treated COVID-19 patients. The NT-proBNP values recorded were also significantly higher than previous reports,20 the pitfall of which is the same as described above for acute myocardial injury. Higher NT-proBNP values also correlated with higher mortality, which may indicate a potential marker for worse prognosis. However, this finding must be interpreted with caution: on the one hand, both patients who developed the most severe cardiac complications and had some the highest absolute NT-proBNP values were both discharged alive from the ICU, and were still alive at the time of writing; on the other hand, three patients with known previous CVD (one with severe aortic valve stenosis, one with three-vessel coronary artery disease and severely depressed left ventricular ejection fraction and one with recent pacemaker lead endocarditis and four surgical cardiac interventions) also presented with very high absolute NT-proBNP and all died. These findings highlight that prognostic markers may aid in clinical decision but require integration with other medically relevant information and clinical evaluation. The intricate connection between COVID-19 and the cardiovascular system is still under investigation and warrants further studies to shed more light on this matter.
Finally, as cardiologists, working alongside our colleagues at the ICU during the COVID-19 pandemic was a challenging but rewarding experience. The region to which our hospital provides care (Vila Nova de Gaia) had the second highest number of confirmed COVID-19 cases in Portugal, and some of the municipalities with the highest infection per inhabitant ratio.9 We felt the need to provide care to both patients and colleagues and, as such, gladly volunteered. The finding of high rates of acute myocardial injury and elevated NT-proBNP, together with the known diagnostic difficulty of cardiac events in ICU patients with respiratory disease, opened the door for an important role for our team in this collaboration. We were able to improve patient management by providing differentiated cardiovascular care, by giving every admitted patient at least one (and sometimes multiple) ultrasound evaluation, with assessment of left and right ventricular systolic function, echocardiographic significance of acute myocardial injury, valve dysfunction, volume status and lung ultrasound status, which frequently led to a change in clinical decision making. Also, we played an important role in the decision to use cardiac drug therapy but also mechanical support. However, the benefit certainly went both ways: forced out of our comfort zone, we harnessed experience in general patient care of critical patients, learned multiple intensive care procedures and honed some forgotten skills, which certainly will aid us in our care-giving at the cardiac intensive care unit.
ConclusionsIn conclusion, the relationship between SARS-CoV-2 and the cardiovascular system seems relevant but is still widely unknown. More studies are needed to clarify the role of cardiac markers in the prognosis of COVID-19 pneumonia-stricken patients. Collaboration and multidisciplinary care will most likely result in improved patient care.
Ethical approvalAll procedures performed in this study involving human participants were in accordance with the ethical standards of the university and/or national research committee and also with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Grant supportNo grant support to declare.
FundingNo funding to declare.
Informed consentFor this type of study formal consent is not required.
Conflicts of interestThe authors have no conflicts of interest to declare.