Cardiac catheterization laboratories (cath labs) are commonly designed to achieve the best clinical outcomes while being efficient. This study develops methods to support healthcare managers in analyzing the added value of improvement measures, following a value-based healthcare (VBHC) framework.
MethodsBased on a sociotechnical approach, the applied methods aimed to increase efficiency, reduce duplication of tasks, cut costs, and improve patient care, while creating a more inclusive and trusting decision making process. Within the process of building a multicriteria evaluation model, meetings, interviews, and a decision conference were designed. In parallel, a workflow discrete event simulation model was built to replicate current patient flow and activities and to reproduce the impact of implementing improvement measures and variations in human resources.
ResultsFour evaluation criteria were considered for workflow improvement: contribution to the efficiency of the admission process, compliance with schedules, agility among procedures, and human resources training. The designed improvement measures sought to 1) improve the start-up of the day, 2) improve pre-exam assessment, and 3) improve staff training. Results prioritize ‘Measure 2’ and demonstrate that improving human resources allocation increases efficiency and offers significant cost savings.
ConclusionsThe proposed solution is in line with VBHC principles, as it improves efficiency and care delivery while optimizing costs. Simulation was an effective tool to replicate and explore possible changes. Multicriteria modeling proved to be a useful approach for a transparent prioritization and redesign of improvements in the healthcare sector.
Os laboratórios de hemodinâmica são comummente projetados para alcançar os melhores resultados clínicos de forma eficiente. Este estudo desenvolve métodos que visam apoiar gestores da saúde a analisar o valor acrescentado da implementação de medidas de melhoria, segundo uma estrutura de saúde baseada em valor.
MétodosTendo por base uma abordagem sociotécnica, os métodos aplicados visam aumentar a eficiência, reduzir a duplicação de tarefas, diminuir custos e melhorar o atendimento ao paciente, ao mesmo tempo tornando a tomada de decisões mais inclusiva e clara. No seguimento do processo de construção de um modelo multicritério, foram organizadas reuniões, entrevistas e uma conferência de decisão. Em paralelo, foi construído um modelo de simulação de eventos discretos (DES) para replicar o atual fluxo de pacientes e atividades e reproduzir o impacto da implementação de medidas de melhoria e variações nos recursos humanos.
ResultadosForam considerados quatro critérios de avaliação para melhoria do fluxo de trabalhos: contribuição para a eficiência do processo de admissão, para o cumprimento de horários, para a agilidade entre procedimentos e para a formação dos recursos humanos. As medidas de melhoria desenhadas procuraram: 1) melhorar o início da atividade diária, 2) melhorar a avaliação pré-exame, e 3) melhorar a formação do staff. Os resultados priorizam a «Medida 2» e demonstram que a melhoria da alocação de recursos humanos aumenta a eficiência e resulta em reduções significativas nos custos.
ConclusõesA solução proposta está em linha com os princípios da saúde baseados em valor, pois melhora a eficiência e a prestação de cuidados, ao mesmo tempo que otimiza os custos. A simulação foi uma ferramenta eficaz para replicar e explorar possíveis mudanças. O modelo multicritério provou ser uma abordagem útil para uma priorização transparente e para o desenho de melhorias no setor da saúde.
Quality and excellence come as a priority in any healthcare organization. In recent years, countries have become increasingly concerned about aligning their health systems with value-based healthcare (VBHC) approaches. This stems from the belief that VBHC helps healthcare providers optimize costs, make the best use of finite resources, and deliver improved care to patients.1
The daily pressure on healthcare managers to improve quality and control costs, forces them to look for further efficiency gain,2 while improving patient experience and health outcomes. Obtaining these gains usually implies organizational changes that must be analyzed and understood rationally and transparently. However, the implementation of such changes faces resistance from the workforce, which turns it into a challenge.3
When it comes to cardiac catheterization laboratories (Cath Labs), these deal with high-pressure situations on a daily basis,4 and the Cath Lab at Hospital do Espírito Santo de Évora (HESE) is no exception. The volume and underlying complexity surrounding the cases, the multidisciplinarity and magnitude of the team inside the Cath room, the use of advanced and continuously evolving technologies, and the coordination and precision required to perform cardiac catheterizations, make cath labs hard units to manage.5
The Cath Lab at HESE was inaugurated in June 2009, with one cath room, which sought to meet the needs of interventional cardiology in the Alentejo region.6 From 2009 to 2019, the percentage of deaths due to cardiovascular diseases in Portugal decreased from 31.9% to 29.9% and, like most of the regions in Portugal, the Alentejo accompanied the national trend with a decrease from 33.9% to 30.8% deaths due to cardiovascular diseases.7
In 2019, to meet the increasing population needs, the Cath Lab was included as part of an organizational middle management structure called Center for Integrated Responsibility (CRIA - Centro de Responsabilidade Integrada Cérebro-Cardiovascular do Alentejo), created with the objective of providing differentiated and quality healthcare for brain-cardiovascular-related diseases. CRIA, as a multidisciplinary unit, involves the areas of Interventional Cardiology, Interventional Nephrology, Vascular Surgery, Neuroradiology, and Interventional Radiology, where currently 60% of the time it is used for interventional cardiology.6 The structure and goals of CRIA are aligned with a VBHC management strategy that calls for leadership not just at the top management level, but also at a clinical level and therefore our methodology makes use of participatory methods involving all team members.8
The Center for Integrated Responsibility aims to guarantee there are high standards of technical-scientific performance and humanization of health activities, promoting effective and efficient financial and human resources management, with fair remuneration and professional training of its employees. The organizational model, guided by key performance indicators (KPI), recognizes and rewards individual and collective performance.9
The Center for Integrated Responsibility's mission and vision is itself a step toward a VBHC-oriented system as it works to i) ensure the development of best clinical practices focused on the users’ needs, ii) foster clinical governance processes that contribute to the continuous improvement of the quality of care provided, iii) promote the autonomy, involvement, and accountability of professionals regarding resource management, and iv) increase the levels of productivity and satisfaction of in the national health system professionals, among other.9
Since 2020, CRIA has had two cath rooms that operate 12 hours a day, from 8 am to 8 pm, on weekdays, and also in a permanent prevention regimen for acute myocardial infarction emergencies. The first cath room is dedicated mainly to the performance of coronary angiographies and angioplasties, while the second serves the other previously mentioned areas. In this paper, we aim to inform and support CRIA management in the analysis and evaluation of improvement measures in order to enhance operational efficiency, while studying the possibility of operating two Cath rooms without doubling CRIA operational team costs. These analyses make use of methods designed to involve CRIA stakeholders and its workforce, to simulate its operations, and to assess the value of improvement measures.
Material and methodsImproving clinical pathways and measuring improvements’ valueThe methods used for understanding and valuing clinical pathway improvements followed a sociotechnical approach3 which combines sound techniques and participatory processes. While simulation and multicriteria modeling techniques were used to analyze and evaluate the impacts of adopting implementation measures, designed participatory processes were selected to increase communication within the organization. These ensure that the concerns and values of the people who know the system best and who are directly related to management decisions are considered.
Involving participants with different responsibilities and professional qualifications in the modeling processes allowed them to contribute with their knowledge and diversity views regarding the systems’ efficiency.3,10 Other advantages from adequate participation include developing a shared understanding of issues within multidisciplinary groups, as well as generating a sense of common purpose, commitment to future changes, and confidence in the models’ results.3
The adopted methodology was implemented in three phases.
Phase 1Starting with the AS-IS analysis, which is aimed at defining and assessing the current state of the Cath Lab clinical pathways to clarify exactly how CRIA workflow processes work, flaws and all, the on-site observation enabled mapping of patients’ clinical pathway in CRIA and information collection on the main steps and procedures applied during the care process, resources associated with them, and critical points that most influence efficiency (as recommended by Karnon et al. (2012)11). Besides that, interviews with CRIA team members, from all positions and levels of responsibility, were used to understand their perspectives and experiences and to assess their knowledge about the clinical pathway and workflows (following the views of Nilsson and Sandoff (2017)8). In parallel, group meetings with hospital administrators, boards of directors, and the coordinator of the interventional cardiology, referred to as stakeholders, helped identify the short-term objectives of CRIA.
From here, one could induce the main challenges to efficiency and hence define, together with stakeholders, a valid set of criteria to evaluate efficiency in CRIA, operationalized through performance descriptors.12 Bana e Costa and Beinat (2005)13 define a performance descriptor as ‘a measure of the extent to which the criterion can be satisfied, from a most attractive to a least attractive level of performance’, that is an ordered set of plausible levels of performance. A performance descriptor can be a quantitative indicator or a qualitative scale3 and enables a further understanding of the impact of improvement measures in CRIA.
For each of the descriptors, reference levels of performance are used as anchors for weighting. Reference levels can be denominated using different terms,14 although ‘GOOD’ and ‘NEUTRAL’ were considered more suitable for this study. ‘GOOD’ corresponds to a level that has an unquestionably attractive benefit and should be looked to as a ‘goal’ which, when achieved, indicates there is no improvement needed in the respective criterion. ‘NEUTRAL’ is neither attractive nor unattractive, in terms of need for improvement, but a minimally satisfactory level that can surely be improved.15
After setting evaluation criteria and descriptors of performance, one should then link these with the clinical pathway data and KPI information collected from the AS-IS analysis.
Phase 2At a decision conference,3 all the CRIA team members and stakeholders were assembled to perform an on-the-spot construction of a multicriteria value model to evaluate plausible improvements in the previously defined criteria.16 This work session envisioned the construction of collective judgments, agreed upon by the group of participants. By promoting the exchange of points of view (enabled by computer-aided technologies), the decision conference helped to create a solid understanding about the value of improvement measures.
Following the MACBETH technique,17,18 participants evaluated differences in attractiveness between possible improvements,19 through a simple and intuitive protocol of questions using a seven-category scale of qualitative difference of attractiveness, referred to as qualitative judgments: null, very weak, weak, moderate, strong, very strong and extreme.
For each criterion, there was a group of questions, all structured the same way, regarding the comparison between each performance level and the least attractive one and between each consecutive pair of performance levels. In each question, participants were asked to give a judgment that would complete the sentence ‘For the improvement of the efficiency in the Cath Lab workflow [proposed improvement measure] is of [MACBETH scale judgment] importance’. For example, ‘For the improvement of the efficiency in the Cath Lab workflow [going from a delay of 40 to 0 minutes] is of [extreme] importance’. Participants first gave individual answers and then, concertedly, a collective MACBETH judgment was defined. It was important to listen and to understand the justification of non-majority judgments and strive to reach a consensus that included all participants’ standpoints. Once all collective judgments were agreed upon, value scales were built using the MACBETH approach to quantify the attractiveness of improving performance within each criterion and adjusted and validated by the group.
The next part of the decision conference consisted of posing questions about the overall attractiveness; that is, considering all the descriptors in the ‘NEUTRAL’ level, participants were asked to rank the improvements to the ‘GOOD’ level according to attractiveness (see Appendix A). The next and final step involved qualitatively judging the differences of attractiveness between these same levels again, according to the MACBETH scale, first independently and then collectively. The collective qualitative weighting judgments were finally converted into numerical weighting.
The MACBETH technique was implemented with the help of the decision support software M-MACBETH.20 This software allows the construction of a value tree, which gives a visual overview of the previously defined concerns, criteria, and descriptors, organized hierarchically,13 and the conversion of qualitative judgments into value scales (which are subject to discussion, adjustment and validation by the group).17,18
It is important to note that to build an additive value model, one must ensure preference independence between criteria, that is, the evaluation of the performance of a criterion should not depend on the performance of other criteria;21 and that the model was subject to sensitivity and robustness analyses.17,18
Then, a discrete-event simulation (DES) model22 of CRIA was built, with the support of Simul8 software,23 to capture CRIA patient flow and activities and reproduce, in advance, the operational impact of any improvement measures, which could then be evaluated with the multicriteria model.
Alternative managerial implementation measures focusing on the objectives of CRIA were designed in close collaboration with stakeholders during workgroup sessions and then replicated in the DES model (following Goienetxea Uriarte (2017)24).
Phase 3In a meeting with the main stakeholders, the defined implementation measures were simulated to reproduce their operational impact on CRIA workflow, when only one Cath room was functioning. The impacts of each of the improvement measures could then be evaluated with the multicriteria model, built earlier with M-MACBETH, to conclude to which degree one measure had a higher overall value than another,25 considering the perspectives and opinions of decision conference participants. The suggested improvements were recognized by CRIA stakeholders as a valid approach to help them achieve their goals.
Improving the allocation of human resourcesThe simulation model was then updated to depict a new layout of CRIA with two operational cath rooms. This new model aimed at reproducing variations in the number of human resources allocated to the different tasks within CRIA workflow, to test whether human resources needed to be doubled to achieve the same efficiency results as with one Cath room and, if not, what would the required number of human resources be. In a meeting with stakeholders, the number of human resources to be tested in the simulation model was discussed. Furthermore, cost savings were calculated to determine the financial impact of such changes.
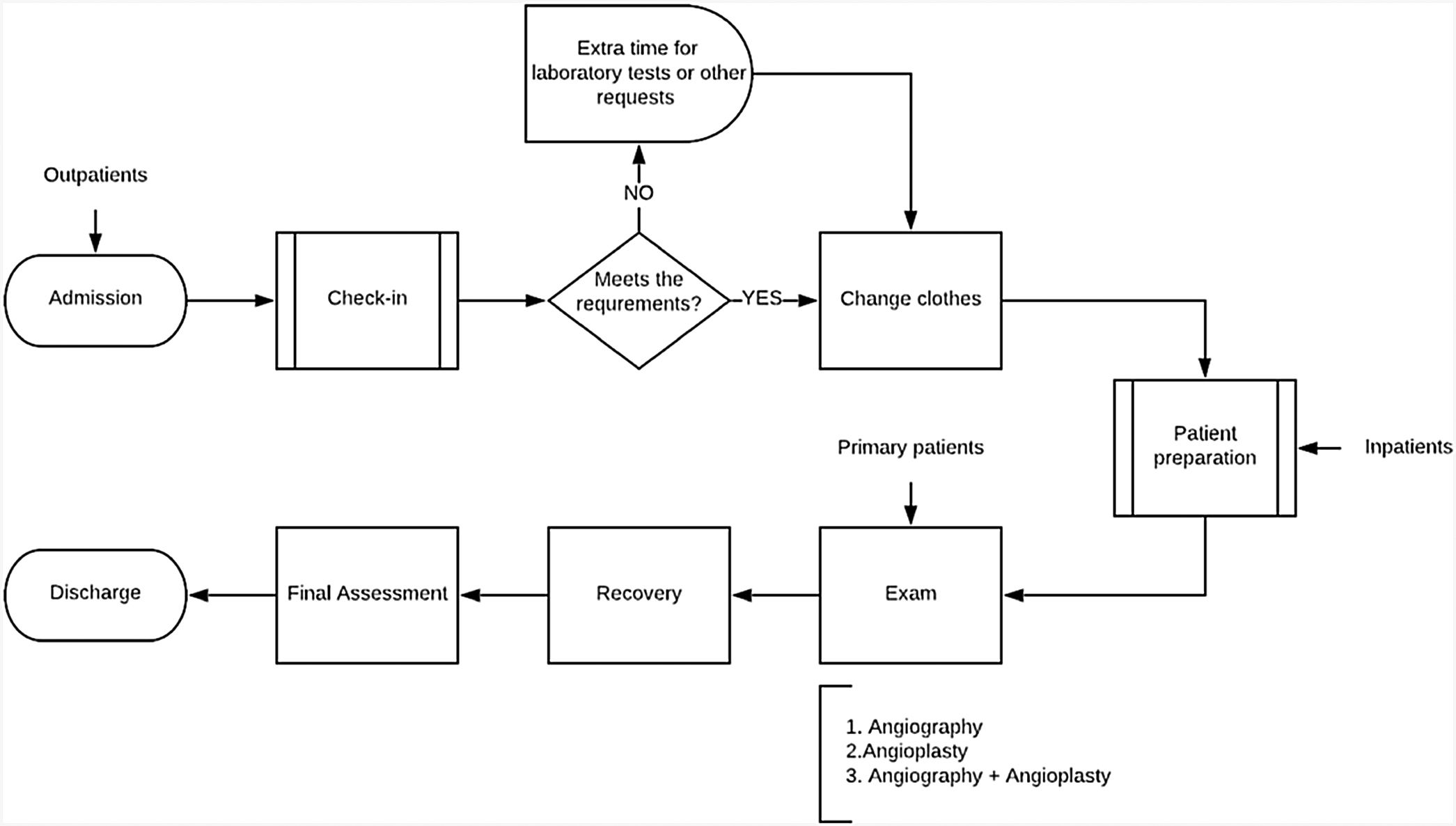
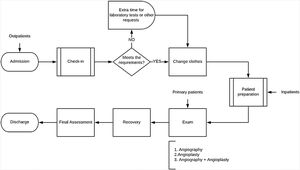
ResultsImproving clinical pathway and measuring the value of improvementsPhase 1From the AS-IS analysis, a detailed mapping of the CRIA clinical pathway, illustrated in Figure 1, was created. This map helped identify the performance indicators that were sources of operational inefficiencies related to medical service delivery, logistics, or administrative services.26
After the initial interviews with CRIA team members and group meetings with stakeholders, it was clear that the main goal for CRIA is to become a reference cardiology center, capable of meeting cardiological needs in the Alentejo region, under a VBHC model. These interactions also helped diagnose some of CRIA's main challenges: i) limited pre-exam assessment, ii) restricted external referral, iii) high load of administrative tasks, and iv) lack of human resources.
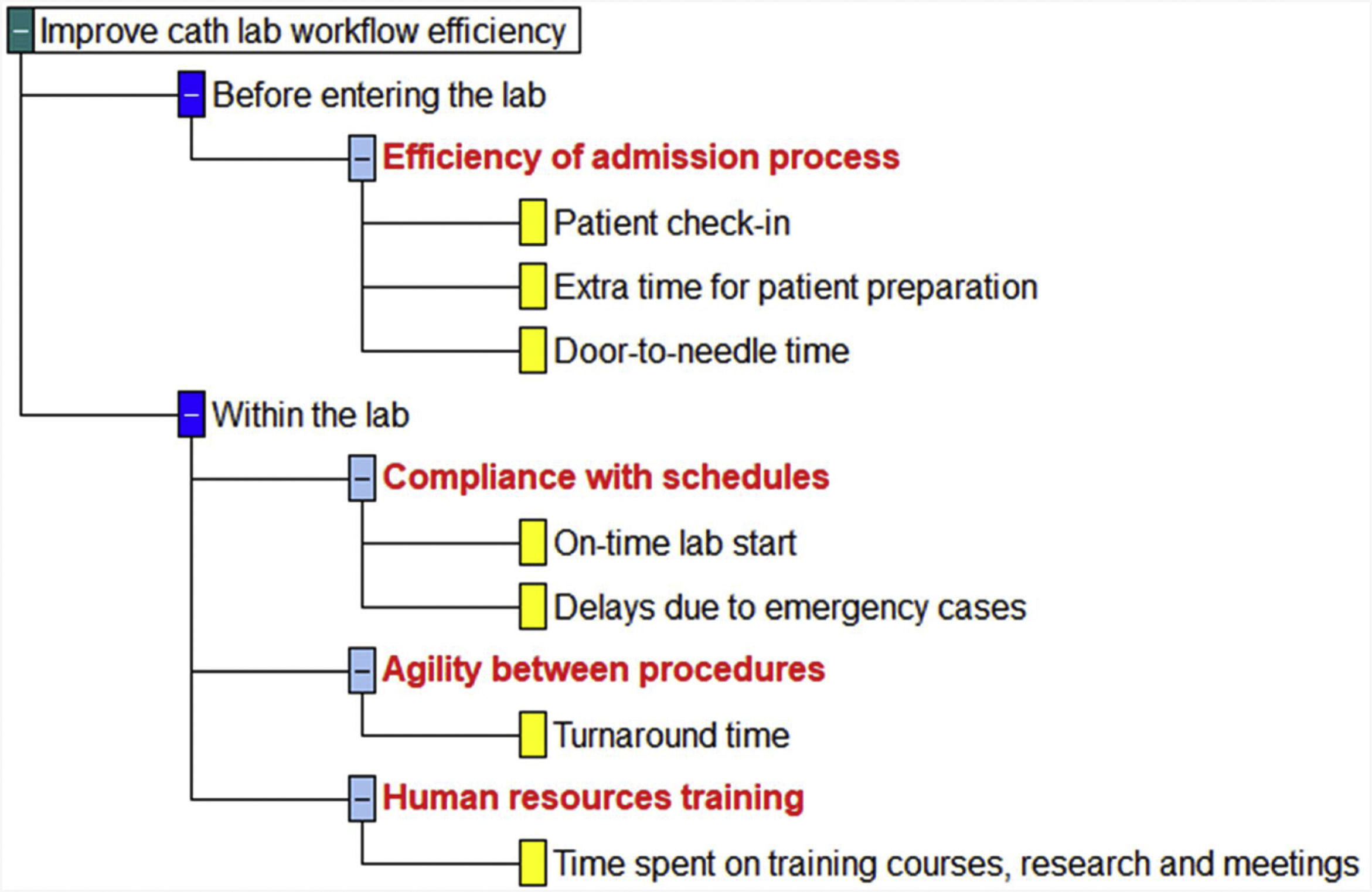
Considering the outputs of the AS-IS analysis, we defined the following set of evaluation criteria together with the stakeholders:
- 1.
Efficiency of admission process: Improve the time it takes from check-in to the beginning of the procedure, considering any extra time needed for patient preparation.
- 2.
Compliance with schedules: Improve the punctuality of CRIA in the first procedure of the day, considering that it should start at 8:30 am (0 minutes delay).
- 3.
Agility between procedures: Improve the efficiency related to turnaround times, which correspond to the average duration from the conclusion of a procedure (hemostasis) to the beginning of the next scheduled one.
- 4.
Human resources training: Improve the capacity of the available human resources by promoting weekly training courses.
The next step consisted in associating performance descriptors with the criteria that had now been validated by stakeholders. The performance descriptors were structured through several equally spaced reference levels of performance in each criterion (see Appendix A for more detail). Since the performance descriptors are seen as the objective portion of the model, they were built to be sources of unambiguous factual information for the drawing up of value judgments (following good practice adopted in Bana e Costa et al. (2012)14).
For each criterion, two reference levels were defined, GOOD’ and ‘NEUTRAL’. ‘GOOD’ was set as a target performance level for the lab, based on what managers envisaged and considering exemplary performances from other Cath Labs. ‘NEUTRAL’ was set as the status quo, in other words, the current state of the Cath Lab in that criterion based on previously provided data (see Table A2 in Appendix A).
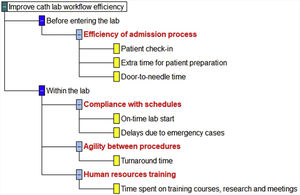
The structuring of the decision model resulted in a value tree (Figure 2), built with the support of M-MACBETH. Hierarchically, the tree starts with the two areas of concern, passing through the criteria and ending with the performance indicators.
Phase 2The decision conference gathered 17 on-site professionals, including cardiologists, nurses, cardiopneumology technicians, radiology technicians, operational assistants, and hospital managers. In the room, there was also a facilitator guiding the group throughout the conference and a decision analyst giving support and using the M-MACBETH program. For three hours, participants questioned, discussed, and constructively contributed to the evaluation of possible improvement measures. The room layout respected the one suggested by Bana e Costa et al. (2014),27 with all participants maintaining eye-to-eye contact and direct visual access to two displays, one projecting the M-MACBETH software and the other displaying the decision conference protocol questions and corresponding results from individual and collective judgments.
‘Agility between procedures’ was the criterion on which participants collectively agreed that an improvement from the current average turnaround time of 35 minutes (deemed as a neutral performance) to a turnaround time of 20 minutes (deemed as a good performance) would have the greatest impact on the efficiency of CRIA workflow, therefore obtaining the highest weighting (0.36), followed by ‘Efficiency of admission process’ (0.29), ‘Compliance with schedules’ (0.19) and ‘Human resources training’ (0.16).
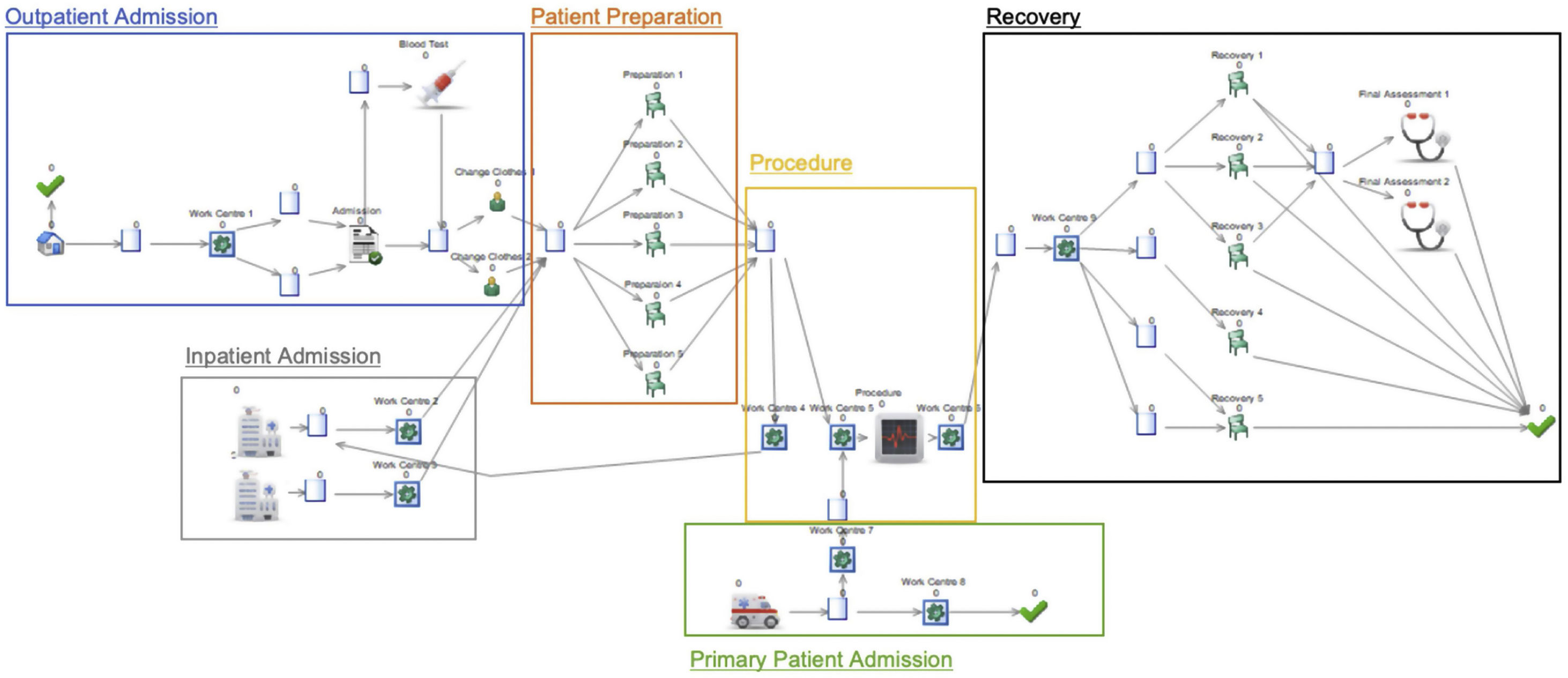
The next stage was to develop the computational model representing the configuration of CRIA, according to the patient workflow depicted in Figure 1. In the simulation layout, detailed in Appendix B, one could emphasize six main processes: i) Outpatient Admission; ii) Inpatient Admission; iii) Preparation; iv) Primary Patient Admission; v) Procedure; vi) and Recovery. Regarding input parameters, the simulation model contemplates several variables that include the percentage of rescheduled outpatients, percentage of patients that need blood tests, nurse availability, administrative assistant availability, average turnaround time, and time spent weekly on training. These variables change when testing alternative improvement measures.
The following three alternative improvement measures were designed and simulated using the developed model:
Measure 1 – Improve the start-up of the day
This measure focused on improving the start-up of the day by hiring a full-time administrative assistant (from 8 am to 3 pm) to assure that check-in was not performed by a nurse and by applying some changes in daily management and scheduling. The latter included starting the day with an inpatient to guarantee that a patient was ready to start the procedure at 8:30 am since, with these patients, one can ensure a proper and timely pre-exam preparation. Also, two outpatients were scheduled at 8 am and two at 10 am instead of four at 8am, so that the nurses would only have to prepare two patients at a time and consequently, patients would spend less time at the Cath lab.
This improvement was simulated and associated with an enhancement of the current average turnaround times of about 32.4% to an average of 25 minutes, and of the first procedure of the day of about 22.9%, starting on average at 8:57 am.
Measure 2 – Improve pre-exam assessment
‘Measure 2’ intended to enhance efficiency by preventing and decreasing the number of delays caused by inadequate pre-exam preparation. Consequently, it consisted of i) having a full-time administrative assistant that would conduct the confirmation call, following a well-structured script with a checklist for patients with no special needs and, ii) a nurse doing the confirmation calls to patients with special needs (e.g., elderly people) or, if necessary, onsite appointments to guarantee full compliance with requirements and proper pre-exam preparation.
It was also important to allocate some time for staff training to understand what the core exam requirements are and how to check them. In the simulation model, these changes improved turnaround time by 51.4%, to around 18 minutes, and the start of the first procedure of the day by 17.1%, which would start around 8:59 am.
Measure 3 – Improve staff training
The third improvement was a soft approach to all the short-term targets of CRIA and included a weekly 90 minute training session dedicated to workshops, research, teambuilding activities, or feedback sessions to enhance team capabilities. This measure aimed at improving cross-over for some tasks between different professionals and as intended, simulation results showed an improvement in the turnaround time of 43.2%, which corresponds to an average of 21 minutes. Moreover, this measure proposed treating inpatients first, as highlighted in ‘Measure 1’, to enhance the daily start-up. This resulted in the first procedure of the day starting approximately at 8:51 am, an enhancement of 40%, according to the simulation model.
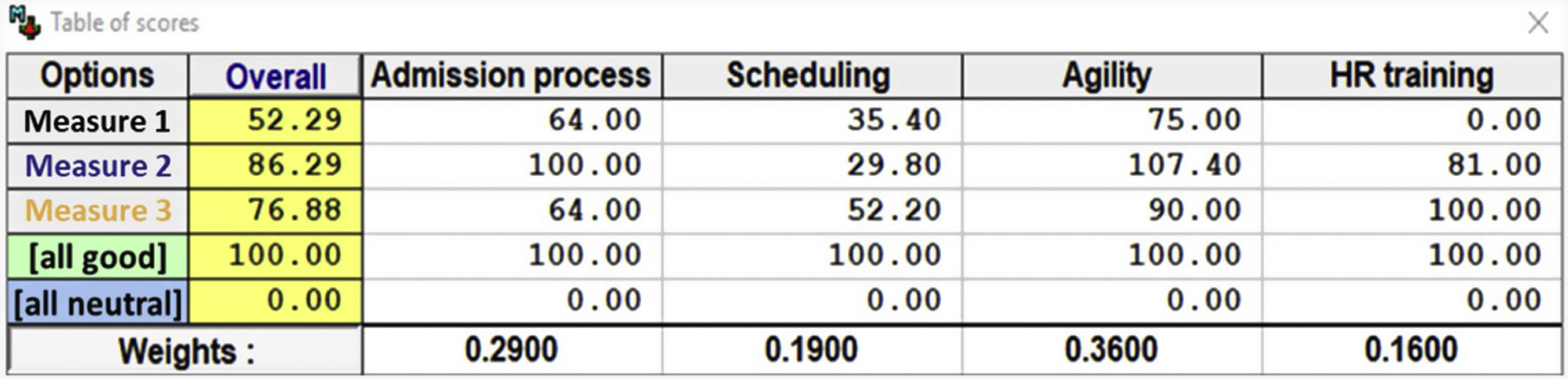
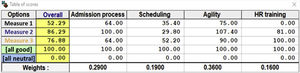
Phase 3The performance of CRIA against each of the measures (see Appendix C) was converted into value scores25 with the support of M-MACBETH. From the sum of the scores of an improvement in each weighted criteria, an overall score for that improvement could be calculated, as presented in Figure 3. ‘Measure 2’ had the best overall score, followed by ‘Measure 3’ and ‘Measure 1’. This means that ‘Measure 2’ adds more value to CRIA efficiency and should be the first to be implemented, considering the short-term objectives of CRIA. Thus, improved turnaround times and greater investment in pre-exam assessment and preparation should be the next steps.
Table of scores, obtained with M-MACBETH support, of the proposed improvement measures (in the M-MACBETH DSS20).
The next stage of the study comprised an analysis of how to improve human resources allocation. In the simulation model, following the implementation of ‘Measure 2’, a second cath room was added to the CRIA layout. As the initial simulation model showed, and CRIA stakeholders confirmed, not all human resources were being 100% utilized during working hours. Initially, the CRIA team comprised three cardiologists, two cardiopneumology technicians, two nurses, one radiology technician, and one operational assistant per shift. CRIA stakeholders suggested conducting a simulation of the impact, in this new layout, of only adding to the team a full-time administrative assistant, a cardiopneumology technician, a nurse, and an operational assistant. This model enabled an assessment of whether CRIA would obtain the same efficiency outcomes by increasing human resource capacity by only 44.4%.
Results from simulation showed that, with this team, CRIA would still be able to perform 18 minute turnaround times, which is close to the value proposed in the literature.26 Moreover, the first procedure of the day would start around 8:48 am (on average), which is, thus far, the closest value to the target of 8:30 am and signifies an improvement of 48.6% in relation to the existing system.
Regarding cost savings, the rationalization of human resources represents a total of annual savings per shift of approximately 68498 euros, when compared to the costs of simply doubling personnel. Considering that there are two daily shifts, the total annual savings amount to 136996 euros, as described in Table 1.
Estimate of annual costs and savings on the new CRIA team after implementation of measures.
| Human Resourcesp/shift | Before model | After model | D | Annual salary | Annual saving | Total annual saving (2 shifts) |
|---|---|---|---|---|---|---|
| Nurses | 4 | 3 | -1 | 22 833 € | -22 833 € | -45 666 € |
| Cardio-pneumology technicians | 4 | 3 | -1 | 22 833 € | -22 833 € | -45 666 € |
| Radiology technician | 2 | 1 | -1 | 22 833 € | -22 833 € | -45 666 € |
| Operational assistant | 2 | 2 | 0 | 12 913 € | 0 € | 0 € |
| Administrative assistant | 1 | 1 | 0 | 13 765 € | 0 € | 0 € |
| 13 | 10.0 | -3 | -68,498 € | -136 998 € |
The method used was grounded in sociotechnical approaches, which means that each of its technical components had a strong associated social element and on which it was heavily dependent. This is aligned with the recommendation of a recent review performed by Oliveira et al. (2019)10 that states the need for developing and enhancing participative methods for evaluating health technologies, processes and programs (for instance, we adopted interacting voting procedures to build consensus in the decision conferences). Moreover, Monks et al. (2012),28 on the use of Simul8, defend that “modeling alone is not enough to achieve change within healthcare systems” and therefore appeals to the inclusion of stakeholders and workflow key players to reach an agreement on the forward actions to take. That being said, the focus on enhancing the willingness and confidence of stakeholders and CRIA was also relevant given the resistance that the implementation of new organizational measures usually faces.
The success of the multicriteria evaluation was mainly due to the decision conference, an organized workshop that was valued by most participants, who actively and constructively participated in the evaluation of different improvement measures. A fundamental step in this stage was a clear explanation and exemplification of the technique employed and of how criteria should be considered. Participants were very aligned with the value focus thinking principles29 and most of the time voted on prioritizing impact on efficiency, rather than what was more important to them. As found in Oliveira et al. (2012) this model proved to be useful for a transparent prioritization and redesign of interventions in the healthcare sector.15
Regarding simulation, it proved to be an effective tool to replicate and explore possible changes in the healthcare sector. The fact that DES enabled the efficiency evaluation of the existing system, to ask ‘what if?’ questions, and to redesign system operational workflow, made it an appealing method for analysis and research modeling. Moreover, DES could be used as a predicting tool to reproduce and assess the impact of implementation measures on the clinical pathway and to study staffing levels, physical capacity, and complex relationships among different system variables,30 which was found by Brenner et al. (2010).31
After reproducing the operational impact of the three designed implementation measures, the simulation demonstrated that ‘Measure 2’ and ‘Measure 3’ were good options with positive effects in the areas of interest. Although only after converting the performance of CRIA into scores, with the support of the multicriteria model, were stakeholders able to decide which measure should be applied first, considering both the performance of the system and the value added to efficiency in Cath Lab workflow, which in this case was ‘Measure 2’. Once again the thesis put forward by Monks et al. (2012)28thesis was confirmed, as simulation on its own was insufficient to make a substantiated decision.
Overall, the results support the prioritization of an improvement measure that invested in the efficiency of the admission process, even before the arrival of the patient to CRIA, which in turn avoids any delays caused by inadequate pre-exam assessment and preparation. With that aim, a proposal was made for a full-time administrative assistant who performs a confirmation call following a well-structured script with a checklist. For patients with specific conditions, or with special needs, it was proposed that a nurse conduct the confirmation call or, if needed, an onsite appointment to guarantee compliance with requirements. The assistant would also be responsible for check-ins and, therefore allowing nurses to spend those 7–8 minutes preparing the cath room for incoming patients. This measure suggests that it is important to dedicate some time to training, especially to learn about the core exam requirements and how to check them.
Focusing on ‘agility between procedures’ – the number one criterion in the multicriteria evaluation – an improvement to 18 minutes is recommended, which results from a proper allocation of responsibilities among team members,26 an increase in the cross-over of some tasks between different professionals, and better communication skills. This might also be facilitated by training and workgroup sessions (up to one hour a week) which, besides fostering the teams’ sense of common purpose, support the streamlining of tasks, without compromising operational efficiency, as shown by the simulation results. Since agility between procedures impacts all patients throughout the day, and if CRIA achieves the proposed time reduction (around 19 minutes between interventions, as suggested by ‘Measure 2’), it is expected that CRIA will be able to assist an additional one or maybe two patients every day. This increment would allow a shorter guaranteed maximum response time for non-urgent patients, which is currently 120 days after medical recommendation,32 although 30 consecutive days after medical recommendation33 is the suggested period. While the potential financial impact of such an improvement was not studied, a better response in a shorter timeframe is a step closer to CRIA becoming a reference site for cardiovascular care.
Improving human resource allocation, more than increasing efficiency, offers significant cost savings. The second simulation model showed that with two Cath rooms functioning, CRIA only needed to increase human resources capacity by 44.4% to obtain the same operational performance; at the start-up of the day even better results were obtained. Improved human resources allocation represents annual cost savings of around 136996 euros when compared to a scenario where human resources are simply doubled. Therefore, when operating with two Cath rooms, CRIA should add a full-time administrative assistant, a cardiopneumology technician, a nurse, and an operational assistant to the team.
To assess and ensure the proper implementation of the proposed measures, regular meetings and contact with stakeholders should take place, guaranteeing that these become part of CRIA daily activity, without sidelining staff experience throughout the process.
The proposed solution is in line with VBHC principles, where high spending does not necessarily equate to the delivery of better healthcare. Through an integrated approach, the applied methods produced clear efficiencies, reduced duplication of tasks, cut costs, and improved patient care,1 while making the decision process more inclusive and trusting.34 The feedback relative to the social component was astonishing and, in addition, the technical component also yielded viable results that were useful to support board members in strategy management.
Study limitationsThere are still plenty of aspects that need to be improved to make this approach more embracing and reusable. In further applications, more criteria (going beyond the adopted efficiency concept) and alternative measures should be integrated and generated. It is important to stress that difficulties during the implementation stage arose due to the need to use two distinct software tools. Furthermore, this study does not cover the operational and financial impact that the proposed changes might have on the hospital's other services, due to the increase in patients and consequent staff workload.
ConclusionsThe results of this study show the relevance of promoting the discussion and exchange of perspectives between management and team members about priorities and actions going forward. The adopted participatory processes promoted improvement even during model building by creating a sense of common purpose and allowing CRIA team members to participate in the VBHC management strategy and improvement of the system.
Improving clinical pathways can be achieved through the implementation of the following measures: 1) ‘Improving the start-up of the day’, 2) ‘Improving the pre-exam assessment’, and 3) ‘Improving staff training’. Results show that the second measure, which encourages better turnaround times and greater investment in pre-exam assessment and preparation, adds more value to CRIA efficiency.
Improving human resources allocation might allow CRIA to obtain annual cost savings up to 136996 euros, compared to the costs of doubling the team once operational with two Cath rooms. Further studies could explore the financial impact that improving clinical pathways and human resource allocation would have on other hospital services/departments.
In conclusion, the methods developed and implemented through VBHC guidelines provide insights into how best to use finite resources, while simultaneously guaranteeing higher quality, efficient care. Overall, the study revealed strategies to mitigate barriers in the implementation of changes in a healthcare unit. The identified evaluation criteria demonstrate CRIA's excellence and great concern for staff and patient experience, two of the main features that will help it become a reference center led by VBHC principles.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank HESE for all the data provided and, especially the CRIA team for the contribution and availability. Funding Mónica Oliveira work was supported by the Portuguese Foundation for Science and Technology under the MEDI-VALUE project (Grant no. PTDC/EGE-OGE/29699/2017). The first and second authors acknowledge support from the Center for Management Studies of Instituto Superior Técnico (CEG-IST), a research centre funded by FCT project UIDB/00097/2020.
See Tables A1 and A2.
List of the key performance indicators summarized according to the four criteria and the metrics for their measurement.
| Criterion | KPIs associated | KPI definition | Metrics for calculation |
|---|---|---|---|
| 1. Efficiency of admission process | Patient check-in duration | Time taken for the process of registering the patient, usually performed by a nurse. | Patient arrival timePreparation time |
| Extra time for patient preparation | Time taken for the patient be in the right conditions to do the exam in case fasting was not properly made or if there is the need of doing blood tests. | Preparation time | |
| Waiting time (outpatients) | Time since the patient arrives until the procedure begins. | Patient arrival timeProcedure start time | |
| 2. Compliance with schedules | On-time lab start | Difference between scheduled time and actual start time of the first procedure of the day. | Procedure start time |
| Delays due to emergency cases | Delays due to the occurrence of emergency cases (primary exams). | Number of emergency cases | |
| 3. Agility between procedures | Turnaround time | Duration between the exit of the preceding patient and the arrival of the next scheduled one. | Procedure start timeProcedure end time |
| 4. Human resources training | Time spent on training courses, research and meetings | Time invested in activities to develop the team's capabilities. | Time spent on other tasks |
List of the four evaluation criteria and respective descriptors of performance. Each performance descriptor has the ‘GOOD’ and ‘NEUTRAL’ levels identified.
| Criterion | Performance descriptor |
|---|---|
| 1. Efficiency of admission process | 1. Have an administrative fully dedicated to CRIA (calls and check-in) and a nurse doing pre-exam assessment GOOD |
| 2. Have an administrative fully dedicated to CRIA (calls and check-in) and no nurse doing pre-exam assessment (patient assessment right before the exam) | |
| 3. No administrative fully dedicated to CRIA but a nurse doing pre-exam assessment | |
| 4. No administrative fully dedicated to CRIA and no nurse doing pre-exam assessment (patient assessment right before the exam) NEUTRAL | |
| 2. Compliance with schedules | 1. 0 minutes GOOD |
| 2. 10 minutes | |
| 3. 20 minutes | |
| 4. 30 minutes | |
| 5. 40 minutes NEUTRAL | |
| 3. Agility between procedures | 1. 10 minutes |
| 2. 20 minutes GOOD | |
| 3. 30 minutes | |
| 4. 40 minutes NEUTRAL | |
| 5. 50 minutes | |
| 4. Human resources training | 1. 120 minutes |
| 2. 90 minutes GOOD | |
| 3. 60 minutes | |
| 4. 30 minutes | |
| 5. 0 minutes NEUTRAL |
See Tables C1 and C2.
Impact of the improvement measures in the efficiency key performance indicators.
| KPIs associated | Existing system | Measure 1 | Measure 2 | Measure 3 | |
|---|---|---|---|---|---|
| 1. Efficiency of admission process | Patient check-in duration | 8 min | 7 min | 7 min | 7 min |
| Extra time for patient preparation | 65 min | 53 min | 42 min | 44 min | |
| Waiting time (outpatients) | 187 min | 125 min | 107 min | 109 min | |
| 2. Compliance with schedules | On-time lab start | 35 min | 27 min | 29 min | 21 min |
| Delays due to emergency cases | 2 cases/month | 2 cases/month | 2 cases/month | 2 cases/month | |
| 3. Agility between procedures | Turnaround time | 37 min | 25 min | 18 min | 22 min |
| 4. Human resources training | Time spent on training courses, research, and meetings | 0 min | 0 min | 60 min | 90 min |