Hypertrophic cardiomyopathy (HCM) remains a leading cause of sudden cardiac death (SCD) in young athletes and the classic decision regarding sports eligibility is the disqualification from competitive sport. The 2020 European Society of Cardiology (ESC) guidelines on sports cardiology and exercise in patients with cardiovascular disease are more liberal, emphasizing the multiple benefits of regular exercise and the shared decision making process.1
Recent studies have shown a lower risk of SCD and exercise-induced implantable cardioverter defibrillator shocks in individuals with HCM than previously described.2 Pelliccia et al.3 showed that over a nine-year follow-up in athletes with HCM who continued competitive sports, there were no significant differences in the incidence of symptoms or major clinical events compared to athletes who ceased exercise. Patients with HCM who engaged in exercise programs saw a significant improvement in functional capacity, while other research has demonstrated that the majority of SCD cases occur at rest.4 Although this evidence is promising, due to the heterogenicity and broad spectrum of HCM risk, the generalization of this message is simplistic and may lead to a wrong interpretation, leading to potential prognostic implications.
In fact, several issues should be clarified in the relationship between HCM and exercise. SCD can occur in the absence of major risk factors; athletes participating in high endurance or extreme sports are exposed to conditions that cannot be reproduced in preparticipation evaluation and ESC-risk score have never been validated in athletes. On the other hand, a detailed analysis of ESC guidelines, shows that recommendations for exercise in HCM have low class (IIb) and level of evidence (C) for high-intensity exercise/competitive sports in the absence of any markers of increased risk; low-moderate-intensity recreational exercise for individuals who have any marker and competitive sports for gene positiv/phenotype negative cases. In this context, shared decision-making is broadly advocated, combining the patients’ principles, preferences and autonomy, but must not be oversimplified as a process in which only the athlete decides.5
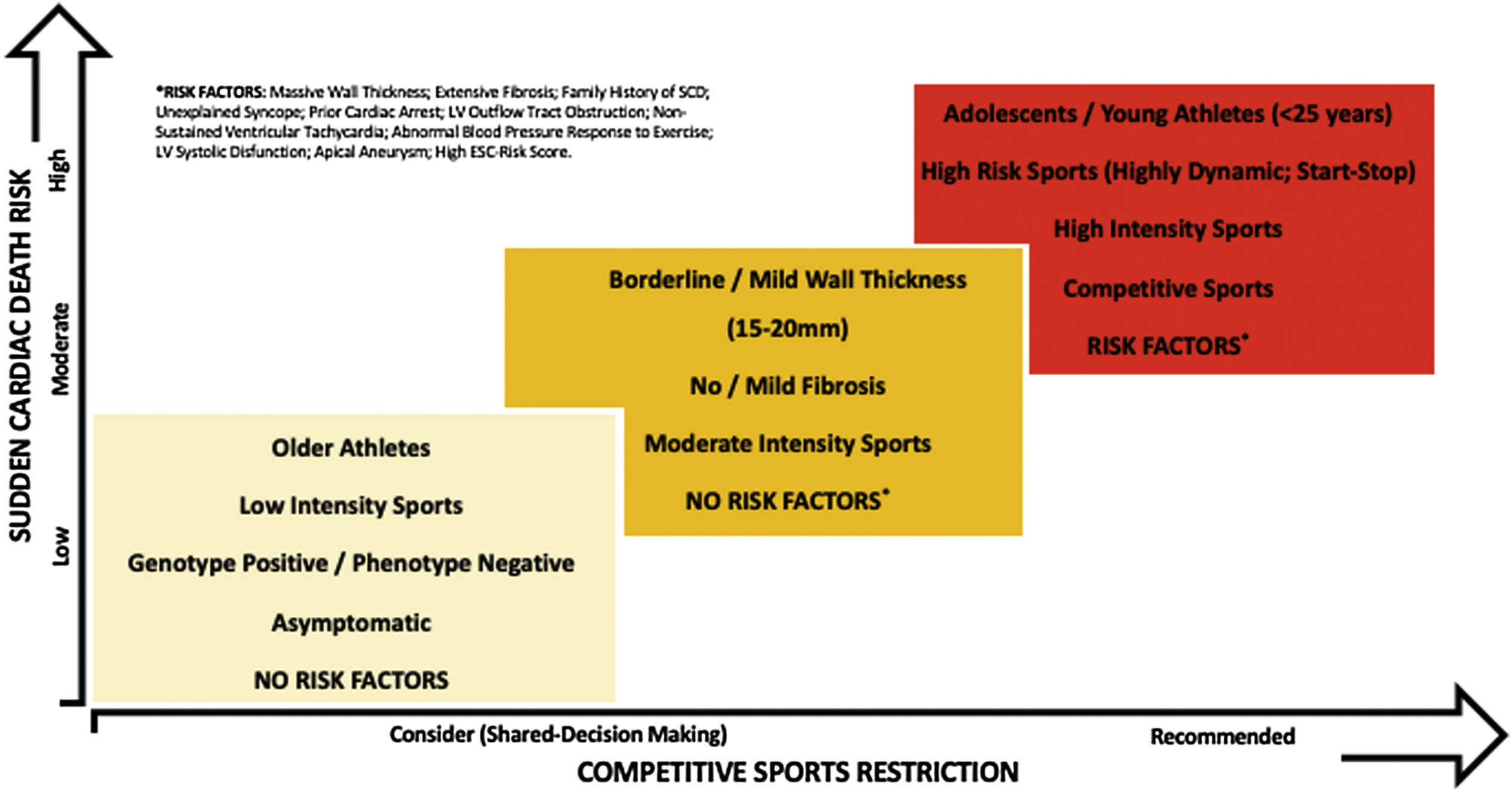
After diagnosis, risk stratification is essential to establish more accurate recommendations regarding sports eligibility and exercise prescription in HCM. Major risk factors are common to all HCM patients: prior cardiac arrest, unexplained syncope, family history of SCD, high ESC-risk score, left ventricular (LV) outflow tract obstruction, massive ventricular wall thickness, non-sustained ventricular tachycardia, extensive myocardial fibrosis, abnormal blood pressure response to exercise, LV systolic disfunction or apical aneurysm.6 The athlete's age and its impact on SCD risk (mean age 18 years) is very important, while specific disciplines such as highly dynamic and start-stop sports are associated with increased risk. Individuals with positive genotype and negative phenotype may engage in all sports, but a regular follow-up is recommended, mainly in adolescents/young adults.5
Individuals with HCM have different vulnerability to exercise-induced fatal arrhythmias and systematic restriction may be unjustified. However, the evidence is scarce to define the risk of SCD across all athletes and to investigate the safety of exercise in HCM, making eligibility decisions challenging, particularly in young competitive athletes. In this setting, a comprehensive approach is needed, focusing on individualized risk stratification and exercise prescription (Figure 1).5
The main issue is not whether exercise is possible in HCM, but which athletes can exercise, and which exercise is recommended. The goal should not be to establish the same recommendation for all patients but choose the right recommendation for each individual patient. Additional research is needed to determine the safety of sports in patients with HCM and develop evidence-based SCD risk stratification methods in this population. Until then, as in other areas of sports cardiology, it is essential to balance the benefits and risks of exercise.
Conflicts of interestThe author has no conflicts of interest to declare.