Understanding human behavior remains challenging, particularly in the context of health behavior changes. Progress in this area represents a significant contribution toward reducing the morbidity and mortality of non-communicable diseases. Cardiovascular disease (CVD) is the leading cause of mortality globally, and it is uncontentious that the main risk factors are modifiable and primarily behavioral: smoking, hypertension, dyslipidemia, unhealthy diet, and physical inactivity.1,2 Implementing measures to improve the prevention of CVD should be a real priority, from primordial to quaternary levels of prevention.
At the beginning of the 21st century, the field of behavioral cardiology emerged, the concept of cardiovascular (CV) health was introduced, and efforts began to optimize healthcare delivery systems with a focus on promoting health behaviors.
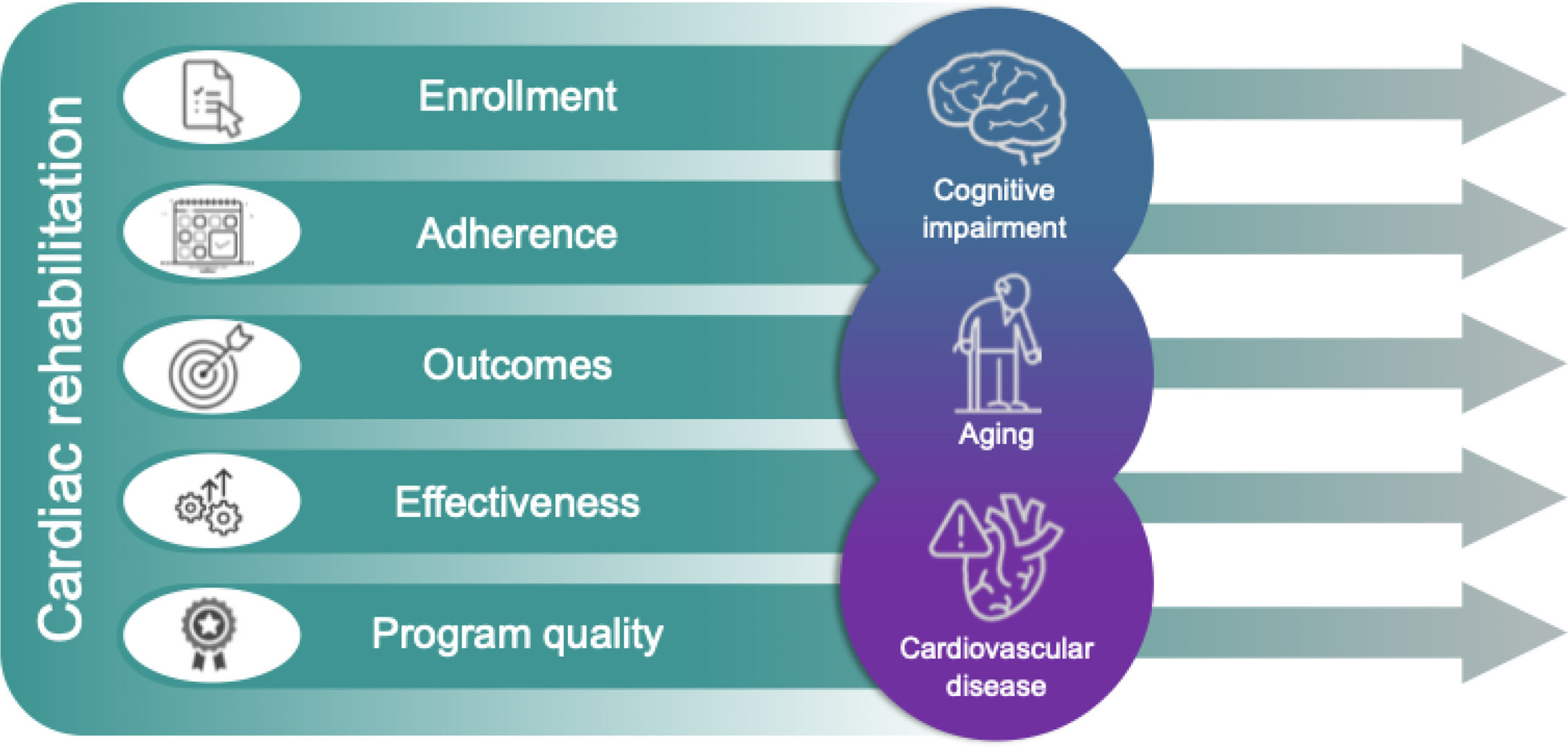
Cardiac rehabilitation (CR) is a multidisciplinary intervention that includes individually prescribed and monitored exercise training, education, and counseling for behavior change.1,3,4 With a Class I, Level A recommendation for various CV conditions, including myocardial infarction and heart failure, CR addresses the physical, psychological, and behavioral aspects of CVD recovery.1,3,4 CR typically progresses in phases, starting during hospitalization (phase 1), moving to center-based programs (phase 2) with secondary prevention interventions, and culminating in a phase of autonomy (phase 3, maintenance).3–5 Phase 2 requires the greatest investment from healthcare institutions, demanding dedicated physical infrastructure, equipment, and skilled human resources from various professional disciplines.3 Unfortunately, due to several barriers, these programs remain under-prescribed, with low enrollment rates and poor adherence.1,3,4,6 These are key concerns for the European Society of Cardiology/European Association of Preventive Cardiology (ESC/EAPC) that have highlighted the importance of standardized CR programs to improve quality and outcomes.3 The ESC/EAPC's accreditation framework emphasizes performance measures such as enrollment and adherence, advocating the integration of tailored interventions to address patient-level barriers.3 Similarly, the latest update of CR programs core components by the American Heart Association/American Association of Cardiovascular and Pulmonary Rehabilitation (AHA/AACPR) prioritizes addressing the challenges of enrollment and adherence, and introduces ‘program quality’ as a new component to evaluate performance at a program level.1
Uptake, enrollment, participation, compliance, adherence, and engagement are terms with distinct meanings, although they are often used interchangeably in the medical field. Consistent with most current literature, we define ‘enrollment’ as participation post-referral to CR and ‘adherence’ as active involvement in the program, including compliance with pharmacological treatments and engagement in lifestyle changes.1,3,6
Low enrollment and non-adherence are primarily influenced by psychosocial factors, particularly those related to aging.6 Depression and anxiety have been the focus of mental health assessments in CR programs, as depression has a profoundly negative impact on CV health and affects a significant portion of patients following acute myocardial infarction and those with heart failure.1,4 Of note, the ESC/EAPC and the AHA/AACPR rightly emphasize depression improvement as a key quality indicator for CR programs.1,3 However, other psychosocial factors, such as misconceptions about illness and treatments, low motivation for behavior change, social isolation, low educational level, unemployment, or poor economic status, should also be considered when assessing determinants of CR enrollment and adherence.6 Interestingly, psychosocial factors also play a crucial role in seeking treatment in acute coronary events, during which pain intensity does not affect the promptness with which a person seeks treatment. In this setting, for instance, anxiety and illness-related knowledge are influential in the speed of seeking help. Indeed, in CVD overall, health beliefs significantly impact health behaviors, especially healthcare-seeking behavior. Interestingly, older patients who considered their recent acute myocardial infarction or stroke to be an inevitable coincidence of ‘old age’ made fewer lifestyle changes in the following three years but were more willing to consult health professionals or be hospitalized.7 In fact, questions related to old age as a main determinant of low enrollment and non-adherence do not end here. In this context, cognitive function may act as a relevant mediator.
The link between cardiac diseases and brain health, particularly between CVD and cognitive impairment, is increasingly recognized. Robust evidence was highlighted by an AHA Scientific Statement dated October 2024, with a special focus on vascular, behavioral, and social factors.2 Undoubtedly a concern in aging populations such as ours,8 clinically significant cognitive impairment may play a crucial role in CR as we assume that trends toward healthier behaviors greatly rely on cognitive integrity. Cognitive function throughout life may evolve with the occurrence of benign senescence forgetfulness and subjective memory complaints, often in the context of mild depression and anxiety symptoms. Pathological cognitive impairment, whose etiology may include CVD, can manifest as mild cognitive impairment (MCI), where the patient's autonomy is overall maintained, or as dementia, with varying levels of disability. CV risk factors, such as age, hypertension, dyslipidemia, smoking, and diabetes, are also common in patients with MCI and dementia.2 Additionally, older individuals with vascular cognitive impairment have a higher prevalence of traditional CV risk factors.2 Therefore, it is not surprising that up to 50% of patients on CR have some form of cognitive impairment.9 Still, current protocols largely neglect formal cognitive testing at the time of admission.1,3–5 MCI, and even mild dementia, may go undetected, sometimes by experienced medical doctors or staff who are not necessarily familiar with these highly prevalent conditions. In fact, memory disfunction is not invariably present, despite major executive disfunction, for instance. Moreover, current estimates of mild dementia in Portugal are a matter of concern.8 Typically, patient evaluations at the time of CR admission are conducted by cardiologists, who may be unfamiliar with cognitive testing. Even among psychiatrists and neurologists, approaches to cognitive assessment can vary significantly. Regardless of the setting, brief valid and reliable tools, such as the Montreal Cognitive Assessment, may prove useful in practice.2,9
In summary, promoting health behavior change becomes even more challenging when cognitive impairment is involved. The complex interplay and overlap between aging, CVD, and cognitive impairment is illustrated in Figure 1, along with its potential impact on CR processes and outcomes. Cognitive impairment may even surpass depression in prevalence among CR participants, possibly having a greater effect on the key goals of current programs (e.g., adherence to treatments, learning about disease management and healthy lifestyles, behavior change maintenance). Cognitive impairment may impede self-management, hinder lifestyle changes, and result in missed healthcare appointments, all of which contribute to poor CR adherence and effectiveness. Nonetheless, patients >60 who adhere to CR programs demonstrate benefits in quality-of-life indexes comparable to those of younger adults.10
Further research is needed, particularly in Portugal, on CR enrollment and adherence and its determinants. The same applies to the prevalence of cognitive impairment among participants and consequences for adherence and outcomes. Just as exercise prescriptions must be tailored to cardiac status, we should probably assume that person-centered interventions in CR programs ought to be adjusted to cognitive status. Unfortunately, systematic cognitive assessment is not part of current protocols,1,3–5 with a probable toll on adherence.
Multimodal CR programs require substantial healthcare investment and involve professionals from cardiology, rehabilitation medicine, psychiatry, psychology, physiotherapy, nutrition, and nursing. Non-adherence, regardless of its cause, threatens cost-effectiveness, while identifying cognitive impairment at admission is feasible. This could help in tailoring more appropriate interventions and optimizing cost-effectiveness through improved enrollment and adherence, thereby generating benefits for all parties-patients, families, and healthcare teams. In short, there are well-founded reasons for a call to action.
Conflicts of interestThe authors have no conflicts of interest to declare.