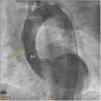
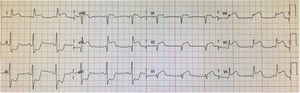
A 75-year-old obese woman with dyslipidemia and hypertension was admitted for acute chest pain. She presented anterolateral ST-segment elevation (Figure 1) and slightly elevated troponin levels. She was transferred to a percutaneous coronary intervention-capable centre.
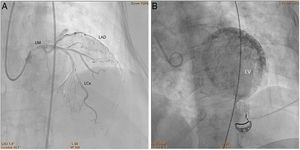
On admission, she presented with cardiogenic shock. Cardiac catheterization showed a dubious image of left main coronary artery dissection, without atherosclerotic lesions. An extremely slow flow in the left anterior descending and left circumflex arteries was noted (Figure 2A, Clip 1A), concomitant with contrast retention in the myocardial microcirculation (Figure 2B, Clip 1B).
A/Clip 1A. Cardiac catheterization. Left heart catheterization showing slow flow in the left main coronary artery and its branches. B/Clip 1B. Cardiac catheterization. Left heart catheterization showing myocardial microcirculation contrast retention. LAD: left anterior descending coronary artery; LCx: left circumflex coronary artery; LM: left main coronary artery; LV: left ventricle.
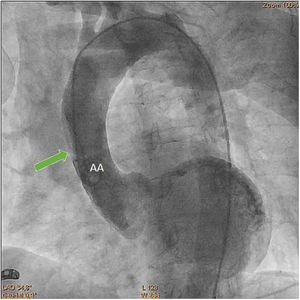
Aortography revealed a subtraction image compatible with an intimal flap in the ascending aorta (AA) (Figure 3, Clip 2), suggestive of aortic dissection (AD). The transthoracic echocardiogram revealed moderate left ventricular systolic dysfunction with anterior wall and apex hypokinesia, with no valvular changes.
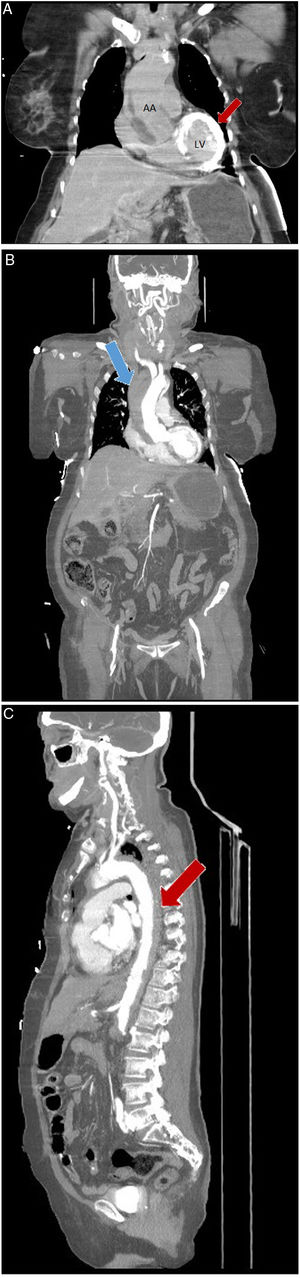
Computed tomography showed myocardial contrast retention in the left ventricle wall (Figure 4A). An aneurysmal dilatation of the AA with associated intramural hematoma and an intimal flap extending distally were noted, compatible with Stanford type A AD (Figure 4B and C). She suffered a cardiac arrest with pulseless electrical activity, recovered after 12 minutes of advanced life support, and was transferred to a cardiothoracic surgery centre. On admission to this center, she presented echocardiographic signs of retrograde dissection, with aortic regurgitation, and no clinical conditions for performing surgery. The patient died a few hours later.
(A) Coronal computed tomography. Non-contrast-enhanced coronal computed tomography showing myocardial contrast retention in the left ventricle wall (red arrow). (B) Coronal computed tomography. Contrast-enhanced coronal computed tomography showing intramural hematoma in ascending aorta (blue arrow). (C). Axial computed tomography. Contrast-enhanced axial computed tomography showing intramural hematoma in descending aorta (red arrow). AA: ascending aorta; LV: left ventricle.
This case portrays a poorly known phenomenon of myocardial contrast retention that should alert clinicians to a possible coronary artery involvement in the context of acute aortic syndrome.
Conflicts of interestThe authors have no conflicts of interest to declare.